AI Hybrid Strategy Improves Mammogram Interpretation
Posted on 22 Aug 2025
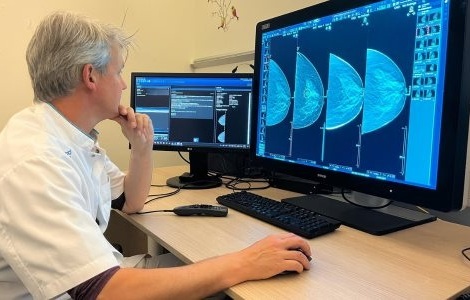
Breast cancer screening programs rely heavily on radiologists interpreting mammograms, a process that is time-intensive and subject to errors. While artificial intelligence (AI) models have shown strong performance, they can sometimes be overconfident and unreliable, creating challenges in clinical use. Now, researchers have developed a hybrid approach that combines AI certainty estimates with radiologist review, reducing workload while maintaining detection accuracy.
Researchers at Radboud University Medical Center (Nijmegen, Netherlands) developed and tested this hybrid reading strategy as part of the Dutch National Breast Cancer Screening Program. The approach uses AI to evaluate every mammogram, producing both a probability of malignancy (PoM) and an uncertainty estimate. Cases deemed certain by AI are processed automatically, while uncertain or high-risk cases are reviewed by radiologists, ensuring both safety and efficiency.
The study analyzed 41,469 mammography exams from 15,522 women, with 332 screen-detected cancers and 34 interval cancers. The dataset was split into two groups, one for setting optimal thresholds and the other for evaluation. The findings, published in Radiology, show that the hybrid method achieved a cancer detection rate of 6.6 per 1,000 and recall of 23.7 per 1,000, both comparable to traditional double-reading by radiologists.
Using this method, 38% of cases were classified as certain and safely handled by AI alone, cutting radiologist workload by 38%. The AI achieved higher accuracy when confident, with an AUC of 0.96 compared to 0.87 in uncertain cases, and sensitivity nearly equal to double radiologist reading. Younger women with dense breasts were more likely to yield uncertain AI scores, requiring human review. If these results occurred in clinical practice, the decision to recall 19% of women would be made by AI without the intervention of a radiologist.
Researchers emphasize the importance of uncertainty quantification as a tool to build trust and potentially solve workforce shortages in breast cancer screening. They note that further validation, ideally through a prospective trial, is needed to confirm its benefits in clinical practice.
“The use of AI with uncertainty quantification can be a possible solution for workforce shortages and could help build trust in the implementation of AI,” said Sarah D. Verboom, doctoral candidate in the Department of Medical Imaging at Radboud University Medical Center. "I think in the future, we could get to a point where a portion of women are sent home without ever having a radiologist look at their mammogram because AI will determine that their exam is normal. We're not there yet, but I think we could get there with this uncertainty metric and quality control."
Related Links:
Radboud University Medical Center














