Physicians Avoid Online Error-Reporting Tools Because of Embarrassment
|
By MedImaging International staff writers Posted on 25 Oct 2011 |
“Too busy,” and “too complicated” are the typical excuses one might expect when medical professionals are asked why they fail to use online error-reporting systems designed to improve patient safety and the quality of care. But investigators found instead that the most typical reason among radiation oncologists was fear of getting into trouble and embarrassment.
Johns Hopkins University (Baltimore, MD, USA) investigators e-mailed an anonymous survey to physicians, nurses, radiation physicists and other radiation specialists at Johns Hopkins University, North Shore-Long Island Jewish Health System (Great Neck, NY, USA), Washington University in St. Louis (MO, USA), and the University of Miami (FL, USA), with questions about their reporting near-misses and errors in delivering radiotherapy. Each of the four centers tracks near misses and errors through online, intradepartmental systems. Some 274 providers returned completed surveys.
According to the survey, few nurses and physicians reported routinely submitting online reports, in contrast to physicists, dosimetrists, and radiation therapists who reported the most use of error and near-miss reporting systems. Almost all respondents agreed that error reporting is their responsibility. Getting colleagues into trouble, liability and embarrassment in front of colleagues were reported most frequently by physicians and residents.
More than 90% of respondents had observed near misses or errors in their clinical practice. The vast majority of these were reported as near misses as opposed to errors, and, as a result, no providers reported patient harm. Hospitals have specific systems for reporting errors, but few have systems to accommodate the complex data associated with radiotherapy.
“It is important to understand the specific reasons why fewer physicians participate in these reporting systems so that hospitals can work to close this gap. Reporting is not an end in itself. It helps identify potential hazards, and each member of the health care team brings a perspective that can help make patients safer,” said Johns Hopkins radiation oncology resident Kendra Harris, MD, who presented an abstract of the data at the 53rd annual meeting of the American Society for Radiation Oncology (ASTRO), held October 2011 in Miami, FL, USA.
The up side, according to Dr. Harris, is that few respondents reported being too busy to report or that the online tool was too complicated. “Respondents recognized that error events should be reported and that they should claim responsibility for them. The barriers we identified are not insurmountable,” she added.
Dr. Harris reported that online reporting systems should be simple and promoted as quality improvement tools, not instruments for placing blame and meting out sanctions. “These systems should not be viewed as punitive; rather, they’re a critical way to improve therapy,” she stated. “You can’t manage what you can’t measure.”
Most of the respondents said they would participate in a national reporting system for radiotherapy near misses and errors. “A national system that collects pooled data about near-misses and errors, which are thankfully rare, may help us identify common trends and implement safety interventions to improve care,” added Dr. Harris.
Related Links:
Johns Hopkins University
Johns Hopkins University (Baltimore, MD, USA) investigators e-mailed an anonymous survey to physicians, nurses, radiation physicists and other radiation specialists at Johns Hopkins University, North Shore-Long Island Jewish Health System (Great Neck, NY, USA), Washington University in St. Louis (MO, USA), and the University of Miami (FL, USA), with questions about their reporting near-misses and errors in delivering radiotherapy. Each of the four centers tracks near misses and errors through online, intradepartmental systems. Some 274 providers returned completed surveys.
According to the survey, few nurses and physicians reported routinely submitting online reports, in contrast to physicists, dosimetrists, and radiation therapists who reported the most use of error and near-miss reporting systems. Almost all respondents agreed that error reporting is their responsibility. Getting colleagues into trouble, liability and embarrassment in front of colleagues were reported most frequently by physicians and residents.
More than 90% of respondents had observed near misses or errors in their clinical practice. The vast majority of these were reported as near misses as opposed to errors, and, as a result, no providers reported patient harm. Hospitals have specific systems for reporting errors, but few have systems to accommodate the complex data associated with radiotherapy.
“It is important to understand the specific reasons why fewer physicians participate in these reporting systems so that hospitals can work to close this gap. Reporting is not an end in itself. It helps identify potential hazards, and each member of the health care team brings a perspective that can help make patients safer,” said Johns Hopkins radiation oncology resident Kendra Harris, MD, who presented an abstract of the data at the 53rd annual meeting of the American Society for Radiation Oncology (ASTRO), held October 2011 in Miami, FL, USA.
