Intraoperative Radiotherapy May Offer Faster, More Precise Treatment for Breast Cancer
|
By MedImaging International staff writers Posted on 26 Apr 2011 |
Clinicians are currently utilizing a new treatment option for breast cancer that allows women to receive a full dose of radiation therapy during breast-conserving surgery.
Conventionally, women who opt to have a lumpectomy must first have surgery then undergo about six weeks of radiation. This schedule can be challenging for women who have busy schedules or do not have access to a center offering radiation therapy. In some instances, the demanding schedule causes women not to comply with the recommended course of treatment, increasing their risk for cancer recurrence. Intraoperative radiation therapy combines lumpectomy and the full course of radiation during a two and half hour operation.
"With this technique, the radiation oncologist will be in the operating room administering radiation to the tumor bed immediately following the surgeon's removal of the tumor," said William Small, Jr., MD, vice chairman radiation oncology at Northwestern Memorial Hospital and professor of radiation oncology at Northwestern University Feinberg School of Medicine (Chicago, IL, USA). "Instead of waiting a month to start the radiation therapy, it will take place immediately. A patient will wake up from surgery and have received the full amount of radiation therapy that is typically administered over six weeks."
Currently, a breast cancer patient first sees a surgeon to remove the tumor and then she is referred to a radiation oncologist for follow up radiotherapy. Intraoperative radiation therapy allows physicians to deliver radiotherapy at the time of surgery directly to the area where the cancer was removed. Using a system called IntraBeam, manufactured by Carl Zeiss (Oberkochen, Germany), the radiation oncologist is now able to be in the operating room with the surgical oncologist, delivering the entire dose of radiation during surgery. A large international randomized trial confirmed that delivering radiation at the time of lumpectomy was as effective in preventing breast cancer recurrence as whole breast radiation therapy in selected patients (WBRT).
Not all patients who choose lumpectomy comply with the recommended follow up treatment because of factors including time, costs, distance, and access to a treatment facility. Disregarding follow-up radiation after lumpectomy can increase the risk of cancer recurrence. Intraoperative radiation considerably decreases treatment time and allows women to complete radiation and surgery at the same time.
"By eliminating the geographic and time constraints of traditional radiotherapy, intraoperative radiation can make breast conservation surgery a realistic option for more women," said Kevin Bethke, MD, surgical oncologist at Northwestern Memorial and assistant professor of clinical surgery at the Feinberg School. "Active women with busy jobs can choose lumpectomy and comply with the recommended radiation therapy, but limit the impact the treatment has on their lives."
Combined with offering an expedited treatment schedule, intraoperative radiation therapy also has the potential for better cosmetic outcomes, including less scarring, and fewer side effects compared to those associated with WBRT. Skin reactions, including redness, rashes, and irritation, as well as more severe complications including fatigue, swelling, tissue stiffness, and scarring are sometimes associated with traditional radiation therapy.
While early findings indicate single-dose radiation is as effective as WBRT in limiting recurrence of breast cancer in selected patients, it is not an option for every breast cancer diagnosis. Currently, only women with early stage breast cancer are considered as candidates for intraoperative radiation therapy.
"This isn't a replacement for traditional breast cancer treatment, but for the right candidate it may be an attractive alternative," said Dr. Small. "This has potential to expand access to radiation therapy allowing more women to comply with the recommended course of treatment. Hopefully, with a more concise and convenient treatment available, a broader group of women will have the option to choose breast-conserving treatment options."
The physicians hope that by offering intraoperative radiation therapy, they can help their patients effectively treat their cancer, but also do so in a manner that minimizes its impact on their daily lives. "A cancer diagnosis can be extremely stressful for a patient, so it's important that treatment is not," noted Dr. Bethke. "With this new option, we're giving women a way to treat their disease while continuing to live a normal, active life."
Related Links:
Northwestern University Feinberg School of Medicine
Carl Zeiss
Conventionally, women who opt to have a lumpectomy must first have surgery then undergo about six weeks of radiation. This schedule can be challenging for women who have busy schedules or do not have access to a center offering radiation therapy. In some instances, the demanding schedule causes women not to comply with the recommended course of treatment, increasing their risk for cancer recurrence. Intraoperative radiation therapy combines lumpectomy and the full course of radiation during a two and half hour operation.
