Noninvasive Imaging, Earlier Surgery Can Stop Seizures in Tuberous Sclerosis Complex
|
By MedImaging International staff writers Posted on 15 Mar 2010 |
When medication fails to control seizures in children with tuberous sclerosis complex (TSC), a rare genetic disorder that affects multiple organ systems and frequently causes epilepsy, surgery to remove part of the brain is frequently necessary. However, presurgical testing, which involves the implanting of electrodes into a child's head, can lead to longer hospital stays and greater risks from surgery. Now, a study has determined that an alternative, noninvasive approach to presurgical testing, along with earlier consideration for surgery, is associated with the best seizure-free surgical outcome in patients with TSC.
The study was led by researchers from the University of California, Los Angeles' (UCLA; USA) Pediatric Epilepsy Surgery Program. "Surgery to remove the portion of the brain causing the epilepsy is the most successful treatment for children with TSC and intractable epilepsy, but mapping which parts to take out can be challenging in a disease with multiple tubers in the brain and therefore multiple potential seizure-generating regions,” said lead study author Dr. Joyce Wu, an associate professor of pediatric neurology at Mattel Children's Hospital at UCLA. "The standard test of implanting electrodes into the patient's head is uncomfortable, leads to a prolonged hospital stay with increased costs, and potentially increases the risks from surgery. Our study looked at the effectiveness of our noninvasive, diagnostic imaging approach, which appeared to work just as well.”
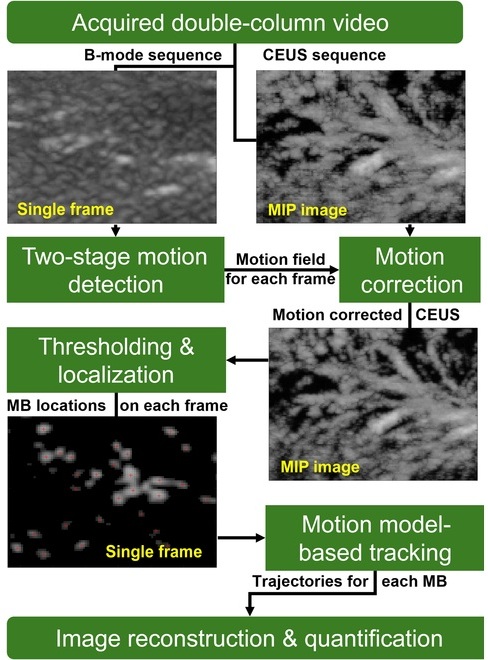
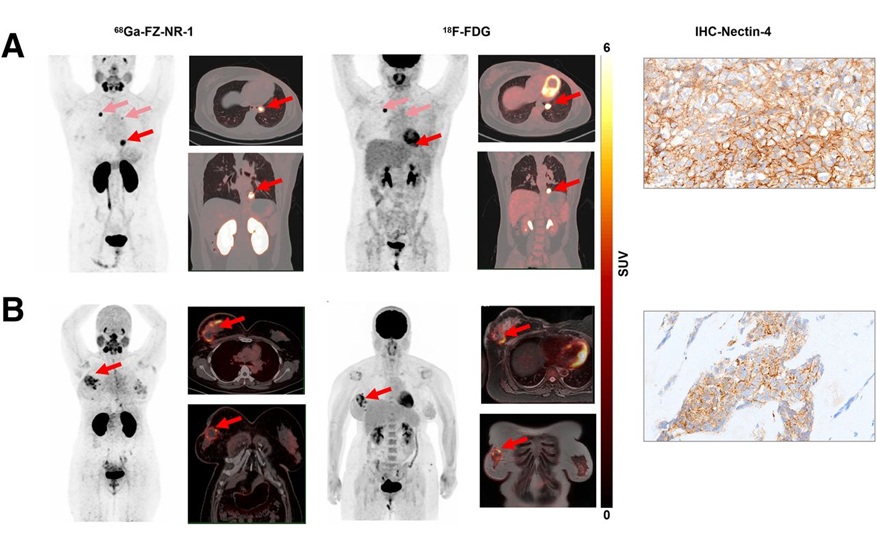
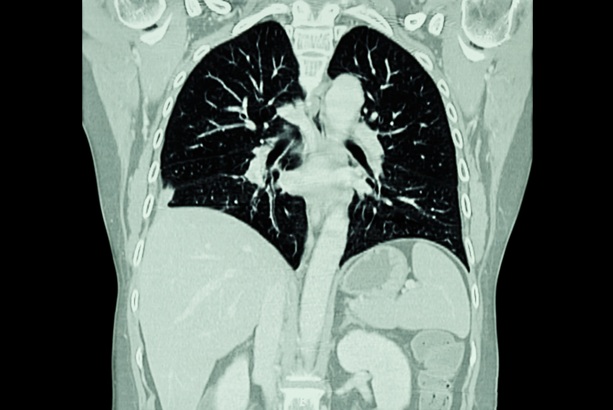
The study is the first to examine UCLA's noninvasive approach, which utilizes a combination of magnetic resonance imaging (MRI), fluorodeoxyglucose positron emission tomography (FDG-PET) and magnetic source imaging (MSI) to identify the area of brain to be removed. The study's findings demonstrated that approximately two-thirds of TSC patients became seizure-free after surgery. The noninvasive results were similar to the traditional surgical testing method of implanting electrodes into the patient's head for several days of monitoring.
