CT Scanning Not Necessary for Minor Head Injuries in Children
|
By MedImaging International staff writers Posted on 24 Jul 2014 |
A US study of more than 40,000 children evaluated in hospital emergency departments for head trauma revealed that if children had only loss of consciousness, and no other signs or symptoms related to the head trauma, they are very unlikely to have sustained serious brain injuries. Children who have only isolated loss of consciousness after head trauma do not routinely require computed tomography (CT) scans of the head, according to the investigators of the research.
Although CT scans are the most typical way to determine if a child has life-threatening bleeding in the brain that may necessitate surgical intervention, the radiation involved carries a small but quantifiable long-term risk of cancer. As such, the data indicate that CT evaluation for children with head trauma should not be routinely used if they are at low risk for clinically significant traumatic brain injuries.
The findings were published July 9, 2014, in the journal JAMA Pediatrics. “Fear of missing a clinically significant head injury, and the wide availability of CT scanners, have been the main factors driving an increase in the use of CT imaging over the past two decades,” said Nathan Kuppermann, professor and chair of the University of California (UC) Davis (USA) department of emergency medicine, and lead investigator of the original study from which the data and current analysis of head injuries were derived. “Our findings can help doctors confidently make a decision to forego CT testing when their patients are unlikely to benefit from it, enabling physicians to first observe their patients for a period of time before deciding on CT use.”
Whether the presence of a single factor suggestive of brain injury is reason enough to justify obtaining a CT scan has been a question Prof. Kuppermann and colleagues with the Pediatric Emergency Care Applied Research Network (PECARN; Salt Lake City, UT, USA) have been actively searching through a series of studies over the past few years. The current study revealed that children who lost consciousness after head trauma, but then were awake and alert in the emergency department, and had none of the other five factors determined important by PECARN guidelines for identifying children at low risk for clinically important brain injuries after head trauma (called the PECARN traumatic brain injury prediction rules), had a very low rate of clinically significant brain injuries—only 0.5%, or 1 in 200 children.
If a child had isolated loss of consciousness without any other symptoms or signs of head trauma (i.e., including factors outside of the PECARN traumatic brain injury prediction rules), the incidence of an important brain injury decreased to only 0.2%, or 1 in 500 children. Furthermore, the duration of the loss of consciousness did not significantly affect risk.
“Children with clinically important brain injuries rarely have loss of consciousness alone, and almost always present other symptoms, such as vomiting or showing signs of neurological problems,” said Dr. Lois K. Lee, lead author of the current study and director of trauma research at Boston Children’s Hospital (MA, USA). “Being able to make treatment decisions backed by strong data helps doctors and parents feel better about deciding whether further testing is really needed.”
Moreover, Dr. Lee noted that in instances in which a parent or physician is worried about a child’s condition, it would be sensible to observe the child in the emergency department for a few hours to see if any other signs or symptoms arise before making the decision whether to have a CT.
Research shows that exposure to the ionizing radiation related to CT scanning increase the risk of cancer. Based on a child’s age, one head CT scan for a child is the same as approximately 140 chest X-rays, according to The Essential Physics of Medical Imaging. Radiation exposure in the brains of developing children is of special concern and must be considered carefully against the risk of traumatic brain injury that could cause permanent damage or death if not identified early. The investigators noted that if the guidelines are applied correctly, the use of unnecessary CT scans could be substantially reduced.
An earlier, groundbreaking study led by Prof. Kuppermann and published by the Lancet in 2009 developed and validated a traumatic brain injury prediction rule to identify children at low risk for clinically important head injuries who probably do not require CT evaluation. Factors in the rule included abnormal mental status, scalp hematoma (in children younger than two years old), evidence of vomiting, a skull fracture, history of loss of consciousness associated with the head trauma, and severity of the injury process (such as a major fall). If a child with head trauma has none of the six associated factors, researchers determined that a CT scan would be very unlikely to reveal a clinically significant problem, making it unnecessary for a child to undergo the CT scan.
