Healthcare Costs Could Be Cut by More Appropriate Use of Cardiac Stress Imaging
|
By MedImaging International staff writers Posted on 23 Oct 2014 |
In new research, investigators concluded that overuse of cardiac stress testing using advanced imaging technology has led to increasing healthcare costs in the United States and unnecessary radiation exposure to patients.
Researchers from the New York University Langone Medical Center (NYU; New York, NY, USA), in what is believed to be the first comprehensive examination of trends in cardiac stress testing utilizing imaging, also revealed that there are no significant racial or ethnic health disparities in its use. They also made US estimates of the cost of unnecessary cardiac stress testing with imaging and the health burden of this testing, in relation to cancer risk due to radiation exposure. The study’s findings were published October 7, 2014, in the journal Annals of Internal Medicine.
Cardiac stress testing, especially with imaging, has been at the forefront of debate about rising health care costs, inappropriate use, and patient safety in the context of radiation exposure. Joseph Ladapo, MD, PhD, assistant professor in the departments of medicine and population health at NYU Langone, and the lead author of the study, and colleagues wanted to determine whether US trends in cardiac stress testing with imaging may be attributable to population shifts in demographics, risk factors, and provider characteristics, and to assess whether racial/ethnic discrepancies exist in physician decision making.
The investigators designed their study utilizing data from the US National Ambulatory Medical Care Survey (NAMCS) and US National Hospital Ambulatory Medical Care Survey (NHAMCS) from 1993 to 2010. Patients chosen for the study were adults without coronary heart disease who were referred for cardiac stress tests.
Between 1993–1995 and 2008–2010, the yearly number of ambulatory visits in the United States in which a cardiac stress test was prescribed or performed increased by more than 50%. Cardiac stress tests with imaging comprised a rising percentage of all of these tests—increasing from 59% in 1993–1995 to 87% in 2008–2010. At least 34.6% (one million tests) were probably inappropriate, the researchers concluded, with associated annual costs of USD 501 million and 491 future cases of cancer.
The authors also concluded that there was no evidence of a lower likelihood of black patients receiving a cardiac stress test with imaging (odds ratio, 0.91 [95% CI, 0.69 to 1.21]) than their white counterparts—although some slight evidence of disparity in Hispanic patients was found (odds ratio, 0.75 [CI, 0.55 to 1.02]). The investigators concluded that the national growth in cardiac stress testing can be attributed mostly to population and provider characteristics, but the use of imaging cannot. Physician decision making about cardiac stress testing also does not result in racial/ethnic disparities in cardiovascular disease.
“Cardiac stress testing is an important clinical tool,” said Dr. Ladapo, “but we are over using imaging for reasons unrelated to clinical need. This is causing preventable harm and increasing healthcare costs. “Reducing unnecessary testing also will concomitantly reduce the incidence of radiation related cancer. We estimate that about 500 people get cancer each year in the US from radiation received during a cardiac stress test when, in fact, they most probably didn’t need any radiological imaging in the first place. While this number might seem relatively small, we must remember that “first, do no harm” is one of the guiding principles in medicine.”
As to what can be done to reduce unnecessary cardiac stress testing with imaging, “More efforts, such as clinical decision support, are needed to reduce unnecessary cardiac stress testing,” Dr. Ladapo reported, suggesting greater use of stress testing without radiological imaging, such as regular exercise treadmill tests or stress testing with ultrasound imaging as opposed to CT [computed tomography] imaging.
As to why specific racial and ethnic minorities have poorer rates of treatment for cardiovascular disease and generally have poorer cardiovascular health outcomes compared to white patients, Dr. Ladapo concluded that no one has really explored whether there could be disparities in cardiac stress testing, which is a mainstay of diagnosing patients with heart disease in this country. “If we know that one minority group has a higher incidence of poorer outcomes from heart disease, perhaps we need to examine if they would benefit from more appropriate use of cardiac stress testing,” he proposed. “Perhaps one contributing reason they have poorer outcomes is because we are not testing them appropriately.”
Related Links:
New York University Langone Medical Center
Researchers from the New York University Langone Medical Center (NYU; New York, NY, USA), in what is believed to be the first comprehensive examination of trends in cardiac stress testing utilizing imaging, also revealed that there are no significant racial or ethnic health disparities in its use. They also made US estimates of the cost of unnecessary cardiac stress testing with imaging and the health burden of this testing, in relation to cancer risk due to radiation exposure. The study’s findings were published October 7, 2014, in the journal Annals of Internal Medicine.