"With this technique, the radiation oncologist will be in the operating room administering radiation to the tumor bed immediately following the surgeon's removal of the tumor," said William Small, Jr., MD, vice chairman radiation oncology at Northwestern Memorial Hospital and professor of radiation oncology at Northwestern University Feinberg School of Medicine (Chicago, IL, USA). "Instead of waiting a month to start the radiation therapy, it will take place immediately. A patient will wake up from surgery and have received the full amount of radiation therapy that is typically administered over six weeks."
Currently, a breast cancer patient first sees a surgeon to remove the tumor and then she is referred to a radiation oncologist for follow up radiotherapy. Intraoperative radiation therapy allows physicians to deliver radiotherapy at the time of surgery directly to the area where the cancer was removed. Using a system called IntraBeam, manufactured by Carl Zeiss (Oberkochen, Germany), the radiation oncologist is now able to be in the operating room with the surgical oncologist, delivering the entire dose of radiation during surgery. A large international randomized trial confirmed that delivering radiation at the time of lumpectomy was as effective in preventing breast cancer recurrence as whole breast radiation therapy in selected patients (WBRT).
Not all patients who choose lumpectomy comply with the recommended follow up treatment because of factors including time, costs, distance, and access to a treatment facility. Disregarding follow-up radiation after lumpectomy can increase the risk of cancer recurrence. Intraoperative radiation considerably decreases treatment time and allows women to complete radiation and surgery at the same time.
"By eliminating the geographic and time constraints of traditional radiotherapy, intraoperative radiation can make breast conservation surgery a realistic option for more women," said Kevin Bethke, MD, surgical oncologist at Northwestern Memorial and assistant professor of clinical surgery at the Feinberg School. "Active women with busy jobs can choose lumpectomy and comply with the recommended radiation therapy, but limit the impact the treatment has on their lives."
Combined with offering an expedited treatment schedule, intraoperative radiation therapy also has the potential for better cosmetic outcomes, including less scarring, and fewer side effects compared to those associated with WBRT. Skin reactions, including redness, rashes, and irritation, as well as more severe complications including fatigue, swelling, tissue stiffness, and scarring are sometimes associated with traditional radiation therapy.
While early findings indicate single-dose radiation is as effective as WBRT in limiting recurrence of breast cancer in selected patients, it is not an option for every breast cancer diagnosis. Currently, only women with early stage breast cancer are considered as candidates for intraoperative radiation therapy.
"This isn't a replacement for traditional breast cancer treatment, but for the right candidate it may be an attractive alternative," said Dr. Small. "This has potential to expand access to radiation therapy allowing more women to comply with the recommended course of treatment. Hopefully, with a more concise and convenient treatment available, a broader group of women will have the option to choose breast-conserving treatment options."
The physicians hope that by offering intraoperative radiation therapy, they can help their patients effectively treat their cancer, but also do so in a manner that minimizes its impact on their daily lives. "A cancer diagnosis can be extremely stressful for a patient, so it's important that treatment is not," noted Dr. Bethke. "With this new option, we're giving women a way to treat their disease while continuing to live a normal, active life."