Two related studies led by Prof. Kuppermann and his team were recently published in the Annals of Emergency Medicine. One, in the June 2014 issue, examined whether vomiting by itself necessitates a CT scan in children who have acute head trauma. The second, in the March 2014 issue, evaluated whether swelling of the scalp in children younger than two years old, as a result of a head trauma by itself, justifies a CT scan. Both studies determined that the presence of these individual factors alone, with no other signs and symptoms of head trauma, were not sufficient to warrants an immediate CT scan. Instead, the researchers reported that children in these instances should be observed for a period of time before any decisions regarding CT use are made.
“Head trauma in children results in nearly half-a-million visits to US emergency departments annually,” said Dr. Peter Dayan, lead author of both recent studies and an associate professor of pediatrics at Columbia University (New York, NY, USA). “Our research provides important support for frontline doctors to help them avoid unnecessarily exposing children to the radiation risks inherent in CT testing.”
The head trauma study was designed by Prof. Kuppermann and colleagues in PECARN to determine which children evaluated in the emergency department for head trauma are at low risk for clinically significant traumatic brain injuries and who do not require cranial CT assessment. The pediatric research network comprises 18 hospital emergency departments across the nation and serves more than 1.2 million children. The immense amount of data generated by this patient population enables investigators to confidently answer questions about best practices, according to the investigators.
Related Links:
University of California, Davis
Boston Children’s Hospital
Pediatric Emergency Care Applied Research Network
Columbia University
Although CT scans are the most typical way to determine if a child has life-threatening bleeding in the brain that may necessitate surgical intervention, the radiation involved carries a small but quantifiable long-term risk of cancer. As such, the data indicate that CT evaluation for children with head trauma should not be routinely used if they are at low risk for clinically significant traumatic brain injuries.
The findings were published July 9, 2014, in the journal JAMA Pediatrics. “Fear of missing a clinically significant head injury, and the wide availability of CT scanners, have been the main factors driving an increase in the use of CT imaging over the past two decades,” said Nathan Kuppermann, professor and chair of the University of California (UC) Davis (USA) department of emergency medicine, and lead investigator of the original study from which the data and current analysis of head injuries were derived. “Our findings can help doctors confidently make a decision to forego CT testing when their patients are unlikely to benefit from it, enabling physicians to first observe their patients for a period of time before deciding on CT use.”
Whether the presence of a single factor suggestive of brain injury is reason enough to justify obtaining a CT scan has been a question Prof. Kuppermann and colleagues with the Pediatric Emergency Care Applied Research Network (PECARN; Salt Lake City, UT, USA) have been actively searching through a series of studies over the past few years. The current study revealed that children who lost consciousness after head trauma, but then were awake and alert in the emergency department, and had none of the other five factors determined important by PECARN guidelines for identifying children at low risk for clinically important brain injuries after head trauma (called the PECARN traumatic brain injury prediction rules), had a very low rate of clinically significant brain injuries—only 0.5%, or 1 in 200 children.
If a child had isolated loss of consciousness without any other symptoms or signs of head trauma (i.e., including factors outside of the PECARN traumatic brain injury prediction rules), the incidence of an important brain injury decreased to only 0.2%, or 1 in 500 children. Furthermore, the duration of the loss of consciousness did not significantly affect risk.
“Children with clinically important brain injuries rarely have loss of consciousness alone, and almost always present other symptoms, such as vomiting or showing signs of neurological problems,” said Dr. Lois K. Lee, lead author of the current study and director of trauma research at Boston Children’s Hospital (MA, USA). “Being able to make treatment decisions backed by strong data helps doctors and parents feel better about deciding whether further testing is really needed.”
Moreover, Dr. Lee noted that in instances in which a parent or physician is worried about a child’s condition, it would be sensible to observe the child in the emergency department for a few hours to see if any other signs or symptoms arise before making the decision whether to have a CT.
Research shows that exposure to the ionizing radiation related to CT scanning increase the risk of cancer. Based on a child’s age, one head CT scan for a child is the same as approximately 140 chest X-rays, according to The Essential Physics of Medical Imaging. Radiation exposure in the brains of developing children is of special concern and must be considered carefully against the risk of traumatic brain injury that could cause permanent damage or death if not identified early. The investigators noted that if the guidelines are applied correctly, the use of unnecessary CT scans could be substantially reduced.
