False-Positive CT Findings Do Not Increase Worry in Lung Cancer Patients
|
By MedImaging International staff writers Posted on 13 Aug 2014 |
The US Preventive Services Task Force (Rockville, MD, USA) recently recommended computed tomography (CT) lung screening for individuals at high risk for cancer, but a potential problem with CT scanning is that many patients will have positive findings on the screening test, only to be considered cancer-free with additional scanning. Many policymakers have expressed concern that this high false-positive rate will cause patients to become needlessly anxious.
A new study of US National Lung Screening Trial (NLST) participant responses to false-positive diagnoses, however, found that those who received false-positive screening findings did not report heightened worry or lower quality of life in comparison with participants who received negative screen findings. “Most people anticipated that participants who were told that they had a positive screen result would experience increased anxiety and reduced quality of life. However, we did not find this to be the case,” said Dr. Ilana Gareen, assistant professor (research) of epidemiology in the Brown University (Providence, RI, USA) School of Public Health and lead author of the study published online July 25, 2014, in the journal Cancer.
The NLST’s major finding, announced in 2010, was that screening with helical CT scans reduced lung cancer deaths by 20% compared to screening with chest X-rays. The huge trial spanned more than a decade, enrolling more than 53,000 smokers at 33 sites. In the new study, the investigators followed up with a subset of participants at 16 sites to assess the psychological effects of the CT and X-ray screenings compared in the trial.
“In the context of our study, with the consent process that we used, we found no increased anxiety or decreased quality of life at one or six months after screening for participants having a false-positive,” Dr. Gareen said. “What we expected was that there would be increased anxiety and decreased quality of life at one month and that these symptoms would subside by six months, which is why we measured at both time points, but we didn’t find any changes at either time point.”
The unexpected similarity between the participants with a negative and a false-positive screen findings is not because getting a false-positive diagnosis is at all pleasant, according to Dr. Gareen, but presumably because study participants understood that there was a high likelihood of a false-positive screen findings. “We think that the staff at each of the NLST sites did a very good job of providing informed consent to our participants,” she said. “In advance of any screening, participants were advised that 20%–50% of those screened would receive false positive results, and that the participants might require additional work-up to confirm that they were cancer free.”
To make its evaluations, Dr. Gareen’s team surveyed 2,812 NLST participants for the study. Patients responded well, with 2,317 returning the survey at one month after screening and 1,990 returning the survey at six months. The survey included two standardized questionnaires: the 36-question Short Form SF-36, which elicits self-reports of general physical and mental health quality, and the 20-question Spielberger State Trait Anxiety Inventory.
Dr. Maryann Duggan and her staff from the outcomes and economics evaluation unit at Brown administered the questionnaires by mail with telephone follow-up as required. In the study analysis, the researchers allocated people into groups based on their ultimate accurate diagnoses: 1,024 participants were “false-positive,” 63 were “true positive,” 1,381 were “true negative,” and 344 had a “significant incidental finding,” meaning they didn't have cancer but instead had another possible problem of medical importance.
The findings were clear after statistical adjustment for factors that could have had a confusing influence. Whether participants received X-rays or the helical CT scans, the questionnaire scores of those with false-positive diagnoses remained similar to those who were given true negative diagnoses. Meanwhile, the scores of the true positive participants who were diagnosed with lung cancer markedly worsened over time as their battle with the disease took a physical and psychological toll.
Because the individuals received the questionnaires at one and six months, it is possible that study participants receiving a false-positive screen result suffered anxiety and reduced quality of life for a short time after receiving their screen result, according to Dr. Gareen. However, by one month after their screening, there was no evidence of a difference between the screen result groups.
Dr. Gareen noted that the findings should inspire physicians to recommend appropriate screenings, in spite their high-false positive rates, as long as patients are accurately informed of the probability of a positive screen result and its implications. The data provide evidence that the NLST consent process provided a good model for recommending those undergoing screening, she reported.
Related Links:
Brown University
US Preventive Services Task Force
A new study of US National Lung Screening Trial (NLST) participant responses to false-positive diagnoses, however, found that those who received false-positive screening findings did not report heightened worry or lower quality of life in comparison with participants who received negative screen findings. “Most people anticipated that participants who were told that they had a positive screen result would experience increased anxiety and reduced quality of life. However, we did not find this to be the case,” said Dr. Ilana Gareen, assistant professor (research) of epidemiology in the Brown University (Providence, RI, USA) School of Public Health and lead author of the study published online July 25, 2014, in the journal Cancer.
