Urologists Criticize Flawed Findings Regarding Prostate Cancer Treatment
|
By MedImaging International staff writers Posted on 12 Nov 2013 |
A US urologic organization advocating for integrated and coordinated urologic care with more than 2,000 physician specialists across the United States has carefully reviewed recent literature regarding intensity-modulated radiation therapy (IMRT) for prostate cancer published in a US medical journal and found it to be methodologically flawed and factually inaccurate, and therefore, does not add to the helpful interchange of ideas needed to enhance healthcare or increase value.
The article, “Urologists’ Use of Intensity-Modulated Radiation Therapy for Prostate Cancer,” authored by Mitchell, JM, was published October 24, 2013, in the New England Journal of Medicine. “The Mitchell study was commissioned and funded by the American Society for Radiation Oncology [ASTRO; Fairfax, VA, USA] in an attempt to persuade lawmakers to legislate a monopoly for its members in the use of radiation therapy to treat prostate cancer—an economically driven agenda that has been rejected by [US] Congress, MedPAC, and the GAO,” said Dr. Deepak A. Kapoor, president of LUGPA (Large Urology Group Practice Association; Schaumburg, IL, USA) and chairman and CEO of Integrated Medical Professionals, PLLC (Melville, NY, USA). “Instead of furthering our understanding of the complicated health policy issues around prostate cancer care, Dr. Mitchell’s work appears to be specifically designed to produce talking points for the sponsor’s political agenda, which is primarily to restore their virtual monopoly on the provision of pathology laboratory services.”
Dr. Mitchell’s data revealed that less than one-third of newly detected prostate cancer patients who sought treatment from an integrated urology group received IMRT. This figure is comparable to data from academic literature that precedes the development of integrated groups. Dr. Mitchell did not match her control group for practice size, patient demographics, or severity of disease—LUGPA spokespersons reported that her selection bias is demonstrated by her own inexplicable results. For example, there has been a distinct national tendency towards less invasive IMRT and away from brachytherapy seen across all US sites of service paradoxically, over the six-year study period, the use of IMRT and brachytherapy remained flat in Dr. Mitchell’s control group. The fact that integrated groups’ rates of active surveillance and surgery held constant additionally shows that ownership of IMRT did not affect these groups’ clinical decision making. “Her own data confirms that urologists with ownership of radiation oncology use the technology appropriately and responsibly. That should be the title of Mitchell’s study,” said Dr. Kapoor.
The ASTRO study serves only one purpose, according to LUGPA spokespersons—to undermine competition in the market place. Utilizing such inaccurate data that demonizes groups practicing evidence-based medicine in an attempt to manipulate market share by legislative fiat is both inappropriate and offensive, according to LUGPA. Legislative changes based on such false data will drive up costs, as many patients will be forced to seek care in the more expensive hospital setting, and harm patient access to specialized, integrated care.
LUGPA represents 121 large urology group practices in the United States, with more than 2,000 physicians who comprise more than 20% of the US practicing urologists. LUGPA and its member practices are focused on best practices, data collection, research, and benchmarking to promote quality clinical outcomes.
Related Links:
Large Urology Group Practice Association
American Society for Radiation Oncology
The article, “Urologists’ Use of Intensity-Modulated Radiation Therapy for Prostate Cancer,” authored by Mitchell, JM, was published October 24, 2013, in the New England Journal of Medicine. “The Mitchell study was commissioned and funded by the American Society for Radiation Oncology [ASTRO; Fairfax, VA, USA] in an attempt to persuade lawmakers to legislate a monopoly for its members in the use of radiation therapy to treat prostate cancer—an economically driven agenda that has been rejected by [US] Congress, MedPAC, and the GAO,” said Dr. Deepak A. Kapoor, president of LUGPA (Large Urology Group Practice Association; Schaumburg, IL, USA) and chairman and CEO of Integrated Medical Professionals, PLLC (Melville, NY, USA). “Instead of furthering our understanding of the complicated health policy issues around prostate cancer care, Dr. Mitchell’s work appears to be specifically designed to produce talking points for the sponsor’s political agenda, which is primarily to restore their virtual monopoly on the provision of pathology laboratory services.”
Dr. Mitchell’s data revealed that less than one-third of newly detected prostate cancer patients who sought treatment from an integrated urology group received IMRT. This figure is comparable to data from academic literature that precedes the development of integrated groups. Dr. Mitchell did not match her control group for practice size, patient demographics, or severity of disease—LUGPA spokespersons reported that her selection bias is demonstrated by her own inexplicable results. For example, there has been a distinct national tendency towards less invasive IMRT and away from brachytherapy seen across all US sites of service paradoxically, over the six-year study period, the use of IMRT and brachytherapy remained flat in Dr. Mitchell’s control group. The fact that integrated groups’ rates of active surveillance and surgery held constant additionally shows that ownership of IMRT did not affect these groups’ clinical decision making. “Her own data confirms that urologists with ownership of radiation oncology use the technology appropriately and responsibly. That should be the title of Mitchell’s study,” said Dr. Kapoor.
