Real-Time VR Enhances View and Treatment Options in IR
|
By MedImaging International staff writers Posted on 05 Apr 2019 |

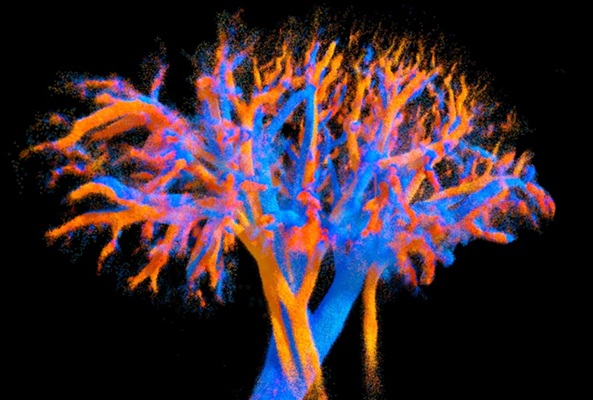
Image: New research suggests virtual reality options could enable interventional radiologists to improve treatments using RT 3D images from inside a patient’s blood vessels (Photo courtesy of Techmaish).
New research presented at the Society of Interventional Radiology’s 2019 Annual Scientific Meeting shows that immersive virtual reality (VR) could enable interventional radiologists to improve treatments using real-time 3D images from inside a patient’s blood vessels. The interactive technology could provide faster, more efficient treatment, with less radiation exposure and greater precision, ease and confidence.
The researchers conducted a study to demonstrate the feasibility of using a catheter with electromagnetic sensors projected onto a VR headset to see and steer the catheter through the anatomy to certain blood vessels. Using a CT angiography scan, they created a 3D printed model and a holographic image of blood vessels in a patient’s abdomen and pelvis. A team of radiologists guided hi-tech catheters through the 3D printed model while the tracking system showed the image from the catheter through the VR headset. They compared the time taken to steer the catheter from the entry point of the femoral artery to three different targeted vessels versus the time the process took using conventional fluoroscopic guidance, as well as the time taken in similar real-life clinical angiographic procedures.
In 18 simulated procedures, the researchers found the mean time to reach the three targeted vessels using VR was much lower than in fluoroscopy, the standard practice that uses an x-ray image. In the first vessel, VR took 17.6 seconds versus 70.3 seconds using the standard practice on the model and 171.2 seconds in the real-life procedure. With the improved efficiency, the researchers believe that VR technology will create safer treatments by reducing the amount of radiation exposure to both patient and physician, as well as increase access to IR treatments. The researchers also surveyed the practitioners who had tried the technology who reported that VR improved the ease, precision and efficiency of the treatment. Additionally, the users said they felt more confident in their abilities.
“Virtual reality will change how we look at a patient’s anatomy during an IR treatment. This technology will allow physicians to travel inside a patient’s body instead of relying solely on 2D, black and white images,” said Wayne Monsky, M.D, PhD, a professor of radiology at the University of Washington and lead author of the study. “Currently, the life-saving potential of IR is limited to hospitals and areas with the resources to invest in image-guided technology. There are three billion people worldwide in rural areas who don't have this access. This technology could allow for portability and accessibility so that these procedures are brought to rural areas using nothing more than a suitcase.”
The researchers conducted a study to demonstrate the feasibility of using a catheter with electromagnetic sensors projected onto a VR headset to see and steer the catheter through the anatomy to certain blood vessels. Using a CT angiography scan, they created a 3D printed model and a holographic image of blood vessels in a patient’s abdomen and pelvis. A team of radiologists guided hi-tech catheters through the 3D printed model while the tracking system showed the image from the catheter through the VR headset. They compared the time taken to steer the catheter from the entry point of the femoral artery to three different targeted vessels versus the time the process took using conventional fluoroscopic guidance, as well as the time taken in similar real-life clinical angiographic procedures.
In 18 simulated procedures, the researchers found the mean time to reach the three targeted vessels using VR was much lower than in fluoroscopy, the standard practice that uses an x-ray image. In the first vessel, VR took 17.6 seconds versus 70.3 seconds using the standard practice on the model and 171.2 seconds in the real-life procedure. With the improved efficiency, the researchers believe that VR technology will create safer treatments by reducing the amount of radiation exposure to both patient and physician, as well as increase access to IR treatments. The researchers also surveyed the practitioners who had tried the technology who reported that VR improved the ease, precision and efficiency of the treatment. Additionally, the users said they felt more confident in their abilities.
