New MRI Technique Reveals Hidden Heart Issues
Posted on 05 Jun 2025
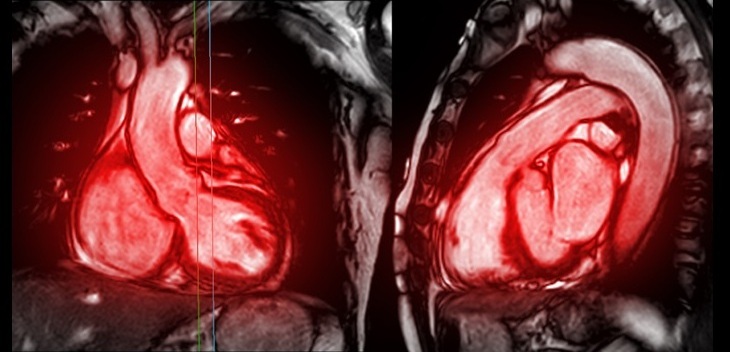
Traditional exercise stress tests conducted within an MRI machine require patients to lie flat, a position that artificially improves heart function by increasing stroke volume due to gravity-driven blood return from the lower body. This makes it difficult for physicians to distinguish between healthy individuals and those with heart disease, creating a diagnostic challenge in assessing true cardiac performance under stress. Researchers have now introduced a new technology: lower body negative-pressure pants that simulate upright posture, providing a more accurate picture of heart function during exercise.
The technology, developed at the University of Texas at Arlington (UTA, Arlington, TX, USA), is the outcome of research focusing on advancing noninvasive methods for exercise-based MRI testing. The patent-pending pants are among several innovations from the group aiming to transform how clinicians evaluate cardiovascular health. The negative-pressure pants function by creating a vacuum around the lower body, drawing blood downward and mimicking the effect of gravity when standing. This counteracts the misleading increase in stroke volume that occurs when lying flat, allowing physicians to observe cardiac performance under more realistic stress conditions. This innovation represents a major leap forward in cardiac imaging, improving the fidelity of exercise-based MRI tests.

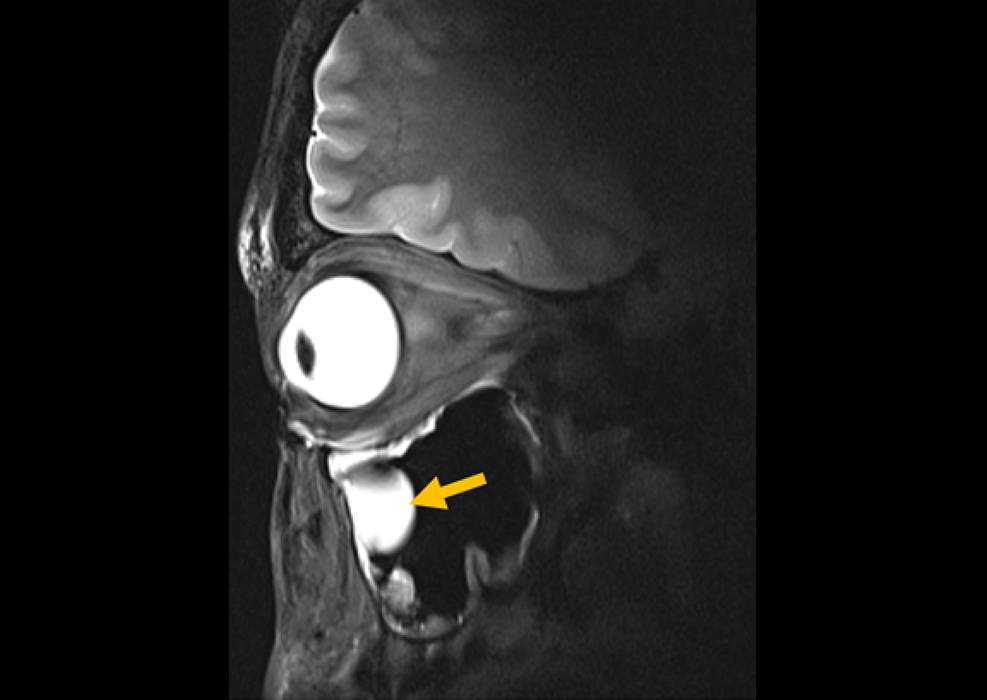
Another advancement from the same team is a novel MRI technique to measure venous oxygen levels without the need for an invasive catheter. In a study published in the American Journal of Physiology, the researchers demonstrated that MRI can accurately assess how much oxygen is being extracted from the blood, eliminating the previous need to insert a catheter into the inferior vena cava. According to the researchers, the method offers the same precision as traditional procedures with significantly less risk to patients. Together, the ability to measure venous oxygenation and cardiac output during exercise enables clinicians to calculate whole-body oxygen usage—a vital marker for assessing risk of illness and death.
This integrated approach replaces the need for separate metabolic carts and oxygen masks with a fully MRI-based solution that is noninvasive and highly repeatable. These innovations are particularly valuable in understanding and treating exercise intolerance, a condition that not only signals underlying health problems but also significantly affects daily living. By identifying the physiological factors limiting exercise capacity, clinicians can develop more personalized and effective therapies.
“We’ve completely transformed the way we look at exercise cardiac MRI,” said researcher Michael Nelson, who led the team. “In my opinion, the recent developments we’ve made should become the new standard. You shouldn’t be doing exercise cardiac MRI without lower body negative-pressure pants.”
Related Links:
APAI Lab at University of Texas at Arlington