Reduced High-Dose Volume Radiotherapy for Bladder Cancer Has Less Toxicity
|
By MedImaging International staff writers Posted on 29 Oct 2013 |
Conventional and reduced high-dose volume radiation therapy (RHDVRT) for muscle-invasive bladder cancer provide similar tumor control and decreased late toxicity when compared to surgery.
The findings were published October 2013, in the International Journal of Radiation Oncology-Biology-Physics, the scientific journal of the American Society for Radiation Oncology (ASTRO). The research is part of the United Kingdom’s BC2001 clinical trial, one of the largest randomized trials conducted involving radiation therapy (RT) in patients with muscle-invasive bladder cancer.
Cystectomy (partial or whole bladder removal surgery) is often the standard treatment for patients with muscle-invasive bladder cancer; however, advanced RT techniques that spare the bladder may be an effective alternative for patients who are unsuitable for or unwilling to undergo cystectomy. This research was done to determine if some of the disadvantages of RT of the bladder, such as late toxicity risks and local recurrence, could be reduced with a lower dose of RT being delivered to the areas of the bladder outside of the tumor region, and to assess the tumor control and toxicity of RT.
This phase III randomized trial was sponsored by the University of Birmingham (UK), supported by Cancer Research UK, and facilitated by the UK National Institute for Health Research Cancer Research Network. The cohort of participants for this part of the trial included 219 patients from 28 centers across the United Kingdom who received either standard radiation therapy or reduced high-volume radiation therapy. Patients were all age 18 and older and had stage T2 -T4a bladder cancer. Study participants were randomized: 108 received standard whole bladder radiation therapy (sRT) and the remaining 111 patients received RHDVRT, in which the full radiation dose was delivered to the tumor and 80% of the maximum dose was delivered to the uninvolved bladder.
Study participants received RT doses based on their cancer center’s choice of either 55 Gy/20 fractions over four weeks or 64 Gy/32 fractions over 6.5 weeks. For patients in the sRT group, the planning target volume (PTV) was the outer bladder wall, plus the extravesical extent of the tumor with a 1.5-cm margin. For patients in the RHDVRT group, two PTVs were defined: PTV1, as in the sRT group, and PTV2, as the gross tumor volume plus a 1.5 cm margin.
Patients were assessed weekly throughout treatment for toxicity; and side effects were measured at 6, 9, and 12 months post-treatment, and annually thereafter. Furthermore, tumor control was evaluated at 6, 9, and 12 months after treatment and then yearly for up to five years. The median patient follow-up time was 72.7 months post-treatment.
In this radiation-therapy volume comparison of the study, the primary endpoints of interest were late toxicity and local control. Late toxicity was determined in this study to be radiation therapy-related side effects at least one to two years post-treatment. The Radiation Therapy Oncology Group (RTOG) scale and Late Effects of Normal Tissue (Subjective, Objective, Management) (LENT/SOM) scale were utilized to gauge late toxicity in study participants. Rates of late toxicity were lower than expected, and the number of patients reporting RTOG or LENT/SOM toxicities (side effects) was not substantially different between the sRT and RHDVRT groups. The overall cumulative grades 3/4 RTOG toxicity rate was 13% at two years post-treatment, and the percentage of patients with grades 3/4 toxicity at any specific point was shown to be < 8% throughout in both groups.
Two-year locoregional recurrence free (LRRF) rate was 61% for the sRT group and 64% for the RHDVRT group, but noninferiority of locoregional control (validation that the RHDVRT treatment was at least not noticeably inferior than the sRT treatment) could not be properly determined in the study.
“We have now demonstrated that delivering at least 75% of the dose [of RT] to the uninvolved bladder is deliverable across multiple sites without obvious detriment to local disease control or survival, although noninferiority could not be formally confirmed,” said lead author Robert A. Huddart, PhD, of the Institute of Cancer Research (London, UK) and the Royal Marsden NHS [National Health Service] Foundation Trust (London, UK). “These results confirm, however, that RT is an effective alternative for patients unable to undergo cystectomy. Further study using image-guided treatment with or without dose escalation is now also warranted.”
Related Links:
University of Birmingham
Institute of Cancer Research
Royal Marsden NHS Foundation Trust
The findings were published October 2013, in the International Journal of Radiation Oncology-Biology-Physics, the scientific journal of the American Society for Radiation Oncology (ASTRO). The research is part of the United Kingdom’s BC2001 clinical trial, one of the largest randomized trials conducted involving radiation therapy (RT) in patients with muscle-invasive bladder cancer.
