Health Information Exchanges between Hospitals Benefit the Patient
|
By MedImaging International staff writers Posted on 10 Feb 2014 |
As hospitals and physicians’ offices in the United States hurry to join online systems that allow them to share medical information securely, a new study suggests that these systems may already be helping slash unnecessary care.
Fewer emergency patients received repeated medical scans when they went to a hospital that takes part in a health information exchange (HIE), according to new findings by the University of Michigan (U-M; Ann Arbor, USA) researchers, which were published online January 2014 in the journal Medical Care.
Moreover, although the project focuses specifically on scans conducted on patients who went to two different emergency departments in a 30-day period, the researchers reported that the findings serve as a good test case for the effectiveness of HIEs. The study is one of the first to demonstrate that with comprehensive data, HIEs may deliver the increased efficiency they promise. The researchers chose to examine emergency care, according to senior author and U-M Medical School emergency physician Keith Kocher, MD, because emergency department teams require information quickly in order to diagnose and treat a patient.
The capability to log in to a computer and open up that patient’s earlier records from other hospitals through an HIE instead of ordering duplicate tests or scans holds a lot of potential, he noted. But until now, large-scale studies have not been done. The findings show that the use of repeat computed tomography (CT) scans, chest X-rays and ultrasound scans was significantly lower when patients had both their emergency visits at two unaffiliated hospitals that took part in an HIE. The data come from two large US states that were among the early adopters of HIEs: California and Florida.
Patients were 59% less likely to have a redundant CT scan, 44% less likely to get a duplicate ultrasound, and 67% less likely to have a repeated chest X-ray when both their emergency visits were at hospitals that shared information across an HIE.
Kocher worked with Eric Lammers, PhD, who performed the analysis for his doctoral work at the U-M School of Public Health and is now working at Mathematica Policy Research. “The emergency department is an important test case for whether we would see any impact from HIEs on rates of repeat imaging,” said Dr. Lammers. “The fact that we find that there is a decrease is in and of itself significant.”
The US government has incentivized participation in HIEs, offering states grants to form them, and medical providers extra money if they sign on. Several HIEs have emerged in Michigan, and the two largest just announced plans to merge. HIEs are a key extension of the electronic health records that hospitals and practices are also being incentivized to adopt.
“There has been a lot of hope, and some hype, that these systems will enable more efficiency in how care is provided across unaffiliated providers,” stated Dr. Lammers. The availability of several years of data from various sources in two HIE early-adopter states gave the chance to do the study, he notes.
The researchers collected information from the California and Florida State Emergency Department Databases, for 2007 through 2010, and information on hospital HIE participation and affiliation from the Health Information Management Systems Society annual survey. The state ED databases were compiled as part of the Healthcare Cost and Utilization Project of the federal Agency for Healthcare Research and Quality.
The investigators discovered that patients in the two states underwent 20,139 repeat CT scans, meaning that 14.7% of those who had a CT scan in their first emergency visit had another one at their second emergency visit at another, unaffiliated hospital within one month. There were also 13,060 repeat ultrasounds, which were ordered for 21% of those who had had ultrasounds at their first visit, and 29,703 repeat chest X-rays ordered for 19.5% of those who had an X-ray at their first emergency visit.
While the researchers could not determine specifically that physicians at the second emergency department had accessed the patient’s records from the first ED, or that it impacted their decision-making if they did, the presence of an HIE at both hospitals means it would have been possible to do so. And they did see that the rates of repeat scanning were higher when an HIE was not present than when one was. They also estimated that if adopted nationwide, HIE might reduce healthcare costs by USD 19 million yearly for these types of repeat imaging tests in the ED.
“Our data allowed us to study a very specific type of care where HIE was associated with reducing what would potentially be a redundant test by half, which we think is pretty meaningful,” said Dr. Kocher. “We can’t say yet how generalizable these results will be to other settings, but these are definitely interesting empirical findings.”
Dr. Kocher noted that other types of patient records, such as recent lab test results, can also make a major difference in what an emergency physician chooses to do when presented with an emergency patient.
Dr. Lammers noted that not all states report the relevant data to the HCUP system, and that more wide-reaching reporting could make research on the impact of HIEs easier as the systems become more common nationwide. The data allow researchers to see the activity of individual patients across their different medical encounters, while preserving patient privacy.