Related Links:
Northwestern University Feinberg School of Medicine
Carl Zeiss
Latest Nuclear Medicine News
- Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
- Combining Advanced Imaging Technologies Offers Breakthrough in Glioblastoma Treatment
- New Molecular Imaging Agent Accurately Identifies Crucial Cancer Biomarker
- New Scans Light Up Aggressive Tumors for Better Treatment
- AI Stroke Brain Scan Readings Twice as Accurate as Current Method
- AI Analysis of PET/CT Images Predicts Side Effects of Immunotherapy in Lung Cancer
- New Imaging Agent to Drive Step-Change for Brain Cancer Imaging
- Portable PET Scanner to Detect Earliest Stages of Alzheimer’s Disease
Channels
Radiography
view channel
AI Improves Early Detection of Interval Breast Cancers
Interval breast cancers, which occur between routine screenings, are easier to treat when detected earlier. Early detection can reduce the need for aggressive treatments and improve the chances of better outcomes.... Read more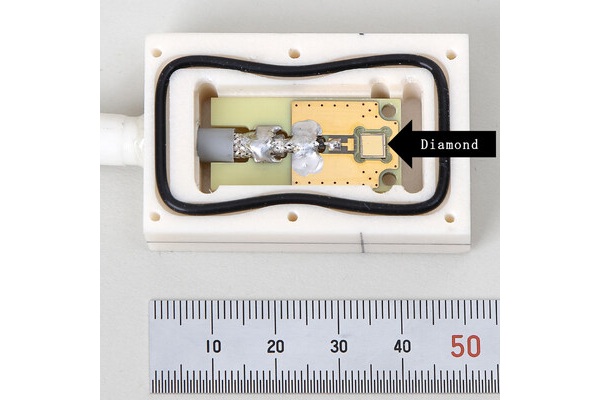
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read moreMRI
view channel
Cutting-Edge MRI Technology to Revolutionize Diagnosis of Common Heart Problem
Aortic stenosis is a common and potentially life-threatening heart condition. It occurs when the aortic valve, which regulates blood flow from the heart to the rest of the body, becomes stiff and narrow.... Read more
New MRI Technique Reveals True Heart Age to Prevent Attacks and Strokes
Heart disease remains one of the leading causes of death worldwide. Individuals with conditions such as diabetes or obesity often experience accelerated aging of their hearts, sometimes by decades.... Read more
AI Tool Predicts Relapse of Pediatric Brain Cancer from Brain MRI Scans
Many pediatric gliomas are treatable with surgery alone, but relapses can be catastrophic. Predicting which patients are at risk for recurrence remains challenging, leading to frequent follow-ups with... Read more
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read moreUltrasound
view channel.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read more
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read moreGeneral/Advanced Imaging
view channel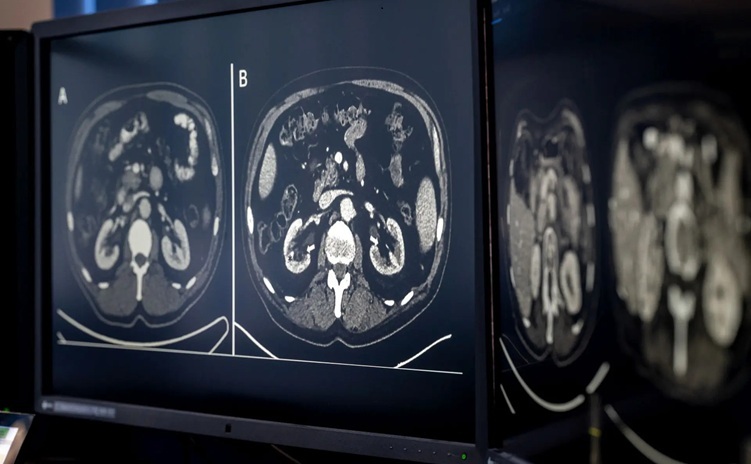
AI-Based CT Scan Analysis Predicts Early-Stage Kidney Damage Due to Cancer Treatments
Radioligand therapy, a form of targeted nuclear medicine, has recently gained attention for its potential in treating specific types of tumors. However, one of the potential side effects of this therapy... Read more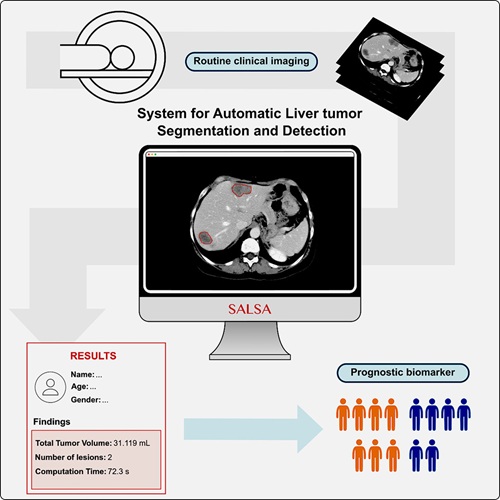
CT-Based Deep Learning-Driven Tool to Enhance Liver Cancer Diagnosis
Medical imaging, such as computed tomography (CT) scans, plays a crucial role in oncology, offering essential data for cancer detection, treatment planning, and monitoring of response to therapies.... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more