“Virtual reality will change how we look at a patient’s anatomy during an IR treatment. This technology will allow physicians to travel inside a patient’s body instead of relying solely on 2D, black and white images,” said Wayne Monsky, M.D, PhD, a professor of radiology at the University of Washington and lead author of the study. “Currently, the life-saving potential of IR is limited to hospitals and areas with the resources to invest in image-guided technology. There are three billion people worldwide in rural areas who don't have this access. This technology could allow for portability and accessibility so that these procedures are brought to rural areas using nothing more than a suitcase.”
Latest Imaging IT News
- New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
- Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
- AI-Based Mammography Triage Software Helps Dramatically Improve Interpretation Process
- Artificial Intelligence (AI) Program Accurately Predicts Lung Cancer Risk from CT Images
- Image Management Platform Streamlines Treatment Plans
- AI-Based Technology for Ultrasound Image Analysis Receives FDA Approval
- AI Technology for Detecting Breast Cancer Receives CE Mark Approval
- Digital Pathology Software Improves Workflow Efficiency
- Patient-Centric Portal Facilitates Direct Imaging Access
- New Workstation Supports Customer-Driven Imaging Workflow
Channels
Radiography
view channel
Routine Mammograms Could Predict Future Cardiovascular Disease in Women
Mammograms are widely used to screen for breast cancer, but they may also contain overlooked clues about cardiovascular health. Calcium deposits in the arteries of the breast signal stiffening blood vessels,... Read more
AI Detects Early Signs of Aging from Chest X-Rays