Related Links:
University of Michigan
Fewer emergency patients received repeated medical scans when they went to a hospital that takes part in a health information exchange (HIE), according to new findings by the University of Michigan (U-M; Ann Arbor, USA) researchers, which were published online January 2014 in the journal Medical Care.
Moreover, although the project focuses specifically on scans conducted on patients who went to two different emergency departments in a 30-day period, the researchers reported that the findings serve as a good test case for the effectiveness of HIEs. The study is one of the first to demonstrate that with comprehensive data, HIEs may deliver the increased efficiency they promise. The researchers chose to examine emergency care, according to senior author and U-M Medical School emergency physician Keith Kocher, MD, because emergency department teams require information quickly in order to diagnose and treat a patient.
The capability to log in to a computer and open up that patient’s earlier records from other hospitals through an HIE instead of ordering duplicate tests or scans holds a lot of potential, he noted. But until now, large-scale studies have not been done. The findings show that the use of repeat computed tomography (CT) scans, chest X-rays and ultrasound scans was significantly lower when patients had both their emergency visits at two unaffiliated hospitals that took part in an HIE. The data come from two large US states that were among the early adopters of HIEs: California and Florida.
Patients were 59% less likely to have a redundant CT scan, 44% less likely to get a duplicate ultrasound, and 67% less likely to have a repeated chest X-ray when both their emergency visits were at hospitals that shared information across an HIE.
Kocher worked with Eric Lammers, PhD, who performed the analysis for his doctoral work at the U-M School of Public Health and is now working at Mathematica Policy Research. “The emergency department is an important test case for whether we would see any impact from HIEs on rates of repeat imaging,” said Dr. Lammers. “The fact that we find that there is a decrease is in and of itself significant.”
The US government has incentivized participation in HIEs, offering states grants to form them, and medical providers extra money if they sign on. Several HIEs have emerged in Michigan, and the two largest just announced plans to merge. HIEs are a key extension of the electronic health records that hospitals and practices are also being incentivized to adopt.
“There has been a lot of hope, and some hype, that these systems will enable more efficiency in how care is provided across unaffiliated providers,” stated Dr. Lammers. The availability of several years of data from various sources in two HIE early-adopter states gave the chance to do the study, he notes.
The researchers collected information from the California and Florida State Emergency Department Databases, for 2007 through 2010, and information on hospital HIE participation and affiliation from the Health Information Management Systems Society annual survey. The state ED databases were compiled as part of the Healthcare Cost and Utilization Project of the federal Agency for Healthcare Research and Quality.
The investigators discovered that patients in the two states underwent 20,139 repeat CT scans, meaning that 14.7% of those who had a CT scan in their first emergency visit had another one at their second emergency visit at another, unaffiliated hospital within one month. There were also 13,060 repeat ultrasounds, which were ordered for 21% of those who had had ultrasounds at their first visit, and 29,703 repeat chest X-rays ordered for 19.5% of those who had an X-ray at their first emergency visit.
While the researchers could not determine specifically that physicians at the second emergency department had accessed the patient’s records from the first ED, or that it impacted their decision-making if they did, the presence of an HIE at both hospitals means it would have been possible to do so. And they did see that the rates of repeat scanning were higher when an HIE was not present than when one was. They also estimated that if adopted nationwide, HIE might reduce healthcare costs by USD 19 million yearly for these types of repeat imaging tests in the ED.
“Our data allowed us to study a very specific type of care where HIE was associated with reducing what would potentially be a redundant test by half, which we think is pretty meaningful,” said Dr. Kocher. “We can’t say yet how generalizable these results will be to other settings, but these are definitely interesting empirical findings.”
Dr. Kocher noted that other types of patient records, such as recent lab test results, can also make a major difference in what an emergency physician chooses to do when presented with an emergency patient.
Dr. Lammers noted that not all states report the relevant data to the HCUP system, and that more wide-reaching reporting could make research on the impact of HIEs easier as the systems become more common nationwide. The data allow researchers to see the activity of individual patients across their different medical encounters, while preserving patient privacy.
