Hysterectomies Can Be Avoided for Cervical Cancer Patients Using 3D Image-Guided Brachytherapy
|
By MedImaging International staff writers Posted on 06 Jun 2012 |
Delivering radiotherapy directly to cancer of the cervix using three-dimensional (3D) imaging techniques is effective at controlling the reoccurrence and metastasis of the disease, and in most instances, avoids the need for hysterectomies.
The new findings were presented May 11, 2012, at the World Congress of Brachytherapy, held in Barcelona (Spain). Dr. Renaud Mazeron reported that a review of the use of 3D image-guided adaptive brachytherapy (IGABT) after a course of chemotherapy and radiotherapy administered together (concomitant chemoradiation) in 163 patients treated between 2004-2009 at the Institut Gustave Roussy (Villejuif, France), had shown that it achieved results that were far superior to those from earlier times using different treatments. Not only was IGABT effective at controlling the tumor, but it also had more acceptable side effects.
At present there is no conclusive evidence whether or not women with cervical cancer, particularly if it is at an advanced stage (stage IB-IIB), should have their wombs removed to help to avoid the cancer returning or spreading. This study suggests that hysterectomies may be unnecessary for most women, unless the cancer has obviously returned and invaded the womb.
Dr. Mazeron, who is an assistant professor in the radiation oncology department of the Institut Gustave Roussy, said, “IGABT is a three-dimensional technique of brachytherapy allowing a much better adaptation of treatment to the target area, while preserving healthy organs at risk from radiation. Our department has been one of the pioneers of this technique and we already have accumulated significant experience. Our current study does not formally show that surgery is unnecessary, since we did not conduct a randomized comparison, but it shows that IGABT combined with chemoradiation achieves results far superior to the historical data, with high rates of control at the site of the primary tumor. In our institute, surgeons have been convinced to abandon systematic surgery by the advances in concomitant chemoradiation and IGABT, and the conjunction of both. Historic data based on classical techniques, which gave external radiation without chemotherapy and X-ray-based brachytherapy which did not allow to adapt the treatment to each case, show that local control of a stage I tumor was usually around 90%, between 60%-87% for stage II, 44%-66% for stage III, and 18%-48% for stage IVA. In this study, we report a rate of 92% in a large group of patients with tumors at any stage.”
Of the 163 patients in the study, 27% had stage I cervical cancer, 57% stage II, 12% stage III, and 3% stage IV. They received concomitant chemoradiation followed by brachytherapy that was guided to the correct area by either magnetic resonance imaging (MRI) in 88% of cases, or computed tomography (CT) in 12% of cases.
Sixty-one (37%) of the women underwent a radical hysterectomy, but residual cancer cells were found in only 13 of these cases. Dr. Mazeron reported that the operations were partly because the study covered a crucial period when surgeons ceased to operate regularly on cervical cancer patients. “At present, surgery is proposed in case of obvious residual tumor after chemoradiation and IGABT. It is sometimes difficult to define complete remission, and thus some patients in the study were operated due to clinical or imaging suspicion of residual tumor, but finally were found to be in complete pathological remission. Currently, surgeons at our institute practice radical hysterectomy following chemoradiotherapy and IGABT only a few times per year, after a biopsy has confirmed that part of the tumor remains. However, in another study, we have shown a worse prognosis, despite surgery, for patients who do not respond completely to radiotherapy or brachytherapy due to a higher risk of metastases,” he said.
After an average follow-up of 36 months, 45 patients had relapsed, including one woman who had had a hysterectomy, and of whom 70.4% had distant metastases. “This clearly shows that distant metastases are the primary cause of relapse,” said Dr. Mazeron.
After three years, overall survival and disease-free survival was 84% and 73%, respectively. Control of the tumor at its primary site (local control) decreased in relation to the initial width of the tumor: 97% for less than 5 cm, 91% for 5-6 cm and 81% for 6 cm or more. Only 7.4% of patients experienced more severe side effects (grade 3/4), but of these 12 patients, nine had undergone a hysterectomy after radiotherapy. “This represents a strong argument for not performing surgery in patients in complete remission after treatment with concomitant chemoradiation and IGABT,” said Dr. Mazeron.