An earlier, groundbreaking study led by Prof. Kuppermann and published by the Lancet in 2009 developed and validated a traumatic brain injury prediction rule to identify children at low risk for clinically important head injuries who probably do not require CT evaluation. Factors in the rule included abnormal mental status, scalp hematoma (in children younger than two years old), evidence of vomiting, a skull fracture, history of loss of consciousness associated with the head trauma, and severity of the injury process (such as a major fall). If a child with head trauma has none of the six associated factors, researchers determined that a CT scan would be very unlikely to reveal a clinically significant problem, making it unnecessary for a child to undergo the CT scan.
Two related studies led by Prof. Kuppermann and his team were recently published in the Annals of Emergency Medicine. One, in the June 2014 issue, examined whether vomiting by itself necessitates a CT scan in children who have acute head trauma. The second, in the March 2014 issue, evaluated whether swelling of the scalp in children younger than two years old, as a result of a head trauma by itself, justifies a CT scan. Both studies determined that the presence of these individual factors alone, with no other signs and symptoms of head trauma, were not sufficient to warrants an immediate CT scan. Instead, the researchers reported that children in these instances should be observed for a period of time before any decisions regarding CT use are made.
“Head trauma in children results in nearly half-a-million visits to US emergency departments annually,” said Dr. Peter Dayan, lead author of both recent studies and an associate professor of pediatrics at Columbia University (New York, NY, USA). “Our research provides important support for frontline doctors to help them avoid unnecessarily exposing children to the radiation risks inherent in CT testing.”