Researchers also unexpectedly discovered that shorter seizure duration before surgery was associated with the best chance of children with TSC becoming seizure-free following surgery. Therefore, they reported, it is important to consider surgery early, when medications fail to control seizures. The study findings were published in the February 2, 2010, issue of Neurology, the medical journal of the American Academy of Neurology.
Up to 90% of patients with TSC have epilepsy, with a significant portion suffering from medication-resistant (intractable) epilepsy. For these patients, surgical removal of the tuber and surrounding cerebral cortex may offer seizure freedom.
The study included 28 TSC patients with intractable epilepsy referred to UCLA between 2000 and 2007. In addition to the standard presurgical evaluation, these patients had MSI and FDG-PET/MRI coregistration. None had the invasive intracranial test. Of these patients, 18 (64%) underwent surgical resection, and of those, 12 (67%) were seizure-free postoperatively with an average follow up of 4.1 years.
The study also confirmed that a younger age at surgery and shorter seizure duration were associated with postoperative freedom of seizures. Since epilepsy in children can be severely debilitating, early diagnosis and treatment are vital in helping a child reach full cognitive potential.
Anya, now two-and-a-half years old, underwent the surgery at UCLA when she was 16 months, after suffering up to 30 seizures a day and her medications not working effectively. Dr. Wu and her team suggested that Anya be evaluated for surgery to remove the offending tubers. It has been more than a year since her seven-hour operation, and she is still seizure-free. "TSC is a pretty devastating disease,” said Anya's mother, Anita Smith, who wrote an article about her daughter's condition for a parenting website. "It's important for parents to know that they do not have to put their child through so many invasive tests and that surgery can be more successful if it's done earlier.”
The next stage of research will focus on applying this approach to non-TSC patients, encouraging earlier considerations for surgery, reporting seizure outcomes after longer postoperative follow-ups, and assessing long-term developmental outcomes. "UCLA is one of the few centers with the ability and experience to treat kids with this rare disorder,” said senior author Dr. Gary Mathern, professor of neurosurgery at UCLA. "By developing improved technologies to help these young patients, we hope to make a difference in their lives.”
Related Links:
University of California, Los Angeles
The study was led by researchers from the University of California, Los Angeles' (UCLA; USA) Pediatric Epilepsy Surgery Program. "Surgery to remove the portion of the brain causing the epilepsy is the most successful treatment for children with TSC and intractable epilepsy, but mapping which parts to take out can be challenging in a disease with multiple tubers in the brain and therefore multiple potential seizure-generating regions,” said lead study author Dr. Joyce Wu, an associate professor of pediatric neurology at Mattel Children's Hospital at UCLA. "The standard test of implanting electrodes into the patient's head is uncomfortable, leads to a prolonged hospital stay with increased costs, and potentially increases the risks from surgery. Our study looked at the effectiveness of our noninvasive, diagnostic imaging approach, which appeared to work just as well.”
The study is the first to examine UCLA's noninvasive approach, which utilizes a combination of magnetic resonance imaging (MRI), fluorodeoxyglucose positron emission tomography (FDG-PET) and magnetic source imaging (MSI) to identify the area of brain to be removed. The study's findings demonstrated that approximately two-thirds of TSC patients became seizure-free after surgery. The noninvasive results were similar to the traditional surgical testing method of implanting electrodes into the patient's head for several days of monitoring.
Researchers also unexpectedly discovered that shorter seizure duration before surgery was associated with the best chance of children with TSC becoming seizure-free following surgery. Therefore, they reported, it is important to consider surgery early, when medications fail to control seizures. The study findings were published in the February 2, 2010, issue of Neurology, the medical journal of the American Academy of Neurology.
Up to 90% of patients with TSC have epilepsy, with a significant portion suffering from medication-resistant (intractable) epilepsy. For these patients, surgical removal of the tuber and surrounding cerebral cortex may offer seizure freedom.