According to Dr. Mazeron, IGABT was an emerging technology and the results from this study should be validated by two international studies, one of which will be presented at the parallel ESTRO 31 conference. “IGABT is the future of brachytherapy in cervical cancer. Potential financial investments should not discourage radiation oncologists. It costs less than intensity-modulated radiation therapy [IMRT], a technique of external beam radiotherapy that has become a standard in the treatment of some cancers. We must keep in mind that cervical cancer is a public health problem in developing countries where it is the second most common cancer in women following breast cancer. IGABT represents a significant improvement in results, and some centers are already practicing this technique in India and Southeast Asia,” he concluded.
Dr. Christine Haie-Meder, radiation oncologist at the Institut Gustave Roussy and chairperson of the World Congress of Brachytherapy, commented, “Image-guided adaptive brachytherapy has recently been implemented in cervix cancer patients. Results are in favor of a significant improvement in local control. The present series also contribute to show improvement in local control with IGABT. Within this context, complementary surgery does not bring any further contribution to local control improvement, and hysterectomy may even increase the risk of complications.”
Brachytherapy is a type of internal radiotherapy, which involves putting solid radioactive material close to, or inside, the tumor. This gives a high dose of radiotherapy directly to the tumor but only a low dose to normal tissues.
The World Congress of Brachytherapy was held in parallel with the 31st conference of the European Society for Radiotherapy and Oncology (ESTRO 31), both took place in Barcelona (Spain), during May 9-13, 2012.
Related Links:
Institut Gustave Roussy
The new findings were presented May 11, 2012, at the World Congress of Brachytherapy, held in Barcelona (Spain). Dr. Renaud Mazeron reported that a review of the use of 3D image-guided adaptive brachytherapy (IGABT) after a course of chemotherapy and radiotherapy administered together (concomitant chemoradiation) in 163 patients treated between 2004-2009 at the Institut Gustave Roussy (Villejuif, France), had shown that it achieved results that were far superior to those from earlier times using different treatments. Not only was IGABT effective at controlling the tumor, but it also had more acceptable side effects.
At present there is no conclusive evidence whether or not women with cervical cancer, particularly if it is at an advanced stage (stage IB-IIB), should have their wombs removed to help to avoid the cancer returning or spreading. This study suggests that hysterectomies may be unnecessary for most women, unless the cancer has obviously returned and invaded the womb.
Dr. Mazeron, who is an assistant professor in the radiation oncology department of the Institut Gustave Roussy, said, “IGABT is a three-dimensional technique of brachytherapy allowing a much better adaptation of treatment to the target area, while preserving healthy organs at risk from radiation. Our department has been one of the pioneers of this technique and we already have accumulated significant experience. Our current study does not formally show that surgery is unnecessary, since we did not conduct a randomized comparison, but it shows that IGABT combined with chemoradiation achieves results far superior to the historical data, with high rates of control at the site of the primary tumor. In our institute, surgeons have been convinced to abandon systematic surgery by the advances in concomitant chemoradiation and IGABT, and the conjunction of both. Historic data based on classical techniques, which gave external radiation without chemotherapy and X-ray-based brachytherapy which did not allow to adapt the treatment to each case, show that local control of a stage I tumor was usually around 90%, between 60%-87% for stage II, 44%-66% for stage III, and 18%-48% for stage IVA. In this study, we report a rate of 92% in a large group of patients with tumors at any stage.”
Of the 163 patients in the study, 27% had stage I cervical cancer, 57% stage II, 12% stage III, and 3% stage IV. They received concomitant chemoradiation followed by brachytherapy that was guided to the correct area by either magnetic resonance imaging (MRI) in 88% of cases, or computed tomography (CT) in 12% of cases.