Related Links:
University of Michigan
Latest Imaging IT News
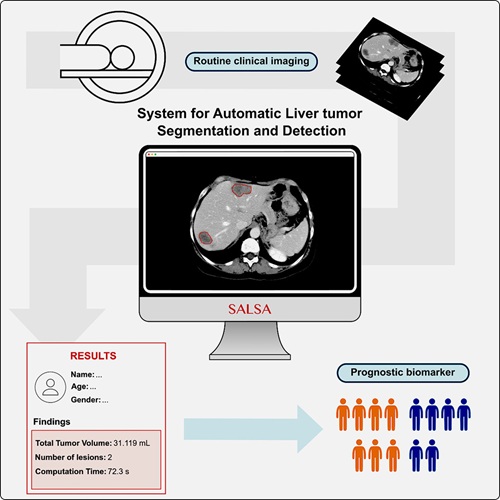
- New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
- Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
- AI-Based Mammography Triage Software Helps Dramatically Improve Interpretation Process
- Artificial Intelligence (AI) Program Accurately Predicts Lung Cancer Risk from CT Images
- Image Management Platform Streamlines Treatment Plans
- AI-Based Technology for Ultrasound Image Analysis Receives FDA Approval
- AI Technology for Detecting Breast Cancer Receives CE Mark Approval
- Digital Pathology Software Improves Workflow Efficiency
- Patient-Centric Portal Facilitates Direct Imaging Access
- New Workstation Supports Customer-Driven Imaging Workflow
Channels
Radiography
view channel
AI Radiology Tool Identifies Life-Threatening Conditions in Milliseconds
Radiology is emerging as one of healthcare’s most pressing bottlenecks. By 2033, the U.S. could face a shortage of up to 42,000 radiologists, even as imaging volumes grow by 5% annually.... Read more
Machine Learning Algorithm Identifies Cardiovascular Risk from Routine Bone Density Scans
A new study published in the Journal of Bone and Mineral Research reveals that an automated machine learning program can predict the risk of cardiovascular events and falls or fractures by analyzing bone... Read more
AI Improves Early Detection of Interval Breast Cancers
