Risk Profiling Used with Mammography Diagnosis Should Reduce Number of Missed Tumors
|
By MedImaging International staff writers Posted on 07 Jul 2014 |
A new approach to reading mammograms that takes into account a woman’s health risk profile would reduce the number of tumors missed, and in addition, decrease the number of false-positive findings, according to recent research.
The study’s findings were presented at a conference of the Institute for Operations Research and the Management Sciences (INFORMS; Catonsville, MD, USA), which took place June 16-18, 2014, at Georgetown University in Washington DC (USA). Mehmet U.S. Ayvaci, from the University of Texas Dallas (USA) presented his research group’s findings about the role of risk profiling in the interpretation of mammograms at Advances in Decision Analysis, a conference sponsored by the INFORMS Decision Analysis Society (DAS). Formed in 1980 with 1,000 current members, DAS supports the development and use of logical methods for improving decision-making in public and private enterprise.
The researchers found that providing radiologists with the patient’s risk profile information for breast cancer at the most advantageous time when examining the mammogram, together with statistical weighting based on profile risk, reduces false-negative results by 3.7%, thereby forewarning women whose cancer would have gone undiagnosed at an early stage, when treatment is most effective. It also reduces false-positive findings by 3.23%, thereby slashing superfluous healthcare costs and sparing patients’ needless worry.
Risk factors include family history, reproductive history, age, and ethnicity, and others forming the risk profile information. The researchers examined the complicated questions of whether providing risk profile data about women being screened for cancer biases radiologists and, if there is bias, whether this bias actually helps make readings more effective.
Historically, available clinical evidence has been inconclusive on the use of profile information when interpreting mammograms. One position is that profile information helps radiologists make better decisions and should be employed when reading mammograms. A contradictory position holds that profile information may bias the radiologists. However, whether bias always causes harm is unclear.
The investigators searched profile information and potential bias in mammography interpretation using a decision science technique called linear opinion pooling, which assigns weights to better aggregate probability estimates. They analyzed the decision performance of three groups: (1) a mammogram-only reading, with no risk profile information about the patient; (2) an unbiased reading, in which radiologists consult the risk profile after examining the mammogram; and (3) lastly, biased or “influenced” readings, in which radiologists consult a woman's risk profile as they examine the mammogram. Then they examined the conditions in which profile information could help improve biopsy decisions.
Numeric analysis using a clinical dataset from the Breast Cancer Surveillance Consortium revealed that use of profile data with an appropriate weight could reduce the false-positives and the number of missed tumors when compared to cases where profile information was not examined.
Related Links:
Institute for Operations Research and the Management Sciences
University of Texas Dallas
The study’s findings were presented at a conference of the Institute for Operations Research and the Management Sciences (INFORMS; Catonsville, MD, USA), which took place June 16-18, 2014, at Georgetown University in Washington DC (USA). Mehmet U.S. Ayvaci, from the University of Texas Dallas (USA) presented his research group’s findings about the role of risk profiling in the interpretation of mammograms at Advances in Decision Analysis, a conference sponsored by the INFORMS Decision Analysis Society (DAS). Formed in 1980 with 1,000 current members, DAS supports the development and use of logical methods for improving decision-making in public and private enterprise.
The researchers found that providing radiologists with the patient’s risk profile information for breast cancer at the most advantageous time when examining the mammogram, together with statistical weighting based on profile risk, reduces false-negative results by 3.7%, thereby forewarning women whose cancer would have gone undiagnosed at an early stage, when treatment is most effective. It also reduces false-positive findings by 3.23%, thereby slashing superfluous healthcare costs and sparing patients’ needless worry.
Risk factors include family history, reproductive history, age, and ethnicity, and others forming the risk profile information. The researchers examined the complicated questions of whether providing risk profile data about women being screened for cancer biases radiologists and, if there is bias, whether this bias actually helps make readings more effective.
Historically, available clinical evidence has been inconclusive on the use of profile information when interpreting mammograms. One position is that profile information helps radiologists make better decisions and should be employed when reading mammograms. A contradictory position holds that profile information may bias the radiologists. However, whether bias always causes harm is unclear.
The investigators searched profile information and potential bias in mammography interpretation using a decision science technique called linear opinion pooling, which assigns weights to better aggregate probability estimates. They analyzed the decision performance of three groups: (1) a mammogram-only reading, with no risk profile information about the patient; (2) an unbiased reading, in which radiologists consult the risk profile after examining the mammogram; and (3) lastly, biased or “influenced” readings, in which radiologists consult a woman's risk profile as they examine the mammogram. Then they examined the conditions in which profile information could help improve biopsy decisions.
Numeric analysis using a clinical dataset from the Breast Cancer Surveillance Consortium revealed that use of profile data with an appropriate weight could reduce the false-positives and the number of missed tumors when compared to cases where profile information was not examined.