The up side, according to Dr. Harris, is that few respondents reported being too busy to report or that the online tool was too complicated. “Respondents recognized that error events should be reported and that they should claim responsibility for them. The barriers we identified are not insurmountable,” she added.
Dr. Harris reported that online reporting systems should be simple and promoted as quality improvement tools, not instruments for placing blame and meting out sanctions. “These systems should not be viewed as punitive; rather, they’re a critical way to improve therapy,” she stated. “You can’t manage what you can’t measure.”
Most of the respondents said they would participate in a national reporting system for radiotherapy near misses and errors. “A national system that collects pooled data about near-misses and errors, which are thankfully rare, may help us identify common trends and implement safety interventions to improve care,” added Dr. Harris.
Related Links:
Johns Hopkins University
Latest Imaging IT News
- New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
- Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
- AI-Based Mammography Triage Software Helps Dramatically Improve Interpretation Process
- Artificial Intelligence (AI) Program Accurately Predicts Lung Cancer Risk from CT Images
- Image Management Platform Streamlines Treatment Plans
- AI-Based Technology for Ultrasound Image Analysis Receives FDA Approval
- AI Technology for Detecting Breast Cancer Receives CE Mark Approval
- Digital Pathology Software Improves Workflow Efficiency
- Patient-Centric Portal Facilitates Direct Imaging Access
- New Workstation Supports Customer-Driven Imaging Workflow
Channels
Radiography
view channel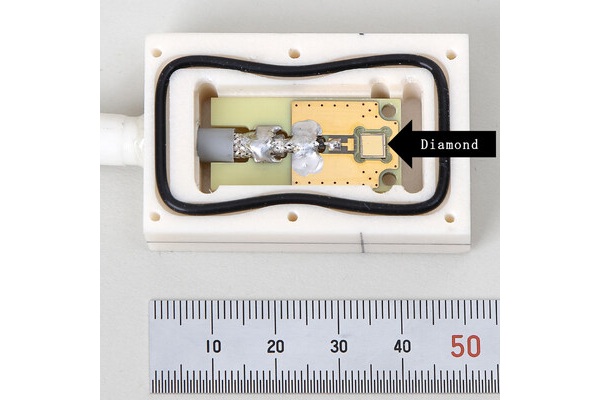
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read more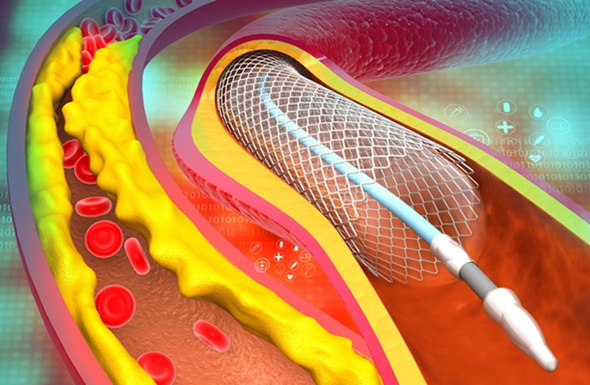
AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure where small metal tubes called stents are inserted into partially blocked coronary arteries... Read moreMRI
view channel
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read more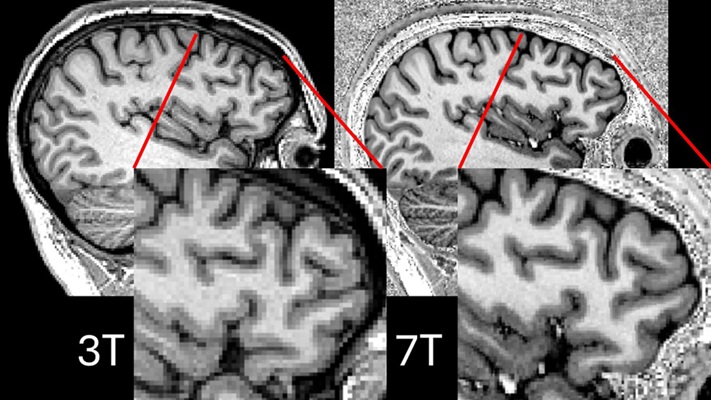
Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
Approximately 360,000 individuals in the UK suffer from focal epilepsy, a condition in which seizures spread from one part of the brain. Around a third of these patients experience persistent seizures... Read more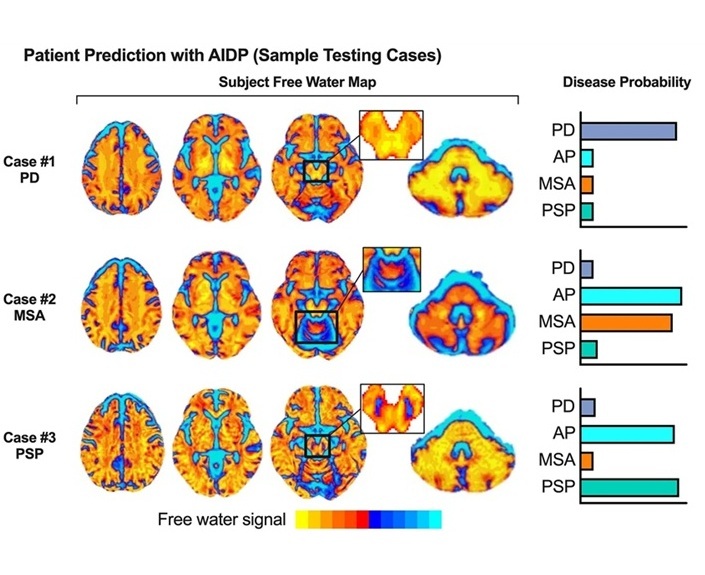
AI-Powered MRI Technology Improves Parkinson’s Diagnoses
Current research shows that the accuracy of diagnosing Parkinson’s disease typically ranges from 55% to 78% within the first five years of assessment. This is partly due to the similarities shared by Parkinson’s... Read more
Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