Chronological age does not always reflect how fast the body is truly aging, and current biological age tests often rely on DNA-based markers that may miss early organ-level decline. Detecting subtle, age-related... Read moreMRI
view channel
MRI Scans Reveal Signature Patterns of Brain Activity to Predict Recovery from TBI
Recovery after traumatic brain injury (TBI) varies widely, with some patients regaining full function while others are left with lasting disabilities. Prognosis is especially difficult to assess in patients... Read more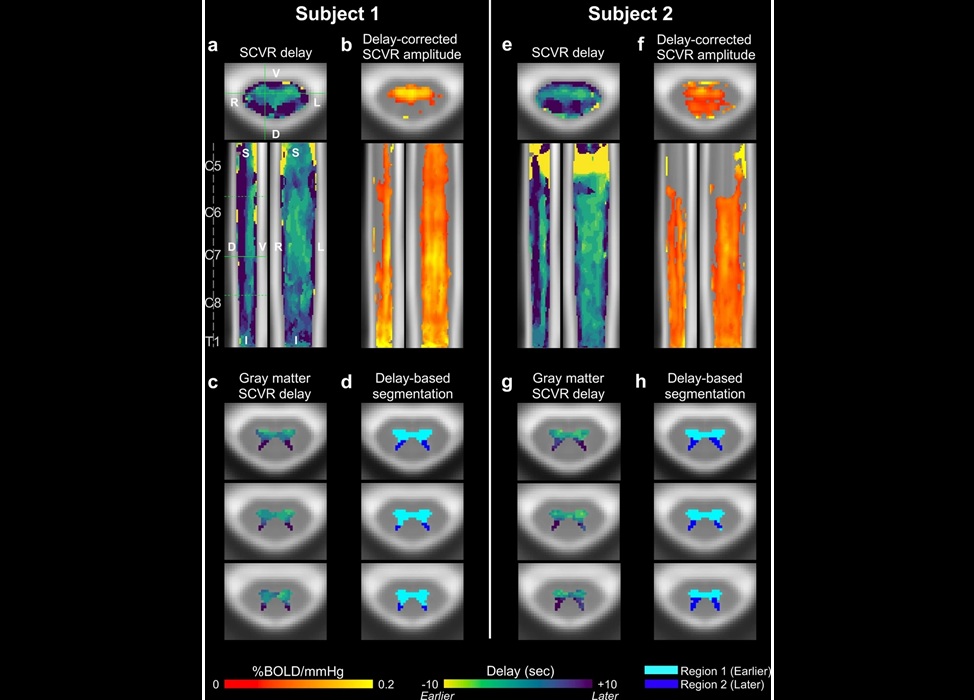
Novel Imaging Approach to Improve Treatment for Spinal Cord Injuries
Vascular dysfunction in the spinal cord contributes to multiple neurological conditions, including traumatic injuries and degenerative cervical myelopathy, where reduced blood flow can lead to progressive... Read more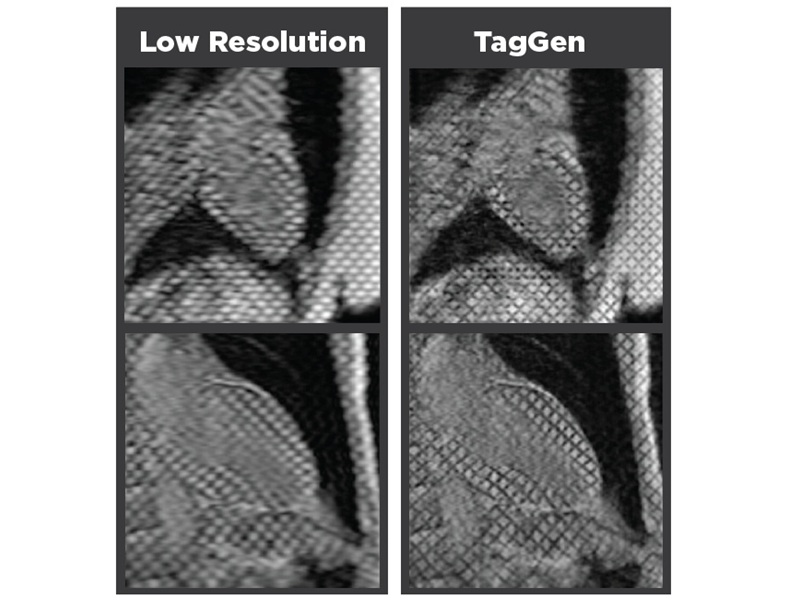
AI-Assisted Model Enhances MRI Heart Scans
A cardiac MRI can reveal critical information about the heart’s function and any abnormalities, but traditional scans take 30 to 90 minutes and often suffer from poor image quality due to patient movement.... Read more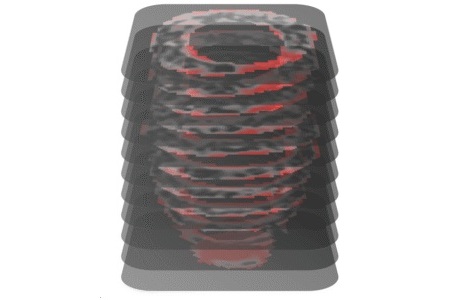
AI Model Outperforms Doctors at Identifying Patients Most At-Risk of Cardiac Arrest
Hypertrophic cardiomyopathy is one of the most common inherited heart conditions and a leading cause of sudden cardiac death in young individuals and athletes. While many patients live normal lives, some... Read moreUltrasound
view channel
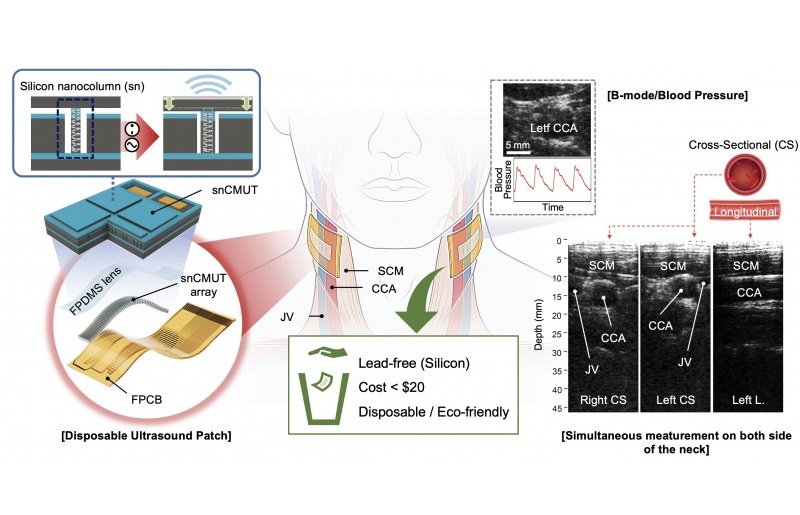
Wearable Ultrasound Imaging System to Enable Real-Time Disease Monitoring
Chronic conditions such as hypertension and heart failure require close monitoring, yet today’s ultrasound imaging is largely confined to hospitals and short, episodic scans. This reactive model limits... Read more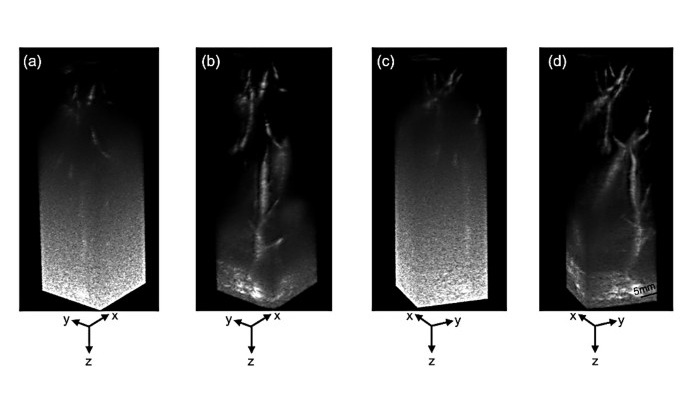