The NLST’s major finding, announced in 2010, was that screening with helical CT scans reduced lung cancer deaths by 20% compared to screening with chest X-rays. The huge trial spanned more than a decade, enrolling more than 53,000 smokers at 33 sites. In the new study, the investigators followed up with a subset of participants at 16 sites to assess the psychological effects of the CT and X-ray screenings compared in the trial.
“In the context of our study, with the consent process that we used, we found no increased anxiety or decreased quality of life at one or six months after screening for participants having a false-positive,” Dr. Gareen said. “What we expected was that there would be increased anxiety and decreased quality of life at one month and that these symptoms would subside by six months, which is why we measured at both time points, but we didn’t find any changes at either time point.”
The unexpected similarity between the participants with a negative and a false-positive screen findings is not because getting a false-positive diagnosis is at all pleasant, according to Dr. Gareen, but presumably because study participants understood that there was a high likelihood of a false-positive screen findings. “We think that the staff at each of the NLST sites did a very good job of providing informed consent to our participants,” she said. “In advance of any screening, participants were advised that 20%–50% of those screened would receive false positive results, and that the participants might require additional work-up to confirm that they were cancer free.”
To make its evaluations, Dr. Gareen’s team surveyed 2,812 NLST participants for the study. Patients responded well, with 2,317 returning the survey at one month after screening and 1,990 returning the survey at six months. The survey included two standardized questionnaires: the 36-question Short Form SF-36, which elicits self-reports of general physical and mental health quality, and the 20-question Spielberger State Trait Anxiety Inventory.
Dr. Maryann Duggan and her staff from the outcomes and economics evaluation unit at Brown administered the questionnaires by mail with telephone follow-up as required. In the study analysis, the researchers allocated people into groups based on their ultimate accurate diagnoses: 1,024 participants were “false-positive,” 63 were “true positive,” 1,381 were “true negative,” and 344 had a “significant incidental finding,” meaning they didn't have cancer but instead had another possible problem of medical importance.
The findings were clear after statistical adjustment for factors that could have had a confusing influence. Whether participants received X-rays or the helical CT scans, the questionnaire scores of those with false-positive diagnoses remained similar to those who were given true negative diagnoses. Meanwhile, the scores of the true positive participants who were diagnosed with lung cancer markedly worsened over time as their battle with the disease took a physical and psychological toll.
Because the individuals received the questionnaires at one and six months, it is possible that study participants receiving a false-positive screen result suffered anxiety and reduced quality of life for a short time after receiving their screen result, according to Dr. Gareen. However, by one month after their screening, there was no evidence of a difference between the screen result groups.
Dr. Gareen noted that the findings should inspire physicians to recommend appropriate screenings, in spite their high-false positive rates, as long as patients are accurately informed of the probability of a positive screen result and its implications. The data provide evidence that the NLST consent process provided a good model for recommending those undergoing screening, she reported.
