Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
Posted on 06 Jan 2025
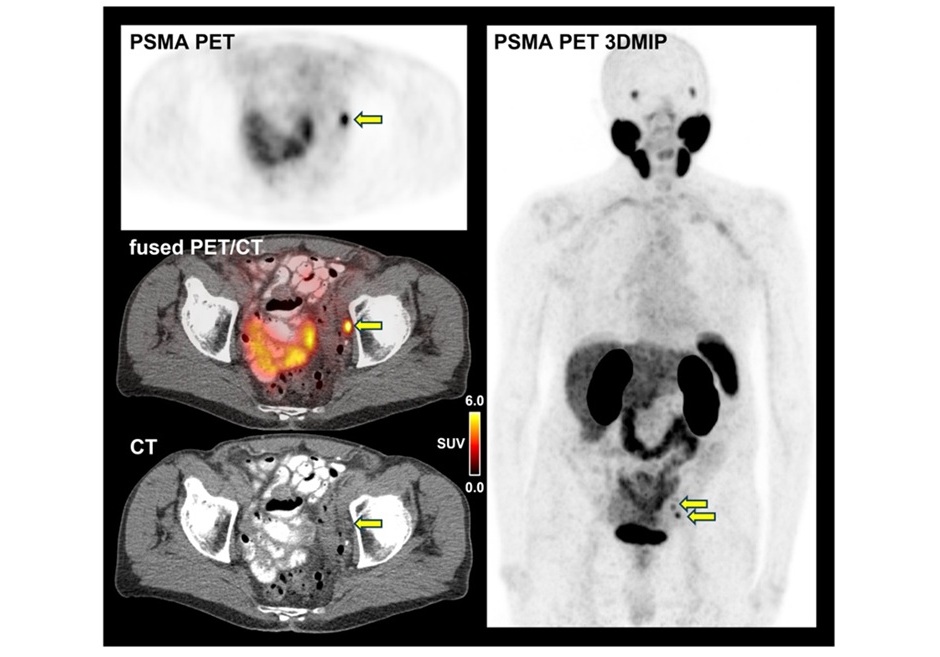
Prostate-specific membrane antigen–positron emission tomography (PSMA-PET) imaging has become an essential tool in transforming the way prostate cancer is staged. Using small amounts of radioactive “tracers,” or radiotracers, that bind to prostate cancer cells, PSMA-PET makes these cells visible on PET scans. In contrast to traditional imaging, which primarily provides anatomical details, PSMA-PET offers functional imaging that highlights the cancer’s biological activity, significantly improving disease staging accuracy. While PSMA-PET’s clinical adoption has revolutionized prostate cancer imaging, treatment decisions still often rely on clinical trials that did not incorporate this advanced imaging technique for patient selection. Now, a new study has shown that high-risk nonmetastatic hormone-sensitive prostate cancer may be more advanced than previously believed. Published in JAMA Network Open, the study found that nearly half of high-risk prostate cancer patients, initially classified as nonmetastatic by conventional imaging, were later found to have metastatic disease when assessed using PSMA-PET. This suggests that traditional imaging might often underestimate the extent of cancer spread.
To further investigate the advantages of PSMA-PET over conventional imaging, researchers at the UCLA Health Jonsson Comprehensive Cancer Center (Los Angeles, CA, USA) conducted a post hoc, retrospective cross-sectional study using data from 182 patients with high-risk recurrent prostate cancers who were previously thought to have disease limited to the prostate and eligible for the EMBARK trial. This clinical trial had previously demonstrated that adding enzalutamide, a type of hormone therapy, to androgen deprivation therapy improved metastasis-free survival. However, the trial relied on conventional imaging to classify patients, a method the researchers believe might have underestimated the disease’s spread in some instances. In this cohort, the researchers found that PSMA-PET detected cancer metastases in 46% of patients, even though traditional imaging had shown no evidence of spread. Moreover, based on PSMA-PET, 24% of the patients had five or more lesions missed by conventional imaging.
These findings challenge the conclusions of earlier studies, such as the EMBARK trial, and advocate for the inclusion of PSMA-PET in patient selection for future clinical and trial interventions in prostate cancer. They also suggest a need to reassess treatment strategies and open the possibility for potentially curative treatments, like targeted radiotherapy, for some patients. The results raise important questions about how new imaging technologies should be integrated into standard clinical care. While the study highlights the significant potential of PSMA-PET, ongoing research is needed to better understand its impact on long-term patient outcomes and how it can best inform therapy, as noted by the researchers.
“We anticipated that PSMA-PET would detect more suspicious findings compared to conventional imaging. However, it was informative to uncover such a high number of metastatic findings in a well-defined cohort of patients resembling the EMBARK trial population that was supposed to only include those without metastases,” said Dr. Adrien Holzgreve, a visiting assistant professor at the David Geffen School of Medicine and first author of the study. “We have good rationales to assume that it is helpful to primarily rely on PSMA-PET findings. But more high-quality prospective data would be needed to claim superiority of PSMA-PET for treatment-guidance in terms of patient outcome. However, we are confident PSMA-PET will continue to advance prostate cancer staging and guide personalized therapies.”