Sixty-one (37%) of the women underwent a radical hysterectomy, but residual cancer cells were found in only 13 of these cases. Dr. Mazeron reported that the operations were partly because the study covered a crucial period when surgeons ceased to operate regularly on cervical cancer patients. “At present, surgery is proposed in case of obvious residual tumor after chemoradiation and IGABT. It is sometimes difficult to define complete remission, and thus some patients in the study were operated due to clinical or imaging suspicion of residual tumor, but finally were found to be in complete pathological remission. Currently, surgeons at our institute practice radical hysterectomy following chemoradiotherapy and IGABT only a few times per year, after a biopsy has confirmed that part of the tumor remains. However, in another study, we have shown a worse prognosis, despite surgery, for patients who do not respond completely to radiotherapy or brachytherapy due to a higher risk of metastases,” he said.
After an average follow-up of 36 months, 45 patients had relapsed, including one woman who had had a hysterectomy, and of whom 70.4% had distant metastases. “This clearly shows that distant metastases are the primary cause of relapse,” said Dr. Mazeron.
After three years, overall survival and disease-free survival was 84% and 73%, respectively. Control of the tumor at its primary site (local control) decreased in relation to the initial width of the tumor: 97% for less than 5 cm, 91% for 5-6 cm and 81% for 6 cm or more. Only 7.4% of patients experienced more severe side effects (grade 3/4), but of these 12 patients, nine had undergone a hysterectomy after radiotherapy. “This represents a strong argument for not performing surgery in patients in complete remission after treatment with concomitant chemoradiation and IGABT,” said Dr. Mazeron.
According to Dr. Mazeron, IGABT was an emerging technology and the results from this study should be validated by two international studies, one of which will be presented at the parallel ESTRO 31 conference. “IGABT is the future of brachytherapy in cervical cancer. Potential financial investments should not discourage radiation oncologists. It costs less than intensity-modulated radiation therapy [IMRT], a technique of external beam radiotherapy that has become a standard in the treatment of some cancers. We must keep in mind that cervical cancer is a public health problem in developing countries where it is the second most common cancer in women following breast cancer. IGABT represents a significant improvement in results, and some centers are already practicing this technique in India and Southeast Asia,” he concluded.
Dr. Christine Haie-Meder, radiation oncologist at the Institut Gustave Roussy and chairperson of the World Congress of Brachytherapy, commented, “Image-guided adaptive brachytherapy has recently been implemented in cervix cancer patients. Results are in favor of a significant improvement in local control. The present series also contribute to show improvement in local control with IGABT. Within this context, complementary surgery does not bring any further contribution to local control improvement, and hysterectomy may even increase the risk of complications.”
Brachytherapy is a type of internal radiotherapy, which involves putting solid radioactive material close to, or inside, the tumor. This gives a high dose of radiotherapy directly to the tumor but only a low dose to normal tissues.
The World Congress of Brachytherapy was held in parallel with the 31st conference of the European Society for Radiotherapy and Oncology (ESTRO 31), both took place in Barcelona (Spain), during May 9-13, 2012.