Related Links:
Brown University
US Preventive Services Task Force
Latest Radiography News
- X-Ray Breakthrough Captures Three Image-Contrast Types in Single Shot
- AI Generates Future Knee X-Rays to Predict Osteoarthritis Progression Risk
- AI Algorithm Uses Mammograms to Accurately Predict Cardiovascular Risk in Women
- AI Hybrid Strategy Improves Mammogram Interpretation
- AI Technology Predicts Personalized Five-Year Risk of Developing Breast Cancer
- RSNA AI Challenge Models Can Independently Interpret Mammograms
- New Technique Combines X-Ray Imaging and Radar for Safer Cancer Diagnosis
- New AI Tool Helps Doctors Read Chest X‑Rays Better
- Wearable X-Ray Imaging Detecting Fabric to Provide On-The-Go Diagnostic Scanning
- AI Helps Radiologists Spot More Lesions in Mammograms
- AI Detects Fatty Liver Disease from Chest X-Rays
- AI Detects Hidden Heart Disease in Existing CT Chest Scans
- Ultra-Lightweight AI Model Runs Without GPU to Break Barriers in Lung Cancer Diagnosis
- AI Radiology Tool Identifies Life-Threatening Conditions in Milliseconds

- Machine Learning Algorithm Identifies Cardiovascular Risk from Routine Bone Density Scans
- AI Improves Early Detection of Interval Breast Cancers
Channels
MRI
view channel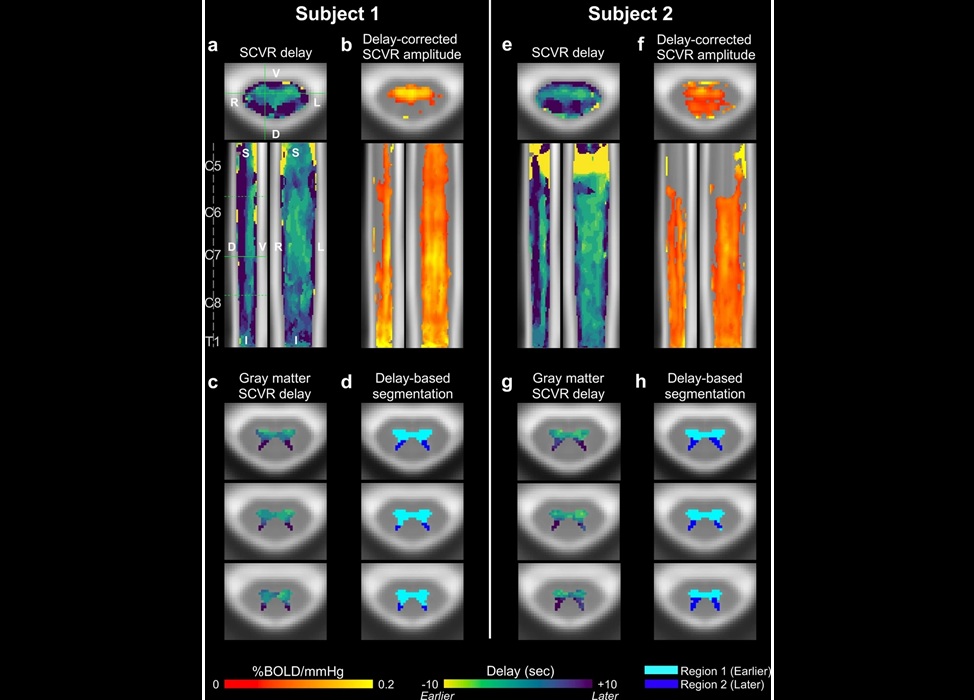
Novel Imaging Approach to Improve Treatment for Spinal Cord Injuries
Vascular dysfunction in the spinal cord contributes to multiple neurological conditions, including traumatic injuries and degenerative cervical myelopathy, where reduced blood flow can lead to progressive... Read more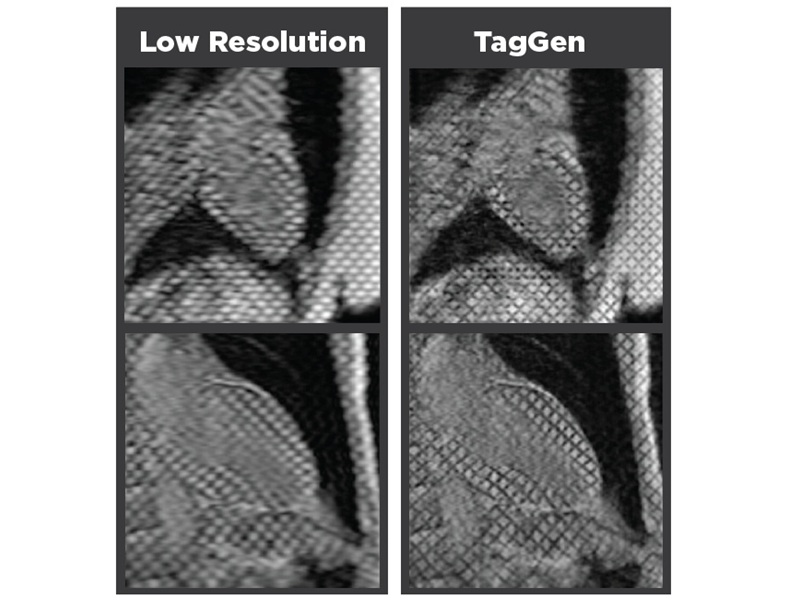
AI-Assisted Model Enhances MRI Heart Scans