The study included 28 TSC patients with intractable epilepsy referred to UCLA between 2000 and 2007. In addition to the standard presurgical evaluation, these patients had MSI and FDG-PET/MRI coregistration. None had the invasive intracranial test. Of these patients, 18 (64%) underwent surgical resection, and of those, 12 (67%) were seizure-free postoperatively with an average follow up of 4.1 years.
The study also confirmed that a younger age at surgery and shorter seizure duration were associated with postoperative freedom of seizures. Since epilepsy in children can be severely debilitating, early diagnosis and treatment are vital in helping a child reach full cognitive potential.
Anya, now two-and-a-half years old, underwent the surgery at UCLA when she was 16 months, after suffering up to 30 seizures a day and her medications not working effectively. Dr. Wu and her team suggested that Anya be evaluated for surgery to remove the offending tubers. It has been more than a year since her seven-hour operation, and she is still seizure-free. "TSC is a pretty devastating disease,” said Anya's mother, Anita Smith, who wrote an article about her daughter's condition for a parenting website. "It's important for parents to know that they do not have to put their child through so many invasive tests and that surgery can be more successful if it's done earlier.”
The next stage of research will focus on applying this approach to non-TSC patients, encouraging earlier considerations for surgery, reporting seizure outcomes after longer postoperative follow-ups, and assessing long-term developmental outcomes. "UCLA is one of the few centers with the ability and experience to treat kids with this rare disorder,” said senior author Dr. Gary Mathern, professor of neurosurgery at UCLA. "By developing improved technologies to help these young patients, we hope to make a difference in their lives.”
Related Links:
University of California, Los Angeles
Latest Nuclear Medicine News
- Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
- Combining Advanced Imaging Technologies Offers Breakthrough in Glioblastoma Treatment