Related Links:
Institut Gustave Roussy
Latest Nuclear Medicine News
- PET Imaging of Inflammation Predicts Recovery and Guides Therapy After Heart Attack
- Radiotheranostic Approach Detects, Kills and Reprograms Aggressive Cancers
- New Imaging Solution Improves Survival for Patients with Recurring Prostate Cancer
- PET Tracer Enables Same-Day Imaging of Triple-Negative Breast and Urothelial Cancers
- New Camera Sees Inside Human Body for Enhanced Scanning and Diagnosis
- Novel Bacteria-Specific PET Imaging Approach Detects Hard-To-Diagnose Lung Infections
- New Imaging Approach Could Reduce Need for Biopsies to Monitor Prostate Cancer
- Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
Channels
Radiography
view channel
X-Ray Breakthrough Captures Three Image-Contrast Types in Single Shot
Detecting early-stage cancer or subtle changes deep inside tissues has long challenged conventional X-ray systems, which rely only on how structures absorb radiation. This limitation keeps many microstructural... Read more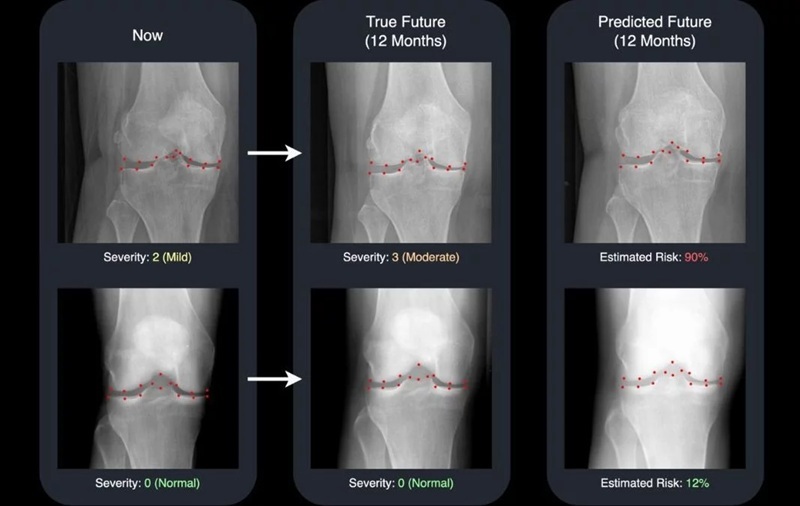
AI Generates Future Knee X-Rays to Predict Osteoarthritis Progression Risk
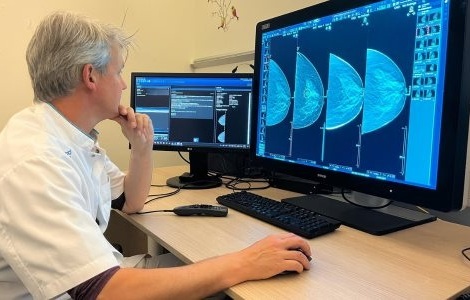
Osteoarthritis, a degenerative joint disease affecting over 500 million people worldwide, is the leading cause of disability among older adults. Current diagnostic tools allow doctors to assess damage... Read moreMRI
view channel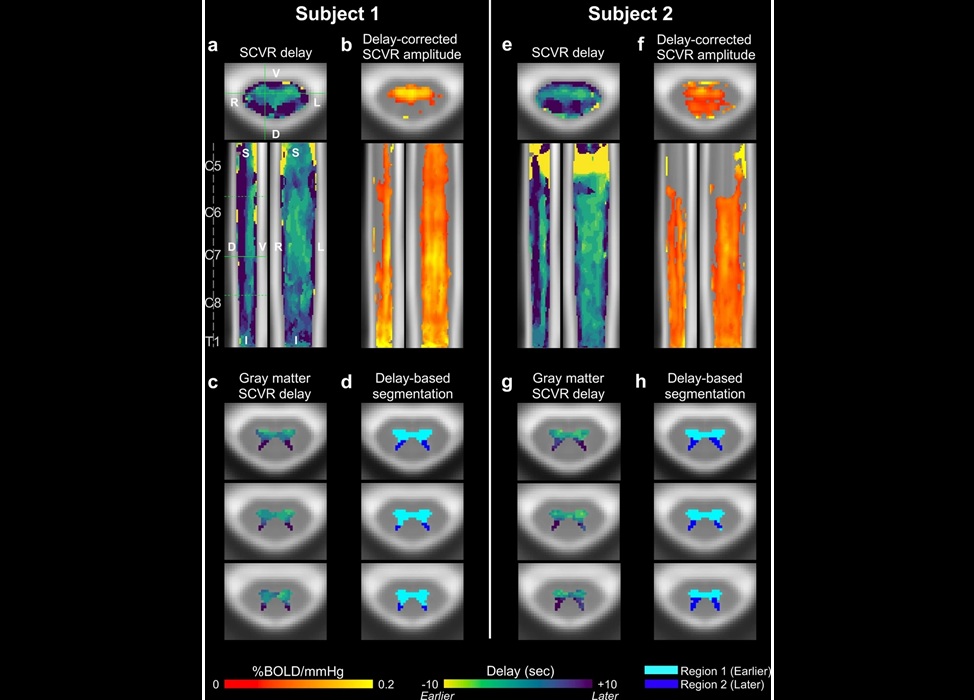