The head trauma study was designed by Prof. Kuppermann and colleagues in PECARN to determine which children evaluated in the emergency department for head trauma are at low risk for clinically significant traumatic brain injuries and who do not require cranial CT assessment. The pediatric research network comprises 18 hospital emergency departments across the nation and serves more than 1.2 million children. The immense amount of data generated by this patient population enables investigators to confidently answer questions about best practices, according to the investigators.
Related Links:
University of California, Davis
Boston Children’s Hospital
Pediatric Emergency Care Applied Research Network
Columbia University
Latest Radiography News
- World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
- AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
- Higher Chest X-Ray Usage Catches Lung Cancer Earlier and Improves Survival
- AI-Powered Mammograms Predict Cardiovascular Risk
- Generative AI Model Significantly Reduces Chest X-Ray Reading Time
- AI-Powered Mammography Screening Boosts Cancer Detection in Single-Reader Settings
- Photon Counting Detectors Promise Fast Color X-Ray Images
- AI Can Flag Mammograms for Supplemental MRI
- 3D CT Imaging from Single X-Ray Projection Reduces Radiation Exposure
- AI Method Accurately Predicts Breast Cancer Risk by Analyzing Multiple Mammograms
- Printable Organic X-Ray Sensors Could Transform Treatment for Cancer Patients
- Highly Sensitive, Foldable Detector to Make X-Rays Safer
- Novel Breast Cancer Screening Technology Could Offer Superior Alternative to Mammogram
- Artificial Intelligence Accurately Predicts Breast Cancer Years Before Diagnosis
- AI-Powered Chest X-Ray Detects Pulmonary Nodules Three Years Before Lung Cancer Symptoms
- AI Model Identifies Vertebral Compression Fractures in Chest Radiographs
Channels
MRI
view channel
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read more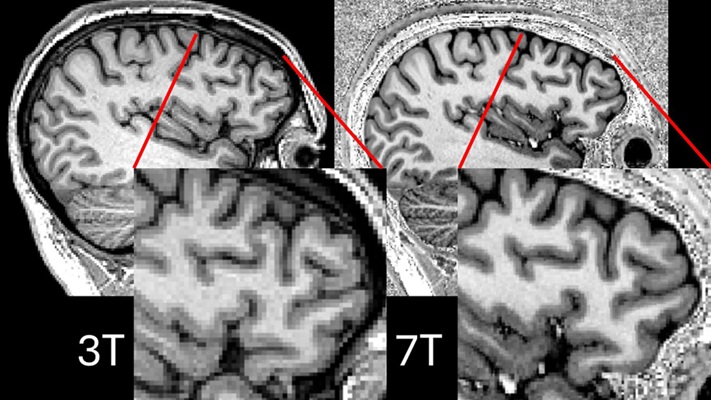
Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