Artificial intelligence (AI) technologies are transforming the way medical images are analyzed, offering unprecedented capabilities in quantitatively extracting features that go beyond traditional visual... Read moreUltrasound
view channel.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read more
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read moreNuclear Medicine
view channel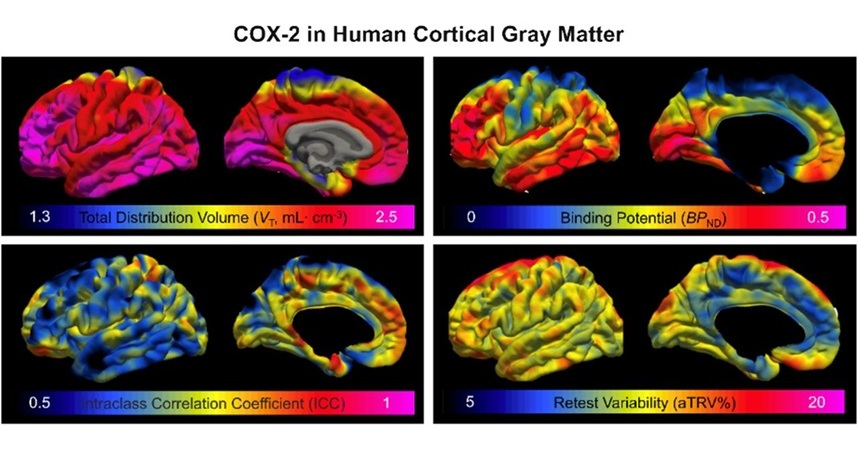
Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
COX-2, an enzyme that plays a key role in brain inflammation, can be significantly upregulated by inflammatory stimuli and neuroexcitation. Researchers suggest that COX-2 density in the brain could serve... Read more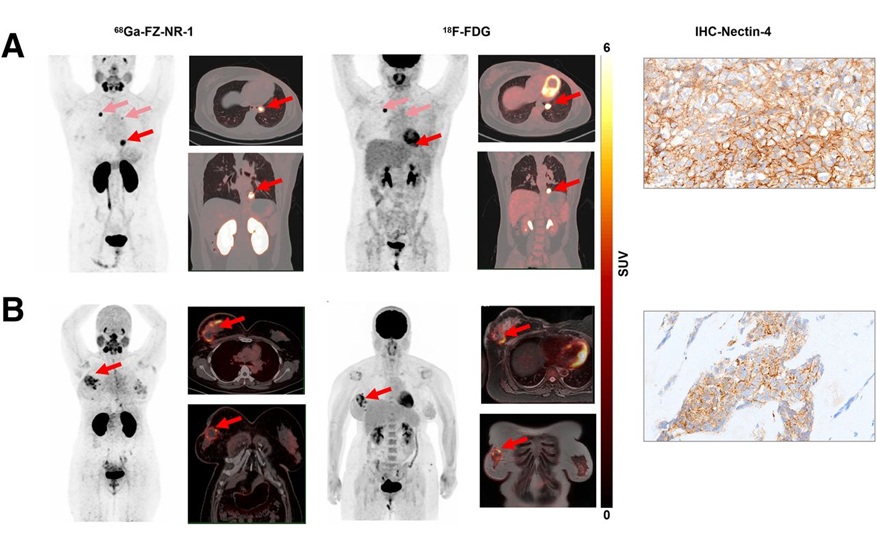
Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC), which represents 15-20% of all breast cancer cases, is one of the most aggressive subtypes, with a five-year survival rate of about 40%. Due to its significant heterogeneity... Read moreGeneral/Advanced Imaging
view channel
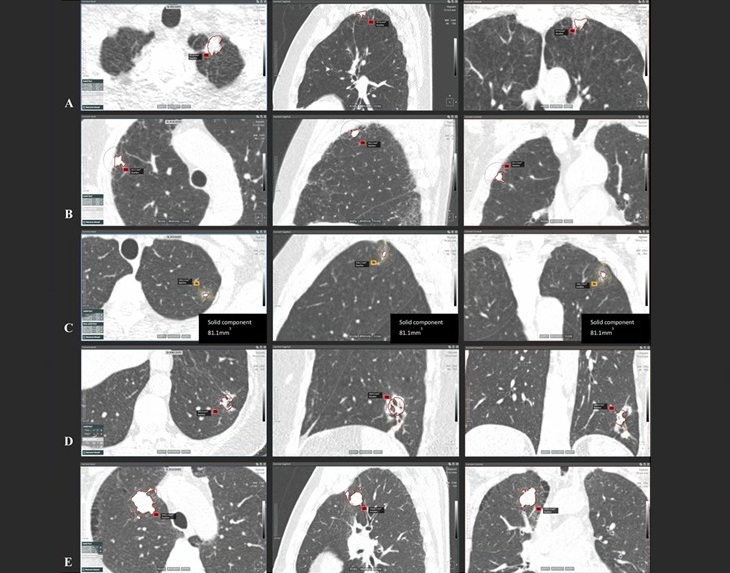
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read more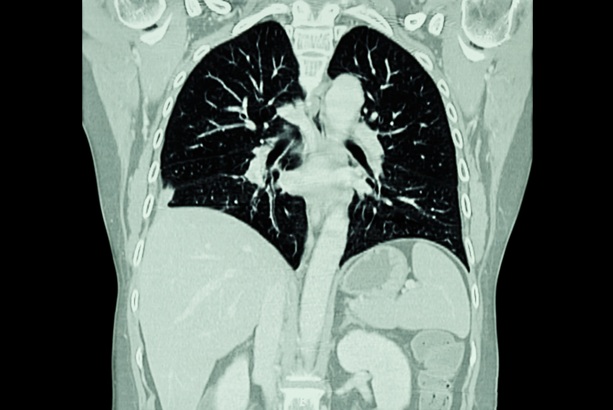
AI Model Significantly Enhances Low-Dose CT Capabilities
Lung cancer remains one of the most challenging diseases, making early diagnosis vital for effective treatment. Fortunately, advancements in artificial intelligence (AI) are revolutionizing lung cancer... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more