AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
Posted on 01 Apr 2025
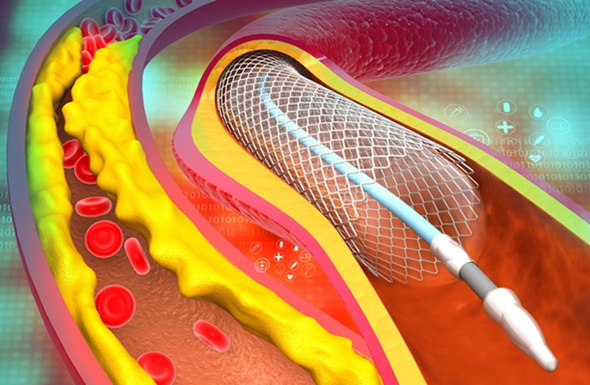
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure where small metal tubes called stents are inserted into partially blocked coronary arteries to help keep them open. To determine which patients are most likely to benefit from PCI, fractional flow reserve (FFR) assessment is used. This technique measures blood pressure and flow in the blocked arteries, helping identify which patients should undergo PCI and which ones can be managed with medication. Typically, patients with an FFR score of 0.80 or lower are recommended for PCI, while those with a score above 0.80 continue with medication. Traditional FFR assessment involves threading a catheter or wire through the body to assess blood flow and pressure in the coronary arteries. While effective in identifying those most likely to benefit from PCI, technical and logistical challenges have hindered the widespread use of this method. Now, researchers have found that patients with at least 50% narrowing in three major coronary arteries had similar outcomes when treated with a minimally invasive stent placement guided by either ultrasound-based imaging or a novel, artificial intelligence (AI)-powered non-invasive imaging method derived from angiography.
The FLAVOUR II study, conducted by researchers from The Second Affiliated Hospital of Zhejiang University School of Medicine (Hangzhou, China), aimed to assess the effectiveness of AI-powered FFR assessment in PCI outcomes. The study met its primary endpoint, which combined death, heart attack, or the need for a repeat procedure after one year. The study enrolled patients who had angiographically significant coronary artery disease, with three of the major arteries supplying blood to the heart showing inflammation or partial blockage from cholesterol buildup. The patients experienced symptoms such as chest pain and shortness of breath. The research team used an innovative AI method called AngioFFR, which calculates FFR from a single-view angiogram (X-ray) of the coronary arteries. Unlike conventional FFR assessment, AngioFFR is non-invasive, simpler, and quicker to perform. The study aimed to compare the outcomes of patients receiving PCI guided by AngioFFR with those guided by intravascular ultrasound (IVUS), which uses sound waves to visualize the extent of arterial narrowing and is the most common imaging technique for guiding PCI.
A total of 1,872 patients (average age 65 years, 68% male) from 22 medical centers in China participated in the study. To be eligible, patients needed at least 50% narrowing in three major coronary arteries, without significant narrowing in the left main coronary artery. Many of the participants had one or more co-existing conditions, including high blood pressure (67.6%), diabetes (31%), high cholesterol (66.9%), chronic kidney disease (24.3%), smoking (25%), and previous heart attack (13.9%). Participants were randomly assigned to undergo either AngioFFR-guided or IVUS-guided PCI. In the AngioFFR group, PCI was performed if the AngioFFR score was 0.80 or lower. In the IVUS group, PCI was carried out if the narrowest part of the artery was between three and four millimeters in width, and the plaque burden (the amount of plaque in the most severely narrowed part of the artery) was above 70%.
At the one-year follow-up, 73.9% of patients in the AngioFFR group received PCI, compared to 83.1% in the IVUS group. The rate of composite outcomes, including death, heart attack, or the need for a repeat procedure, was 6.3% in the AngioFFR group and 6.0% in the IVUS group, with no significant statistical difference. The clinical outcomes of both groups in terms of death, heart attack, and the need for a repeat procedure were similar. The researchers also observed no significant differences between the groups in subgroups such as patients with diabetes. The team plans to continue following the study participants for at least five years to assess any long-term differences in effectiveness between the two methods. The results were presented at the American College of Cardiology’s Annual Scientific Session (ACC.25) and published simultaneously online in The Lancet. However, the researchers acknowledged the study's limitations, including the lack of complex lesions among participants, which are more challenging to treat with PCI, and the lack of diversity in the patient population, as the study was conducted in China.
“This is the first such study to be conducted in patients with angiographically significant lesions,” said Jian’an Wang, MD, a professor in the Heart Center at The Second Affiliated Hospital of Zhejiang University School of Medicine, and the study’s senior author. “Patients whose evaluation was non-invasively guided by the novel, AI-powered technique underwent approximately 10% fewer procedures, and their outcomes were comparable with those for patients whose evaluation was guided by a commonly used ultrasound-based imaging technique.”