Interval breast cancers, which occur between routine screenings, are easier to treat when detected earlier. Early detection can reduce the need for aggressive treatments and improve the chances of better outcomes.... Read more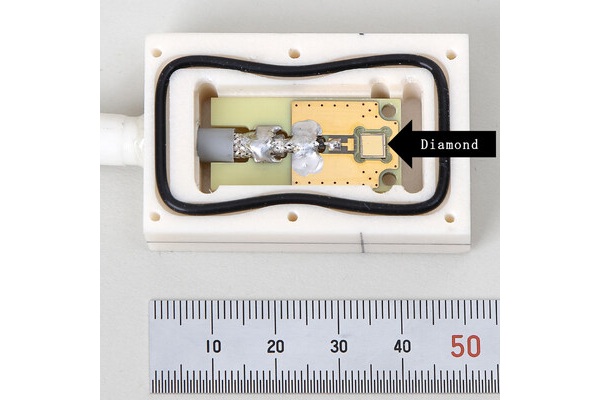
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read moreMRI
view channel
New MRI Technique Reveals Hidden Heart Issues
Traditional exercise stress tests conducted within an MRI machine require patients to lie flat, a position that artificially improves heart function by increasing stroke volume due to gravity-driven blood... Read more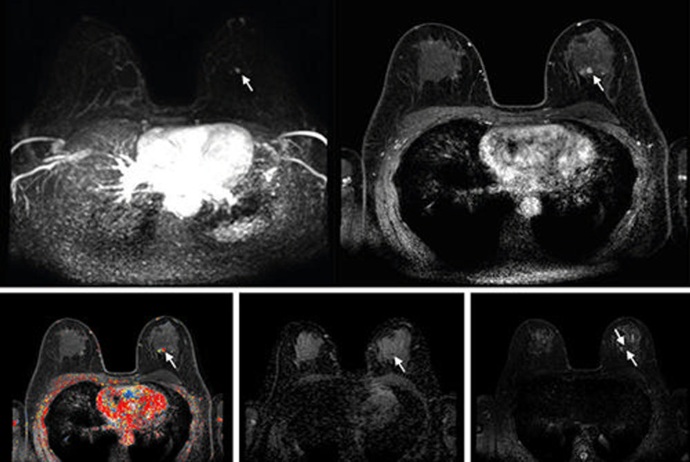
Shorter MRI Exam Effectively Detects Cancer in Dense Breasts
Women with extremely dense breasts face a higher risk of missed breast cancer diagnoses, as dense glandular and fibrous tissue can obscure tumors on mammograms. While breast MRI is recommended for supplemental... Read moreUltrasound
view channel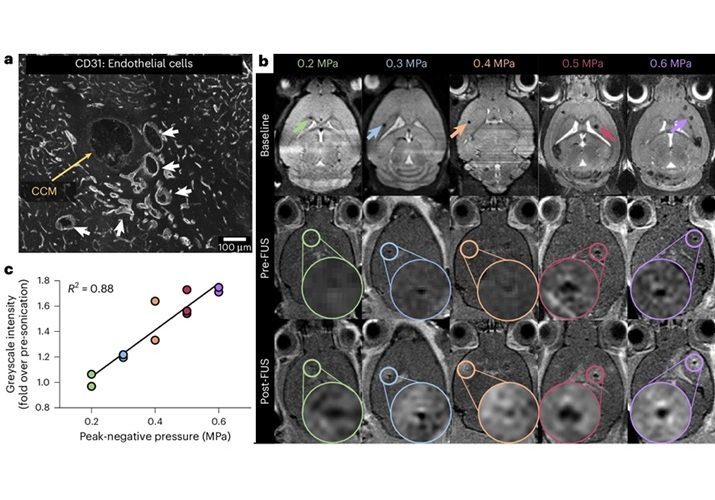
New Incision-Free Technique Halts Growth of Debilitating Brain Lesions
Cerebral cavernous malformations (CCMs), also known as cavernomas, are abnormal clusters of blood vessels that can grow in the brain, spinal cord, or other parts of the body. While most cases remain asymptomatic,... Read more.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read moreNuclear Medicine
view channel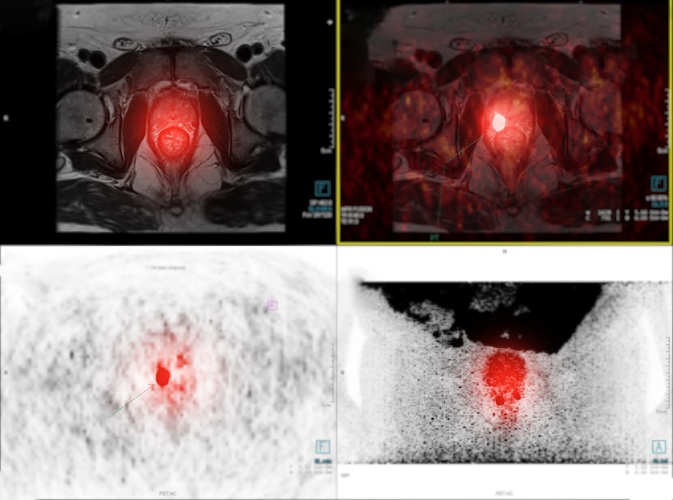
New Imaging Approach Could Reduce Need for Biopsies to Monitor Prostate Cancer