The ASTRO study serves only one purpose, according to LUGPA spokespersons—to undermine competition in the market place. Utilizing such inaccurate data that demonizes groups practicing evidence-based medicine in an attempt to manipulate market share by legislative fiat is both inappropriate and offensive, according to LUGPA. Legislative changes based on such false data will drive up costs, as many patients will be forced to seek care in the more expensive hospital setting, and harm patient access to specialized, integrated care.
LUGPA represents 121 large urology group practices in the United States, with more than 2,000 physicians who comprise more than 20% of the US practicing urologists. LUGPA and its member practices are focused on best practices, data collection, research, and benchmarking to promote quality clinical outcomes.
Related Links:
Large Urology Group Practice Association
American Society for Radiation Oncology
Latest Nuclear Medicine News
- Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
- Combining Advanced Imaging Technologies Offers Breakthrough in Glioblastoma Treatment
- New Molecular Imaging Agent Accurately Identifies Crucial Cancer Biomarker
- New Scans Light Up Aggressive Tumors for Better Treatment
- AI Stroke Brain Scan Readings Twice as Accurate as Current Method
- AI Analysis of PET/CT Images Predicts Side Effects of Immunotherapy in Lung Cancer
- New Imaging Agent to Drive Step-Change for Brain Cancer Imaging
- Portable PET Scanner to Detect Earliest Stages of Alzheimer’s Disease
Channels
Radiography
view channel
AI Improves Early Detection of Interval Breast Cancers
Interval breast cancers, which occur between routine screenings, are easier to treat when detected earlier. Early detection can reduce the need for aggressive treatments and improve the chances of better outcomes.... Read more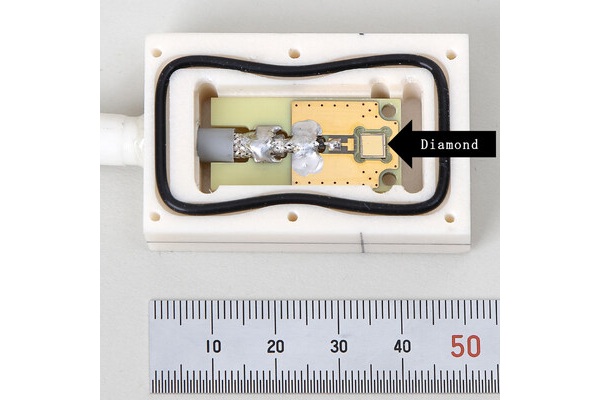
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read moreMRI
view channel
Cutting-Edge MRI Technology to Revolutionize Diagnosis of Common Heart Problem
Aortic stenosis is a common and potentially life-threatening heart condition. It occurs when the aortic valve, which regulates blood flow from the heart to the rest of the body, becomes stiff and narrow.... Read more
New MRI Technique Reveals True Heart Age to Prevent Attacks and Strokes
Heart disease remains one of the leading causes of death worldwide. Individuals with conditions such as diabetes or obesity often experience accelerated aging of their hearts, sometimes by decades.... Read more
AI Tool Predicts Relapse of Pediatric Brain Cancer from Brain MRI Scans
Many pediatric gliomas are treatable with surgery alone, but relapses can be catastrophic. Predicting which patients are at risk for recurrence remains challenging, leading to frequent follow-ups with... Read more
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read moreUltrasound
view channel.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read more
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read moreGeneral/Advanced Imaging
view channel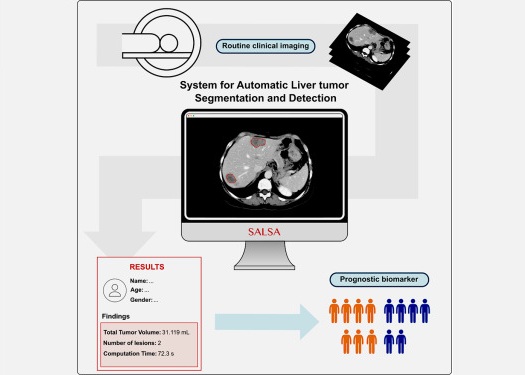
CT-Based Deep Learning-Driven Tool to Enhance Liver Cancer Diagnosis
Medical imaging, such as computed tomography (CT) scans, plays a crucial role in oncology, offering essential data for cancer detection, treatment planning, and monitoring of response to therapies.... Read more
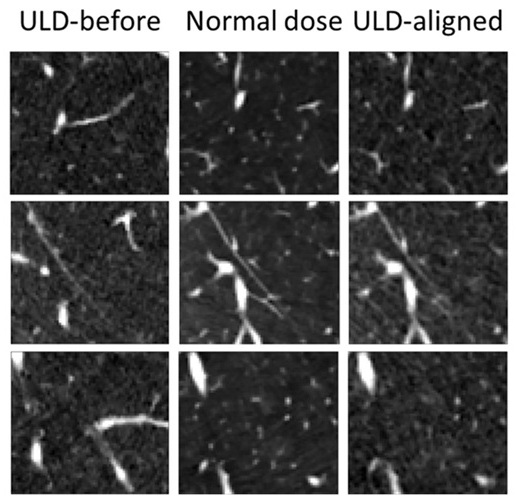
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more