Cystectomy (partial or whole bladder removal surgery) is often the standard treatment for patients with muscle-invasive bladder cancer; however, advanced RT techniques that spare the bladder may be an effective alternative for patients who are unsuitable for or unwilling to undergo cystectomy. This research was done to determine if some of the disadvantages of RT of the bladder, such as late toxicity risks and local recurrence, could be reduced with a lower dose of RT being delivered to the areas of the bladder outside of the tumor region, and to assess the tumor control and toxicity of RT.
This phase III randomized trial was sponsored by the University of Birmingham (UK), supported by Cancer Research UK, and facilitated by the UK National Institute for Health Research Cancer Research Network. The cohort of participants for this part of the trial included 219 patients from 28 centers across the United Kingdom who received either standard radiation therapy or reduced high-volume radiation therapy. Patients were all age 18 and older and had stage T2 -T4a bladder cancer. Study participants were randomized: 108 received standard whole bladder radiation therapy (sRT) and the remaining 111 patients received RHDVRT, in which the full radiation dose was delivered to the tumor and 80% of the maximum dose was delivered to the uninvolved bladder.
Study participants received RT doses based on their cancer center’s choice of either 55 Gy/20 fractions over four weeks or 64 Gy/32 fractions over 6.5 weeks. For patients in the sRT group, the planning target volume (PTV) was the outer bladder wall, plus the extravesical extent of the tumor with a 1.5-cm margin. For patients in the RHDVRT group, two PTVs were defined: PTV1, as in the sRT group, and PTV2, as the gross tumor volume plus a 1.5 cm margin.
Patients were assessed weekly throughout treatment for toxicity; and side effects were measured at 6, 9, and 12 months post-treatment, and annually thereafter. Furthermore, tumor control was evaluated at 6, 9, and 12 months after treatment and then yearly for up to five years. The median patient follow-up time was 72.7 months post-treatment.
In this radiation-therapy volume comparison of the study, the primary endpoints of interest were late toxicity and local control. Late toxicity was determined in this study to be radiation therapy-related side effects at least one to two years post-treatment. The Radiation Therapy Oncology Group (RTOG) scale and Late Effects of Normal Tissue (Subjective, Objective, Management) (LENT/SOM) scale were utilized to gauge late toxicity in study participants. Rates of late toxicity were lower than expected, and the number of patients reporting RTOG or LENT/SOM toxicities (side effects) was not substantially different between the sRT and RHDVRT groups. The overall cumulative grades 3/4 RTOG toxicity rate was 13% at two years post-treatment, and the percentage of patients with grades 3/4 toxicity at any specific point was shown to be < 8% throughout in both groups.
Two-year locoregional recurrence free (LRRF) rate was 61% for the sRT group and 64% for the RHDVRT group, but noninferiority of locoregional control (validation that the RHDVRT treatment was at least not noticeably inferior than the sRT treatment) could not be properly determined in the study.
“We have now demonstrated that delivering at least 75% of the dose [of RT] to the uninvolved bladder is deliverable across multiple sites without obvious detriment to local disease control or survival, although noninferiority could not be formally confirmed,” said lead author Robert A. Huddart, PhD, of the Institute of Cancer Research (London, UK) and the Royal Marsden NHS [National Health Service] Foundation Trust (London, UK). “These results confirm, however, that RT is an effective alternative for patients unable to undergo cystectomy. Further study using image-guided treatment with or without dose escalation is now also warranted.”