Prostate cancer is the second leading cause of cancer-related death among men in the United States. However, the majority of older men diagnosed with prostate cancer have slow-growing, low-risk forms of... Read more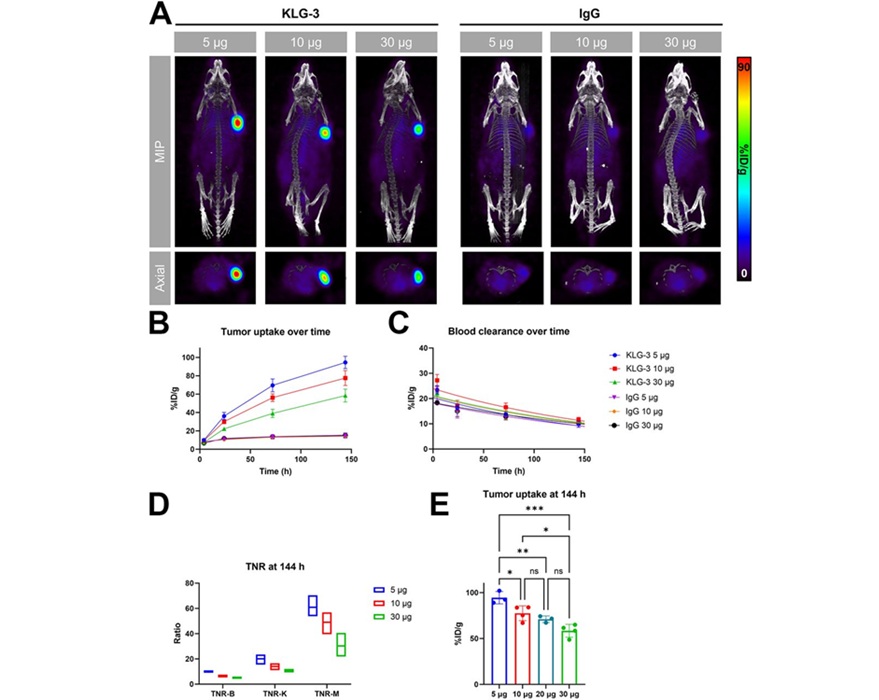
Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
Interleukin-13 receptor α-2 (IL13Rα2) is a cell surface receptor commonly found in solid tumors such as glioblastoma, melanoma, and breast cancer. It is minimally expressed in normal tissues, making it... Read moreGeneral/Advanced Imaging
view channel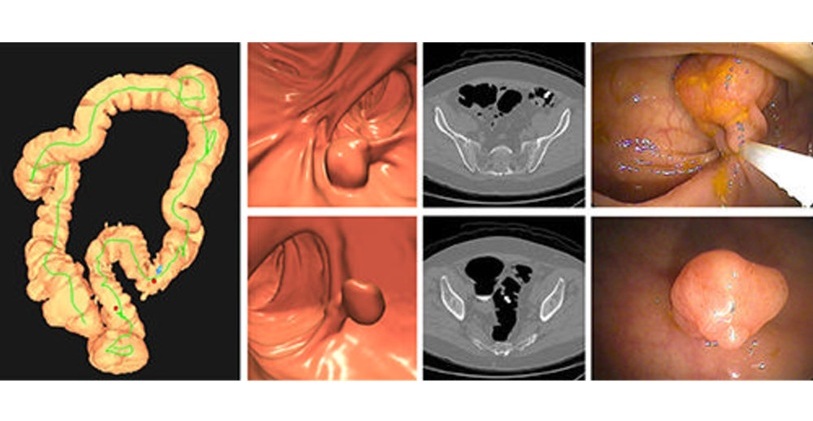
CT Colonography Beats Stool DNA Testing for Colon Cancer Screening
As colorectal cancer remains the second leading cause of cancer-related deaths worldwide, early detection through screening is vital to reduce advanced-stage treatments and associated costs.... Read more
First-Of-Its-Kind Wearable Device Offers Revolutionary Alternative to CT Scans
Currently, patients with conditions such as heart failure, pneumonia, or respiratory distress often require multiple imaging procedures that are intermittent, disruptive, and involve high levels of radiation.... Read more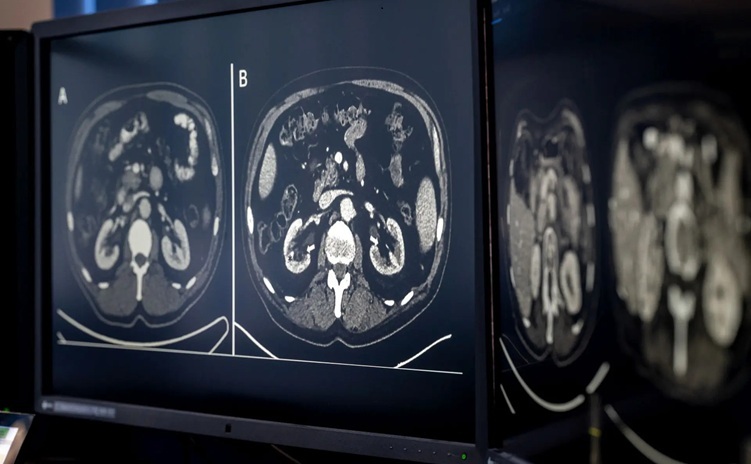
AI-Based CT Scan Analysis Predicts Early-Stage Kidney Damage Due to Cancer Treatments
Radioligand therapy, a form of targeted nuclear medicine, has recently gained attention for its potential in treating specific types of tumors. However, one of the potential side effects of this therapy... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more




 Guided Devices.jpg)