Cardiac stress testing, especially with imaging, has been at the forefront of debate about rising health care costs, inappropriate use, and patient safety in the context of radiation exposure. Joseph Ladapo, MD, PhD, assistant professor in the departments of medicine and population health at NYU Langone, and the lead author of the study, and colleagues wanted to determine whether US trends in cardiac stress testing with imaging may be attributable to population shifts in demographics, risk factors, and provider characteristics, and to assess whether racial/ethnic discrepancies exist in physician decision making.
The investigators designed their study utilizing data from the US National Ambulatory Medical Care Survey (NAMCS) and US National Hospital Ambulatory Medical Care Survey (NHAMCS) from 1993 to 2010. Patients chosen for the study were adults without coronary heart disease who were referred for cardiac stress tests.
Between 1993–1995 and 2008–2010, the yearly number of ambulatory visits in the United States in which a cardiac stress test was prescribed or performed increased by more than 50%. Cardiac stress tests with imaging comprised a rising percentage of all of these tests—increasing from 59% in 1993–1995 to 87% in 2008–2010. At least 34.6% (one million tests) were probably inappropriate, the researchers concluded, with associated annual costs of USD 501 million and 491 future cases of cancer.
The authors also concluded that there was no evidence of a lower likelihood of black patients receiving a cardiac stress test with imaging (odds ratio, 0.91 [95% CI, 0.69 to 1.21]) than their white counterparts—although some slight evidence of disparity in Hispanic patients was found (odds ratio, 0.75 [CI, 0.55 to 1.02]). The investigators concluded that the national growth in cardiac stress testing can be attributed mostly to population and provider characteristics, but the use of imaging cannot. Physician decision making about cardiac stress testing also does not result in racial/ethnic disparities in cardiovascular disease.
“Cardiac stress testing is an important clinical tool,” said Dr. Ladapo, “but we are over using imaging for reasons unrelated to clinical need. This is causing preventable harm and increasing healthcare costs. “Reducing unnecessary testing also will concomitantly reduce the incidence of radiation related cancer. We estimate that about 500 people get cancer each year in the US from radiation received during a cardiac stress test when, in fact, they most probably didn’t need any radiological imaging in the first place. While this number might seem relatively small, we must remember that “first, do no harm” is one of the guiding principles in medicine.”
As to what can be done to reduce unnecessary cardiac stress testing with imaging, “More efforts, such as clinical decision support, are needed to reduce unnecessary cardiac stress testing,” Dr. Ladapo reported, suggesting greater use of stress testing without radiological imaging, such as regular exercise treadmill tests or stress testing with ultrasound imaging as opposed to CT [computed tomography] imaging.