Related Links:
Institute for Operations Research and the Management Sciences
University of Texas Dallas
Latest Radiography News
- AI Radiology Tool Identifies Life-Threatening Conditions in Milliseconds

- Machine Learning Algorithm Identifies Cardiovascular Risk from Routine Bone Density Scans
- AI Improves Early Detection of Interval Breast Cancers
- World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
- AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
- Higher Chest X-Ray Usage Catches Lung Cancer Earlier and Improves Survival
- AI-Powered Mammograms Predict Cardiovascular Risk
- Generative AI Model Significantly Reduces Chest X-Ray Reading Time
- AI-Powered Mammography Screening Boosts Cancer Detection in Single-Reader Settings
- Photon Counting Detectors Promise Fast Color X-Ray Images
- AI Can Flag Mammograms for Supplemental MRI
- 3D CT Imaging from Single X-Ray Projection Reduces Radiation Exposure
- AI Method Accurately Predicts Breast Cancer Risk by Analyzing Multiple Mammograms
- Printable Organic X-Ray Sensors Could Transform Treatment for Cancer Patients
- Highly Sensitive, Foldable Detector to Make X-Rays Safer
- Novel Breast Cancer Screening Technology Could Offer Superior Alternative to Mammogram
Channels
MRI
view channel
New MRI Technique Reveals Hidden Heart Issues
Traditional exercise stress tests conducted within an MRI machine require patients to lie flat, a position that artificially improves heart function by increasing stroke volume due to gravity-driven blood... Read more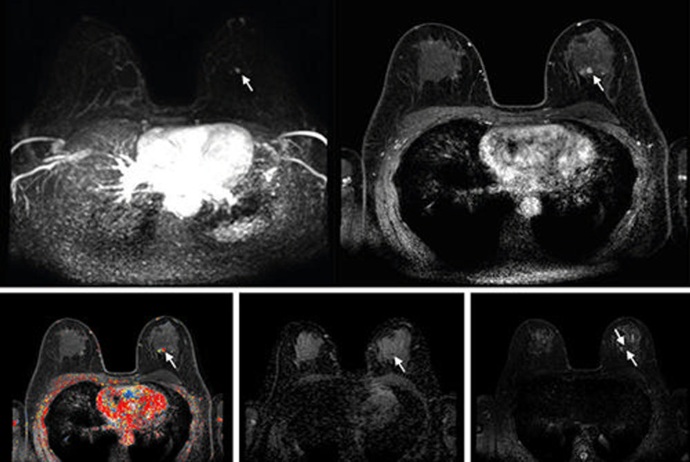
Shorter MRI Exam Effectively Detects Cancer in Dense Breasts
Women with extremely dense breasts face a higher risk of missed breast cancer diagnoses, as dense glandular and fibrous tissue can obscure tumors on mammograms. While breast MRI is recommended for supplemental... Read moreUltrasound
view channel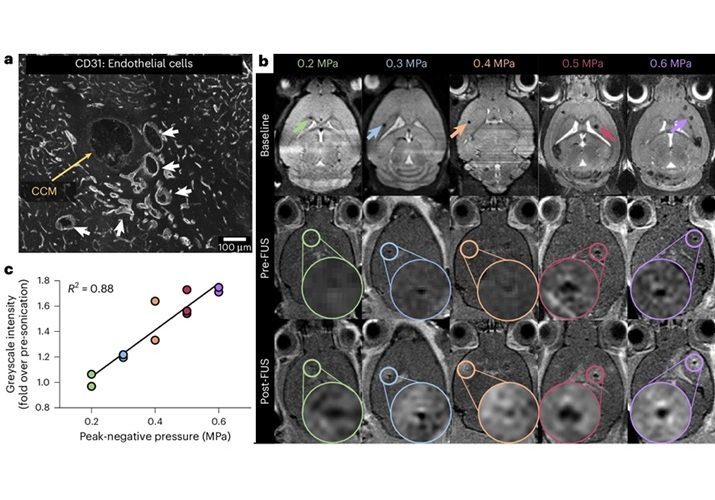
New Incision-Free Technique Halts Growth of Debilitating Brain Lesions