A cardiac MRI can reveal critical information about the heart’s function and any abnormalities, but traditional scans take 30 to 90 minutes and often suffer from poor image quality due to patient movement.... Read more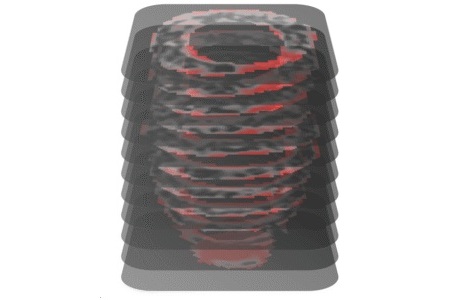
AI Model Outperforms Doctors at Identifying Patients Most At-Risk of Cardiac Arrest
Hypertrophic cardiomyopathy is one of the most common inherited heart conditions and a leading cause of sudden cardiac death in young individuals and athletes. While many patients live normal lives, some... Read moreUltrasound
view channel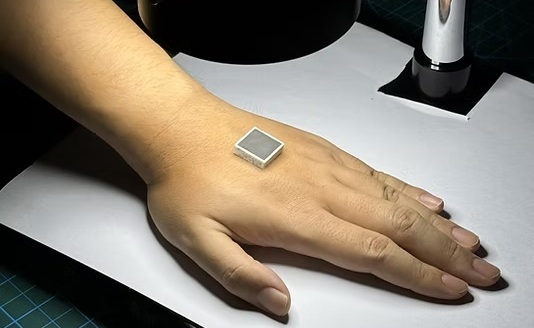
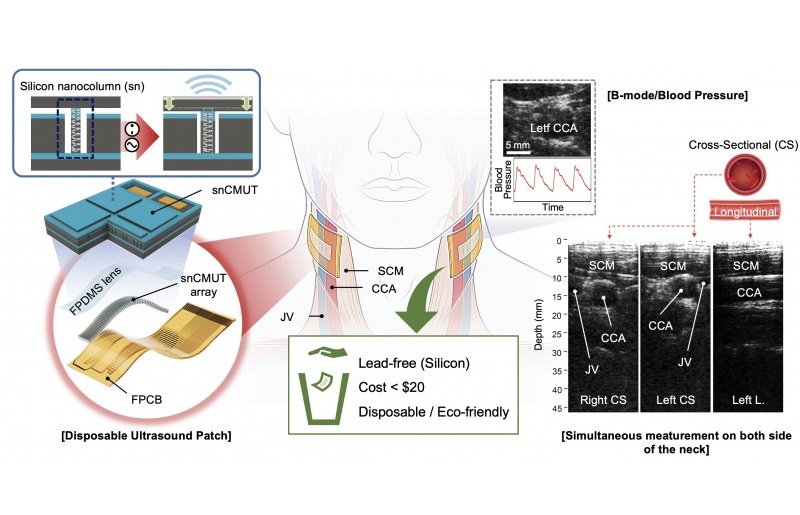
Wearable Ultrasound Imaging System to Enable Real-Time Disease Monitoring
Chronic conditions such as hypertension and heart failure require close monitoring, yet today’s ultrasound imaging is largely confined to hospitals and short, episodic scans. This reactive model limits... Read more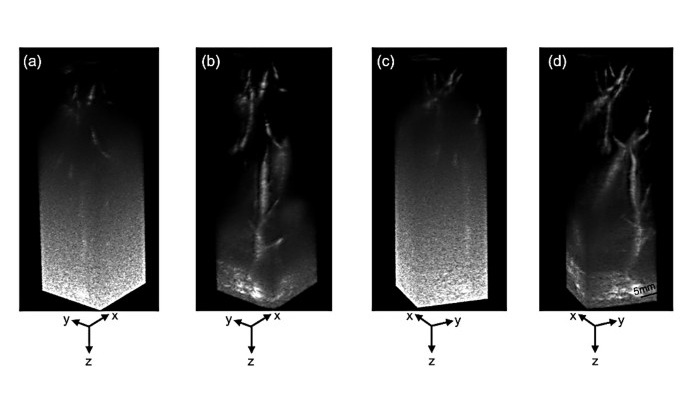
Ultrasound Technique Visualizes Deep Blood Vessels in 3D Without Contrast Agents
Producing clear 3D images of deep blood vessels has long been difficult without relying on contrast agents, CT scans, or MRI. Standard ultrasound typically provides only 2D cross-sections, limiting clinicians’... Read moreNuclear Medicine
view channel
PET Imaging of Inflammation Predicts Recovery and Guides Therapy After Heart Attack
Acute myocardial infarction can trigger lasting heart damage, yet clinicians still lack reliable tools to identify which patients will regain function and which may develop heart failure.... Read more
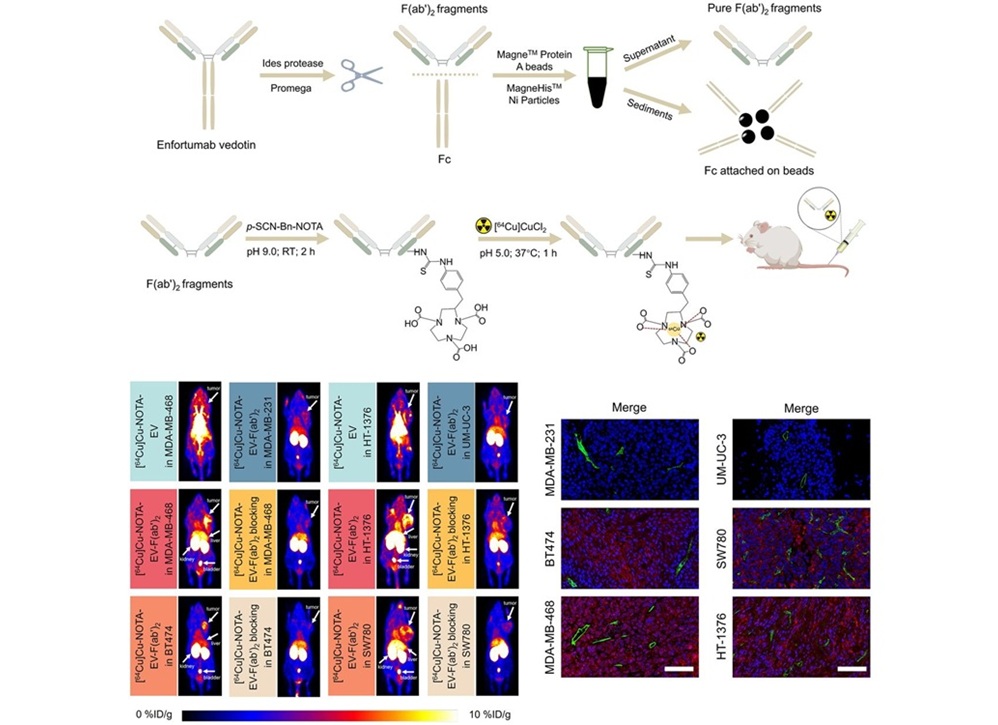
Radiotheranostic Approach Detects, Kills and Reprograms Aggressive Cancers