As to why specific racial and ethnic minorities have poorer rates of treatment for cardiovascular disease and generally have poorer cardiovascular health outcomes compared to white patients, Dr. Ladapo concluded that no one has really explored whether there could be disparities in cardiac stress testing, which is a mainstay of diagnosing patients with heart disease in this country. “If we know that one minority group has a higher incidence of poorer outcomes from heart disease, perhaps we need to examine if they would benefit from more appropriate use of cardiac stress testing,” he proposed. “Perhaps one contributing reason they have poorer outcomes is because we are not testing them appropriately.”
Related Links:
New York University Langone Medical Center
Latest Radiography News
- Novel Breast Cancer Screening Technology Could Offer Superior Alternative to Mammogram
- Artificial Intelligence Accurately Predicts Breast Cancer Years Before Diagnosis
- AI-Powered Chest X-Ray Detects Pulmonary Nodules Three Years Before Lung Cancer Symptoms
- AI Model Identifies Vertebral Compression Fractures in Chest Radiographs
- Advanced 3D Mammography Detects More Breast Cancers
- AI X-Ray Diagnostic Tool Offers Rapid Pediatric Fracture Detection
- AI-Powered Chest X-Ray Analysis Shows Promise in Clinical Practice
- AI-Based Algorithm Improves Accuracy of Breast Cancer Diagnoses
- Groundbreaking X-Ray Imaging Technique Could Improve Medical Diagnostics
- Innovative X-Ray Technique Captures Human Heart with Unprecedented Detail
- Cutting-Edge Technology Enhances Chest X-Ray Classification for Superior Patient Outcomes
- AI Model Accurately Estimates Lung Function Using Chest X-Rays
- High-Powered Motorized Mobile C-Arm Delivers State-Of-The-Art Images for Challenging Procedures
- Injury Prediction Rule Reduces Radiographic Imaging Exposure in Children
- AI Detects More Breast Cancers with Fewer False Positives
- AI-Powered Portable Thermal Imaging Solution Could Complement Mammography for Breast Cancer Screening
Channels
MRI
view channel
Groundbreaking AI-Powered Software Significantly Enhances Brain MRI
Contrast-enhanced magnetic resonance imaging (MRI) utilizes contrast agents to illuminate specific tissues or abnormalities, leading to improved visualization and more comprehensive information.... Read more.jpeg)
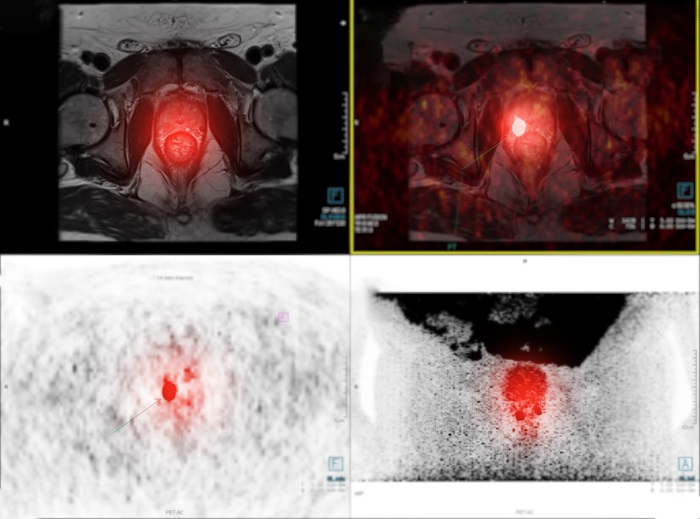
MRI Predicts Patient Outcomes and Tumor Recurrence in Rectal Cancer Patients
Colorectal cancer is on the rise among younger adults—those under 50—while it has been declining in older populations. It is estimated that approximately 1 in 23 men and 1 in 25 women will be diagnosed... Read more
Portable MRI System Dramatically Cuts Time-To-Scan vs. Conventional MRI in Stroke Patients
Imaging of the brain is crucial for the management of acute stroke and transient ischemic attack. Key roles of imaging include confirming the diagnosis, determining treatment eligibility, indicating the... Read moreUltrasound
view channel
Ultrasound Can Identify Sources of Brain-Related Issues and Disorders Before Treatment
For many years, healthcare professionals worldwide have relied on ultrasound to monitor the growth of unborn infants and evaluate the health of internal organs. However, ultrasound technology, once primarily... Read more
New Guideline on Handling Endobronchial Ultrasound Transbronchial Needle Samples
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has become the standard procedure for the initial diagnosis and staging of lung cancer; however, there is limited guidance on... Read more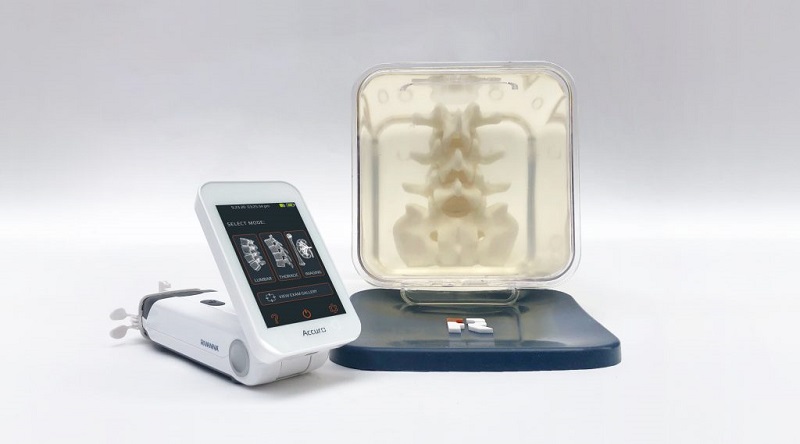
Groundbreaking Ultrasound-Guided Needle Insertion System Improves Medical Procedures
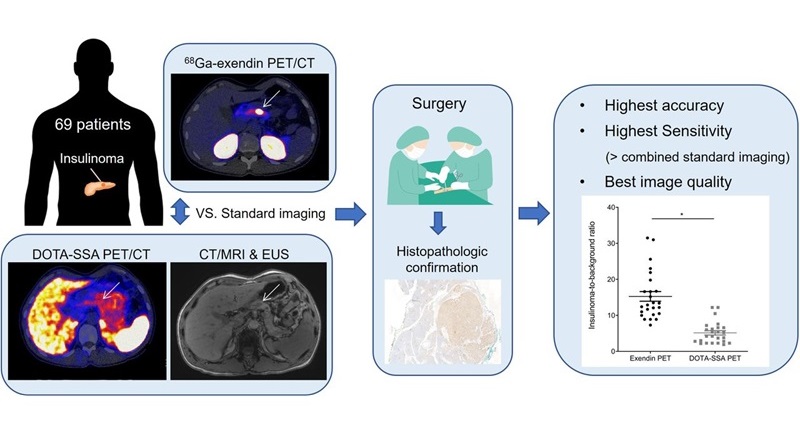