Novel Imaging Approach to Improve Treatment for Spinal Cord Injuries
Vascular dysfunction in the spinal cord contributes to multiple neurological conditions, including traumatic injuries and degenerative cervical myelopathy, where reduced blood flow can lead to progressive... Read more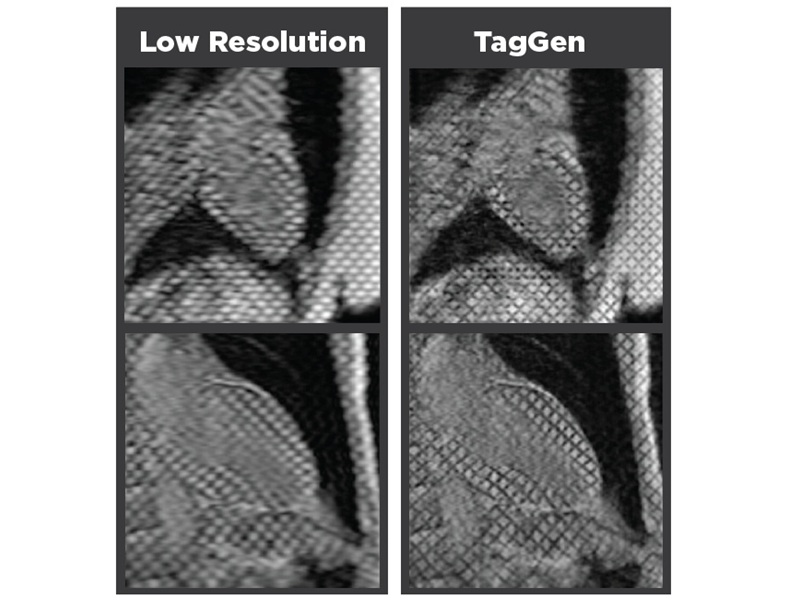
AI-Assisted Model Enhances MRI Heart Scans
A cardiac MRI can reveal critical information about the heart’s function and any abnormalities, but traditional scans take 30 to 90 minutes and often suffer from poor image quality due to patient movement.... Read more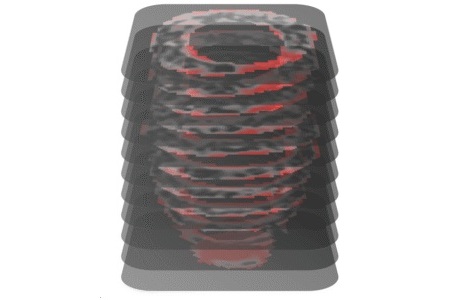
AI Model Outperforms Doctors at Identifying Patients Most At-Risk of Cardiac Arrest
Hypertrophic cardiomyopathy is one of the most common inherited heart conditions and a leading cause of sudden cardiac death in young individuals and athletes. While many patients live normal lives, some... Read moreUltrasound
view channel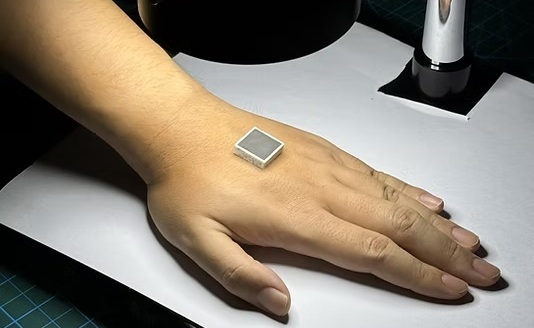
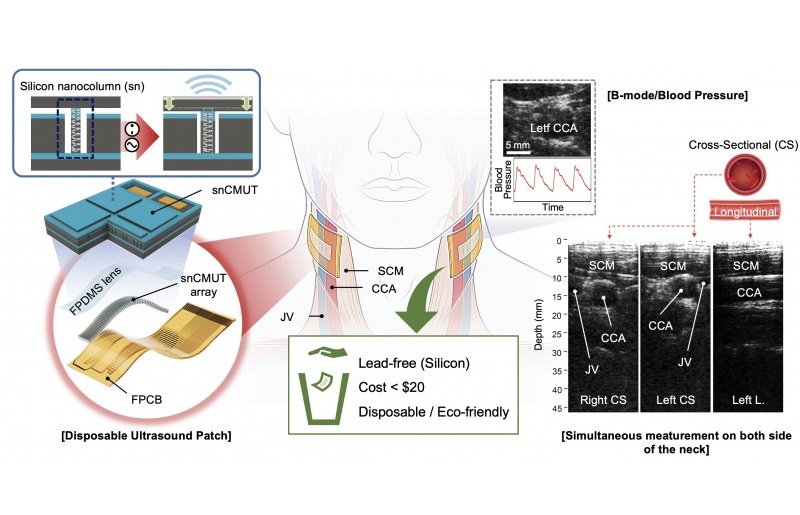
Wearable Ultrasound Imaging System to Enable Real-Time Disease Monitoring
Chronic conditions such as hypertension and heart failure require close monitoring, yet today’s ultrasound imaging is largely confined to hospitals and short, episodic scans. This reactive model limits... Read more
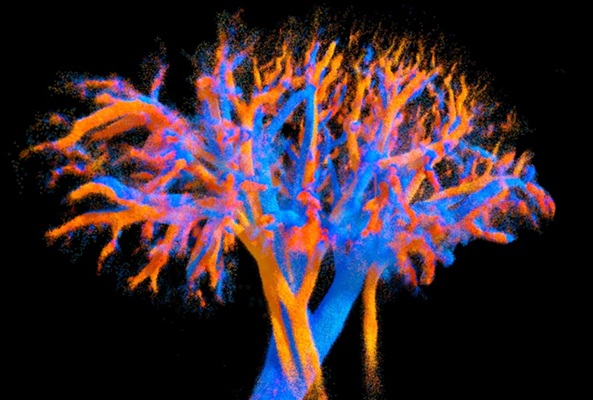
Ultrasound Technique Visualizes Deep Blood Vessels in 3D Without Contrast Agents
Producing clear 3D images of deep blood vessels has long been difficult without relying on contrast agents, CT scans, or MRI. Standard ultrasound typically provides only 2D cross-sections, limiting clinicians’... Read moreGeneral/Advanced Imaging
view channel
3D Scanning Approach Enables Ultra-Precise Brain Surgery
Precise navigation is critical in neurosurgery, yet even small alignment errors can affect outcomes when operating deep within the brain. A new 3D surface-scanning approach now provides a radiation-free... Read more
AI Tool Improves Medical Imaging Process by 90%
Accurately labeling different regions within medical scans, a process known as medical image segmentation, is critical for diagnosis, surgery planning, and research. Traditionally, this has been a manual... Read more
New Ultrasmall, Light-Sensitive Nanoparticles Could Serve as Contrast Agents
Medical imaging technologies face ongoing challenges in capturing accurate, detailed views of internal processes, especially in conditions like cancer, where tracking disease development and treatment... Read more
AI Algorithm Accurately Predicts Pancreatic Cancer Metastasis Using Routine CT Images
In pancreatic cancer, detecting whether the disease has spread to other organs is critical for determining whether surgery is appropriate. If metastasis is present, surgery is not recommended, yet current... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more