Aggressive cancers such as osteosarcoma and glioblastoma often resist standard therapies, thrive in hostile tumor environments, and recur despite surgery, radiation, or chemotherapy. These tumors also... Read more
New Imaging Solution Improves Survival for Patients with Recurring Prostate Cancer
Detecting recurrent prostate cancer remains one of the most difficult challenges in oncology, as standard imaging methods such as bone scans and CT scans often fail to accurately locate small or early-stage tumors.... Read moreGeneral/Advanced Imaging
view channel
3D Scanning Approach Enables Ultra-Precise Brain Surgery
Precise navigation is critical in neurosurgery, yet even small alignment errors can affect outcomes when operating deep within the brain. A new 3D surface-scanning approach now provides a radiation-free... Read more
AI Tool Improves Medical Imaging Process by 90%
Accurately labeling different regions within medical scans, a process known as medical image segmentation, is critical for diagnosis, surgery planning, and research. Traditionally, this has been a manual... Read more
New Ultrasmall, Light-Sensitive Nanoparticles Could Serve as Contrast Agents
Medical imaging technologies face ongoing challenges in capturing accurate, detailed views of internal processes, especially in conditions like cancer, where tracking disease development and treatment... Read more
AI Algorithm Accurately Predicts Pancreatic Cancer Metastasis Using Routine CT Images
In pancreatic cancer, detecting whether the disease has spread to other organs is critical for determining whether surgery is appropriate. If metastasis is present, surgery is not recommended, yet current... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more