Ultrasound Technique Visualizes Deep Blood Vessels in 3D Without Contrast Agents
Producing clear 3D images of deep blood vessels has long been difficult without relying on contrast agents, CT scans, or MRI. Standard ultrasound typically provides only 2D cross-sections, limiting clinicians’... Read moreNuclear Medicine
view channel
PET Imaging of Inflammation Predicts Recovery and Guides Therapy After Heart Attack
Acute myocardial infarction can trigger lasting heart damage, yet clinicians still lack reliable tools to identify which patients will regain function and which may develop heart failure.... Read more
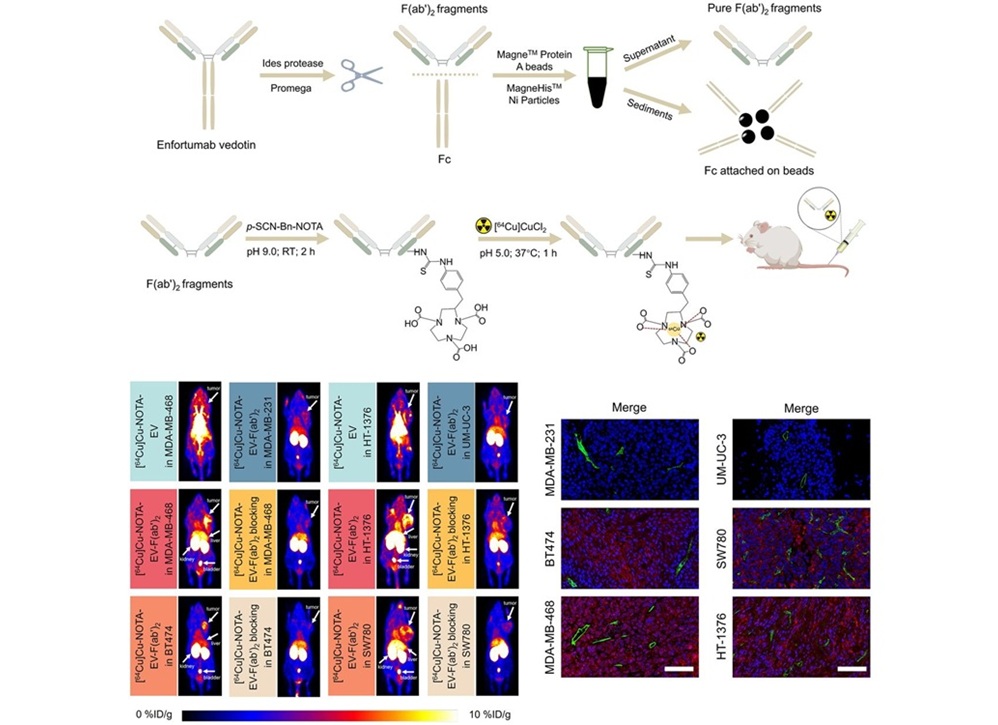
Radiotheranostic Approach Detects, Kills and Reprograms Aggressive Cancers
Aggressive cancers such as osteosarcoma and glioblastoma often resist standard therapies, thrive in hostile tumor environments, and recur despite surgery, radiation, or chemotherapy. These tumors also... Read more
New Imaging Solution Improves Survival for Patients with Recurring Prostate Cancer
Detecting recurrent prostate cancer remains one of the most difficult challenges in oncology, as standard imaging methods such as bone scans and CT scans often fail to accurately locate small or early-stage tumors.... Read moreGeneral/Advanced Imaging
view channel
AI-Based Tool Predicts Future Cardiovascular Events in Angina Patients
Stable coronary artery disease is a common cause of chest pain, yet accurately identifying patients at the highest risk of future heart attacks or death remains difficult. Standard coronary CT scans show... Read more
AI-Based Tool Accelerates Detection of Kidney Cancer
Diagnosing kidney cancer depends on computed tomography scans, often using contrast agents to reveal abnormalities in kidney structure. Tumors are not always searched for deliberately, as many scans are... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more