Ultrasound-guided neuraxial procedures have traditionally been hampered by technical challenges, such as the need for three hands to manage the needle, probe, and syringe simultaneously, steep needle angles... Read moreNuclear Medicine
view channel
PET Software Enhances Diagnosis and Monitoring of Alzheimer's Disease
Alzheimer’s disease is marked by the buildup of beta-amyloid plaques and tau protein tangles in the brain. These deposits of beta-amyloid and tau appear in various brain regions at differing rates as the brain ages.... Read more.jpg)
New Photon-Counting CT Technique Diagnoses Osteoarthritis Before Symptoms Develop
X-ray imaging has evolved significantly since its introduction in 1895. This technique is known for capturing images quickly, making it ideal for emergency situations; however, it does not provide adequate... Read moreGeneral/Advanced Imaging
view channel
Low-Dose CT Screening for Lung Cancer Can Benefit Heavy Smokers
Lung cancer is often diagnosed at a late stage, with only about one-fifth to one-sixth of patients surviving five years after diagnosis. A new report now suggests that low-dose computed tomography (CT)... Read more![Image: A kidney showing positive [89Zr]Zr-girentuximab PET and histologically confirmed clear-cell renal cell carcinoma (Photo courtesy of Dr. Brian Shuch/UCLA Health) Image: A kidney showing positive [89Zr]Zr-girentuximab PET and histologically confirmed clear-cell renal cell carcinoma (Photo courtesy of Dr. Brian Shuch/UCLA Health)](https://globetechcdn.com/mobile_medicalimaging/images/stories/articles/article_images/2024-10-04/ca9scan.jpg)
Non-Invasive Imaging Technique Accurately Detects Aggressive Kidney Cancer
Kidney cancers, known as renal cell carcinomas, account for 90% of solid kidney tumors, with over 81,000 new cases diagnosed annually in the United States. Among the various types, clear-cell renal cell... Read more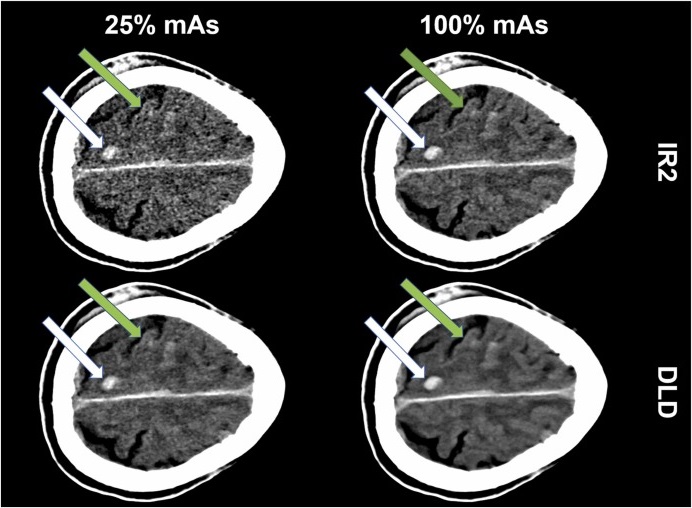
AI Algorithm Reduces Unnecessary Radiation Exposure in Traumatic Neuroradiological CT Scans
Traumatic neuroradiological emergencies encompass conditions that require immediate and accurate diagnosis for effective treatment and optimal patient outcomes. These emergencies can include injuries to... Read more
New Solution Enhances AI-Based Quality Control and Diagnosis in Medical Imaging
Medical image data makes up 80% of clinical data, and artificial intelligence (AI) offers significant potential to unlock its full value, which is crucial for clinical diagnosis, decision-making, and disease... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel.jpeg)
Philips and Medtronic Partner on Stroke Care
A stroke is typically an acute incident primarily caused by a blockage in a brain blood vessel, which disrupts the adequate blood supply to brain tissue and results in the permanent loss of brain cells.... Read more
Siemens and Medtronic Enter into Global Partnership for Advancing Spine Care Imaging Technologies
A new global partnership aims to explore opportunities to further expand access to advanced pre-and post-operative imaging technologies for spine care. Medtronic plc (Galway, Ireland) and Siemens Healthineers... Read more
RSNA 2024 Technical Exhibits to Showcase Latest Advances in Radiology
The Radiological Society of North America (RSNA, Oak Brook, IL, USA) has announced highlights of the Technical Exhibits at RSNA 2024: Building Intelligent Connections, the Society’s 110th Scientific Assembly... Read more













.jpg)