Related Links:
University of Birmingham
Institute of Cancer Research
Royal Marsden NHS Foundation Trust
Latest Nuclear Medicine News
- Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
- Combining Advanced Imaging Technologies Offers Breakthrough in Glioblastoma Treatment
- New Molecular Imaging Agent Accurately Identifies Crucial Cancer Biomarker
- New Scans Light Up Aggressive Tumors for Better Treatment
- AI Stroke Brain Scan Readings Twice as Accurate as Current Method
- AI Analysis of PET/CT Images Predicts Side Effects of Immunotherapy in Lung Cancer
- New Imaging Agent to Drive Step-Change for Brain Cancer Imaging
- Portable PET Scanner to Detect Earliest Stages of Alzheimer’s Disease
Channels
Radiography
view channel
AI Improves Early Detection of Interval Breast Cancers
Interval breast cancers, which occur between routine screenings, are easier to treat when detected earlier. Early detection can reduce the need for aggressive treatments and improve the chances of better outcomes.... Read more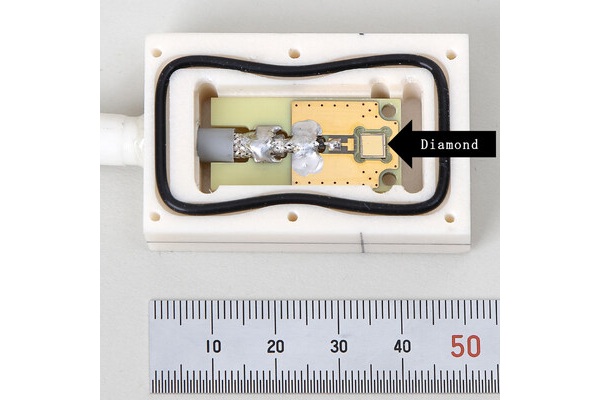
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read moreMRI
view channel
Cutting-Edge MRI Technology to Revolutionize Diagnosis of Common Heart Problem
Aortic stenosis is a common and potentially life-threatening heart condition. It occurs when the aortic valve, which regulates blood flow from the heart to the rest of the body, becomes stiff and narrow.... Read more
New MRI Technique Reveals True Heart Age to Prevent Attacks and Strokes
Heart disease remains one of the leading causes of death worldwide. Individuals with conditions such as diabetes or obesity often experience accelerated aging of their hearts, sometimes by decades.... Read more
AI Tool Predicts Relapse of Pediatric Brain Cancer from Brain MRI Scans
Many pediatric gliomas are treatable with surgery alone, but relapses can be catastrophic. Predicting which patients are at risk for recurrence remains challenging, leading to frequent follow-ups with... Read more
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read moreUltrasound
view channel.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read more
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read moreGeneral/Advanced Imaging
view channel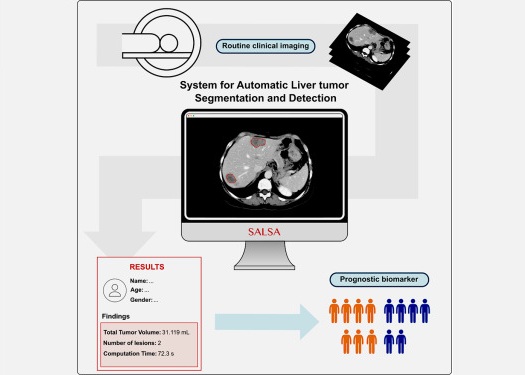
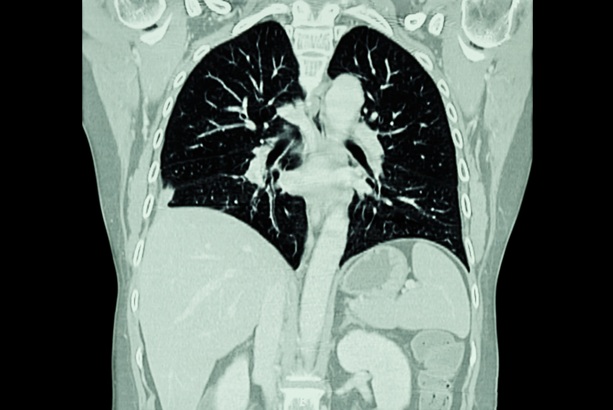
CT-Based Deep Learning-Driven Tool to Enhance Liver Cancer Diagnosis
Medical imaging, such as computed tomography (CT) scans, plays a crucial role in oncology, offering essential data for cancer detection, treatment planning, and monitoring of response to therapies.... Read more
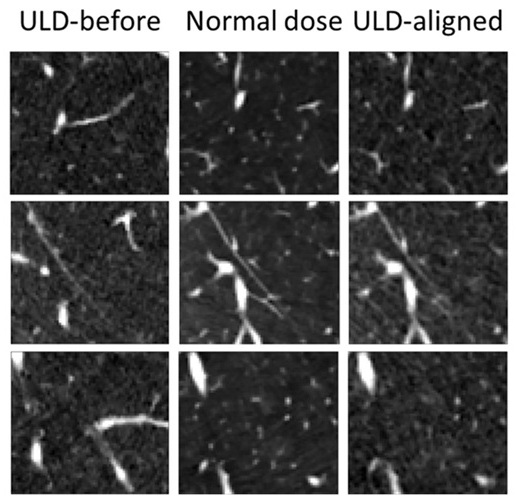
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more