Cerebral cavernous malformations (CCMs), also known as cavernomas, are abnormal clusters of blood vessels that can grow in the brain, spinal cord, or other parts of the body. While most cases remain asymptomatic,... Read more.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read moreNuclear Medicine
view channel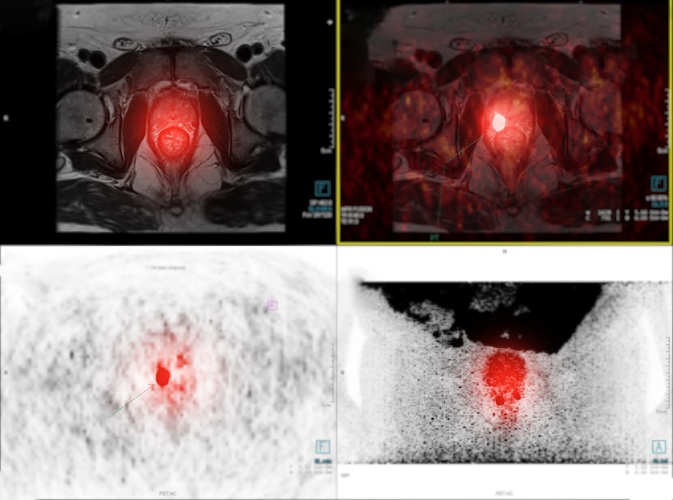
New Imaging Approach Could Reduce Need for Biopsies to Monitor Prostate Cancer
Prostate cancer is the second leading cause of cancer-related death among men in the United States. However, the majority of older men diagnosed with prostate cancer have slow-growing, low-risk forms of... Read more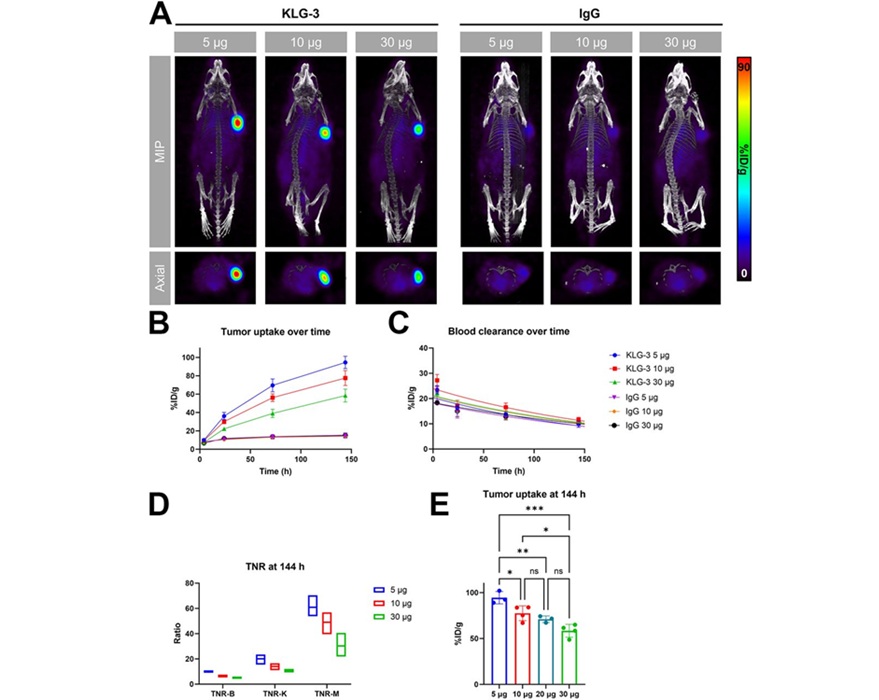
Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
Interleukin-13 receptor α-2 (IL13Rα2) is a cell surface receptor commonly found in solid tumors such as glioblastoma, melanoma, and breast cancer. It is minimally expressed in normal tissues, making it... Read moreGeneral/Advanced Imaging
view channel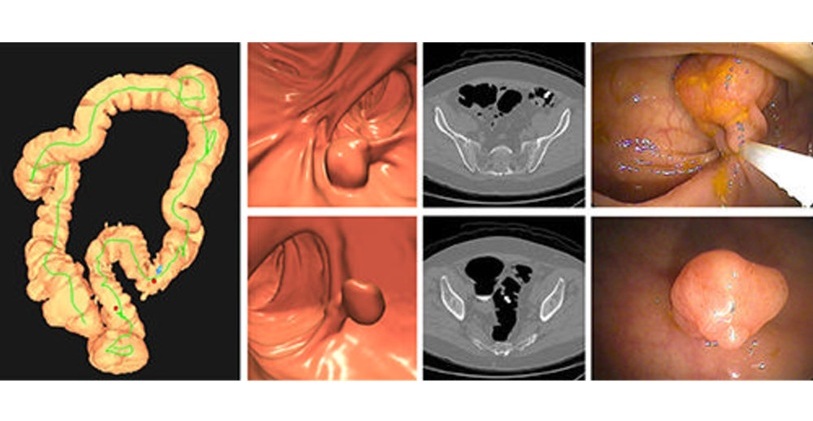
CT Colonography Beats Stool DNA Testing for Colon Cancer Screening
As colorectal cancer remains the second leading cause of cancer-related deaths worldwide, early detection through screening is vital to reduce advanced-stage treatments and associated costs.... Read more
First-Of-Its-Kind Wearable Device Offers Revolutionary Alternative to CT Scans
Currently, patients with conditions such as heart failure, pneumonia, or respiratory distress often require multiple imaging procedures that are intermittent, disruptive, and involve high levels of radiation.... Read more
AI-Based CT Scan Analysis Predicts Early-Stage Kidney Damage Due to Cancer Treatments
Radioligand therapy, a form of targeted nuclear medicine, has recently gained attention for its potential in treating specific types of tumors. However, one of the potential side effects of this therapy... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more