Approximately 360,000 individuals in the UK suffer from focal epilepsy, a condition in which seizures spread from one part of the brain. Around a third of these patients experience persistent seizures... Read more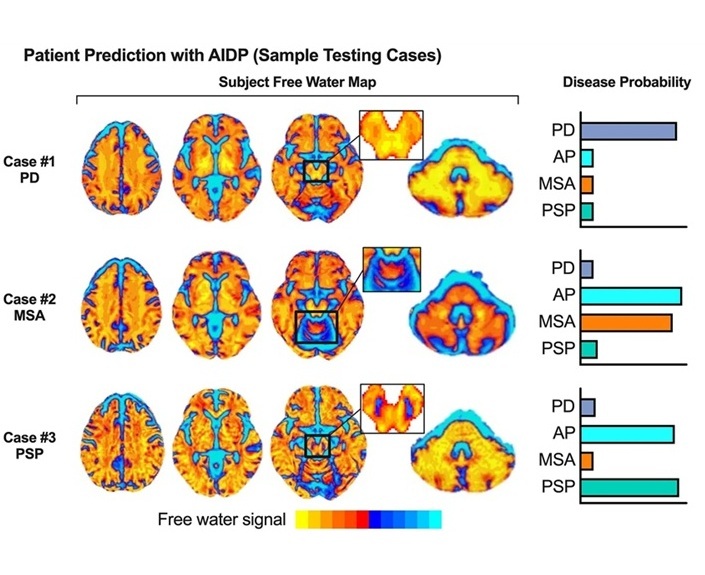
AI-Powered MRI Technology Improves Parkinson’s Diagnoses
Current research shows that the accuracy of diagnosing Parkinson’s disease typically ranges from 55% to 78% within the first five years of assessment. This is partly due to the similarities shared by Parkinson’s... Read more
Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
Artificial intelligence (AI) technologies are transforming the way medical images are analyzed, offering unprecedented capabilities in quantitatively extracting features that go beyond traditional visual... Read moreUltrasound
view channel.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read more
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read moreNuclear Medicine
view channel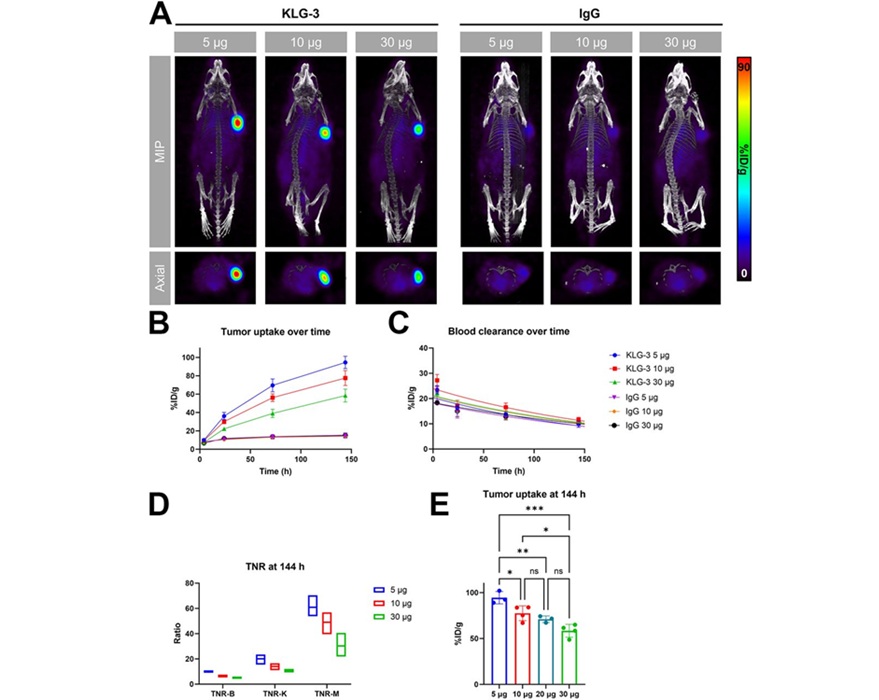
Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
Interleukin-13 receptor α-2 (IL13Rα2) is a cell surface receptor commonly found in solid tumors such as glioblastoma, melanoma, and breast cancer. It is minimally expressed in normal tissues, making it... Read more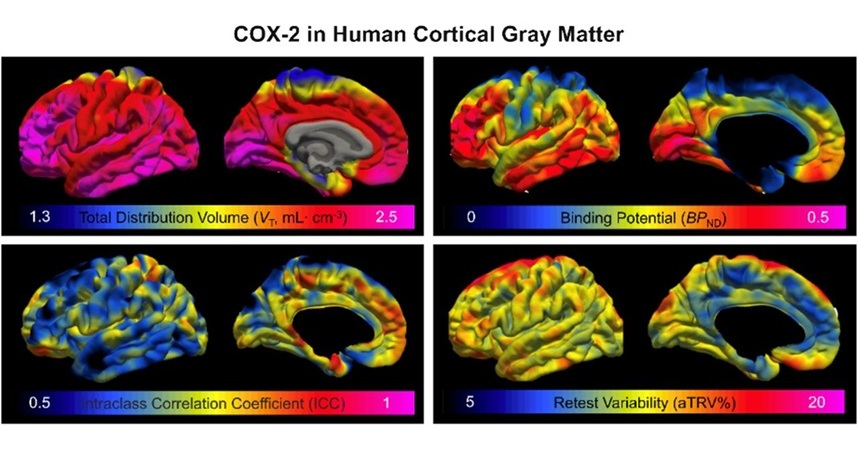
Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
COX-2, an enzyme that plays a key role in brain inflammation, can be significantly upregulated by inflammatory stimuli and neuroexcitation. Researchers suggest that COX-2 density in the brain could serve... Read moreGeneral/Advanced Imaging
view channel
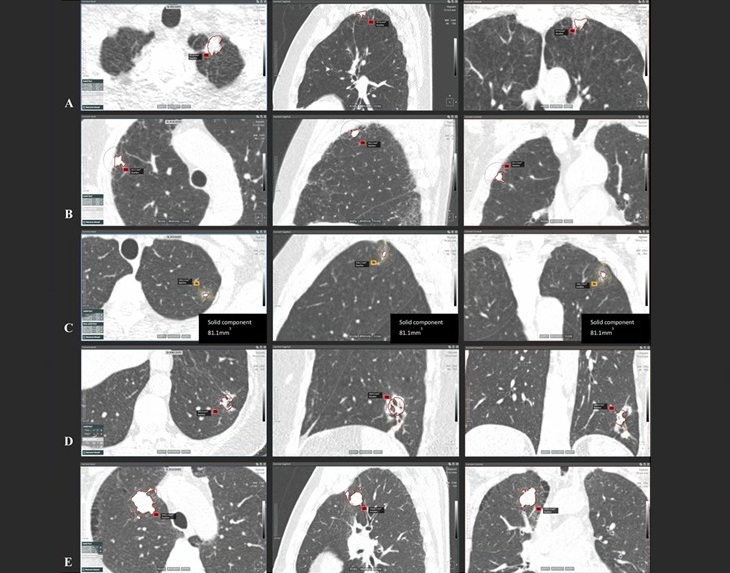
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read more
AI Model Significantly Enhances Low-Dose CT Capabilities
Lung cancer remains one of the most challenging diseases, making early diagnosis vital for effective treatment. Fortunately, advancements in artificial intelligence (AI) are revolutionizing lung cancer... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more