- New Molecular Imaging Agent Accurately Identifies Crucial Cancer Biomarker
- New Scans Light Up Aggressive Tumors for Better Treatment
- AI Stroke Brain Scan Readings Twice as Accurate as Current Method
- AI Analysis of PET/CT Images Predicts Side Effects of Immunotherapy in Lung Cancer
- New Imaging Agent to Drive Step-Change for Brain Cancer Imaging
- Portable PET Scanner to Detect Earliest Stages of Alzheimer’s Disease
Channels
Radiography
view channel
AI Improves Early Detection of Interval Breast Cancers
Interval breast cancers, which occur between routine screenings, are easier to treat when detected earlier. Early detection can reduce the need for aggressive treatments and improve the chances of better outcomes.... Read more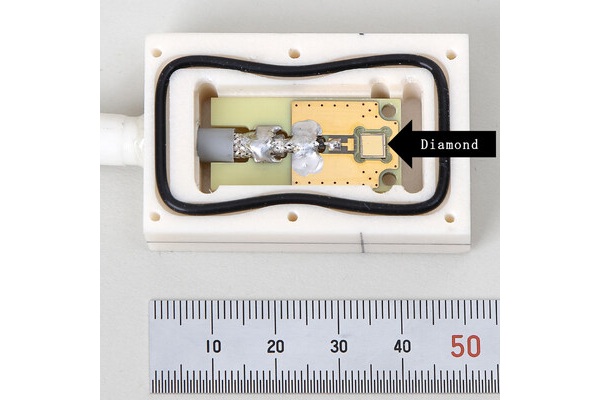
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read moreUltrasound
view channel.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read more
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read moreNuclear Medicine
view channel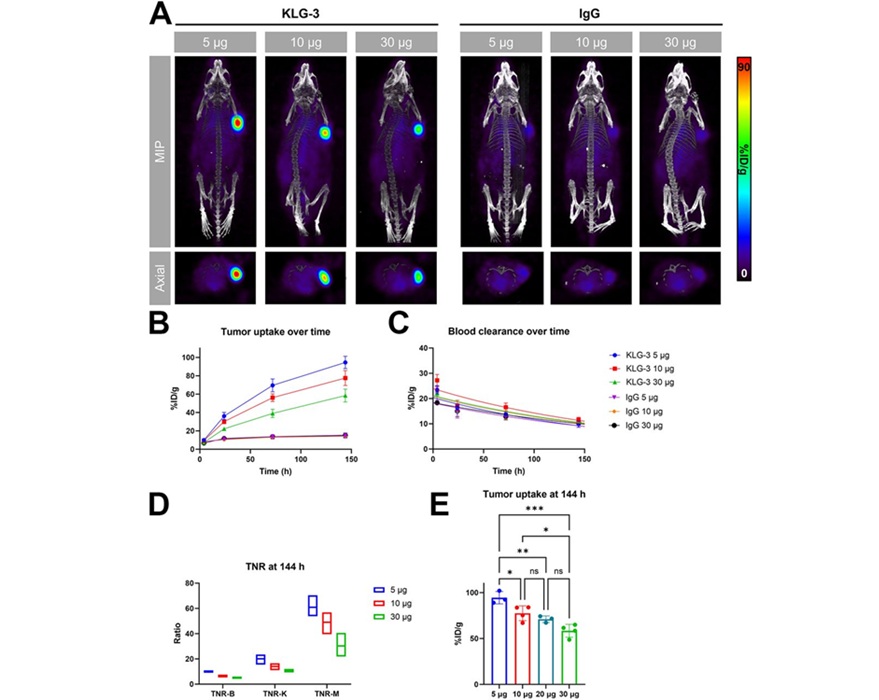
Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
Interleukin-13 receptor α-2 (IL13Rα2) is a cell surface receptor commonly found in solid tumors such as glioblastoma, melanoma, and breast cancer. It is minimally expressed in normal tissues, making it... Read more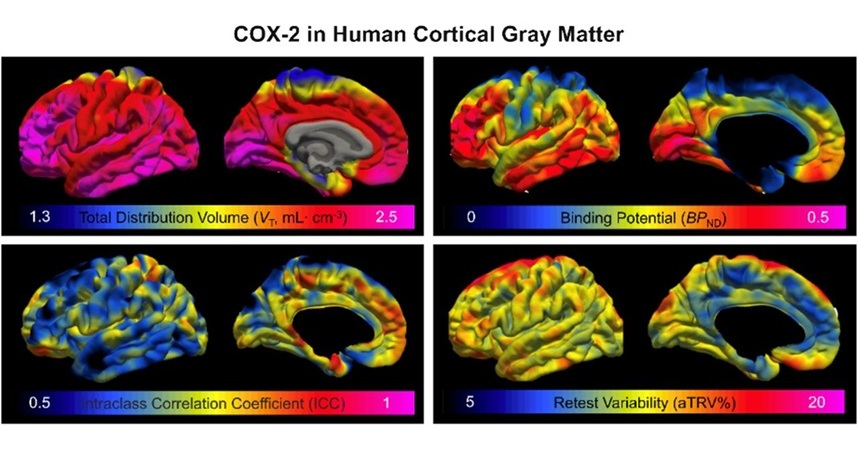
Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
COX-2, an enzyme that plays a key role in brain inflammation, can be significantly upregulated by inflammatory stimuli and neuroexcitation. Researchers suggest that COX-2 density in the brain could serve... Read moreGeneral/Advanced Imaging
view channel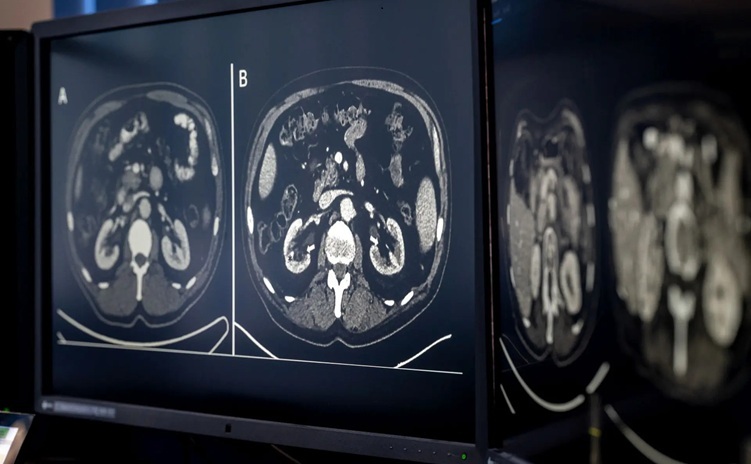
AI-Based CT Scan Analysis Predicts Early-Stage Kidney Damage Due to Cancer Treatments
Radioligand therapy, a form of targeted nuclear medicine, has recently gained attention for its potential in treating specific types of tumors. However, one of the potential side effects of this therapy... Read more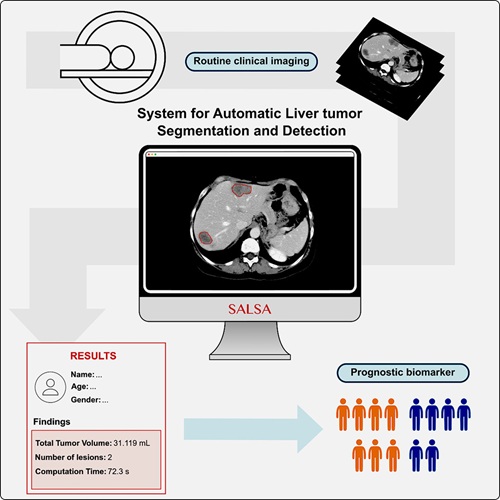
CT-Based Deep Learning-Driven Tool to Enhance Liver Cancer Diagnosis
Medical imaging, such as computed tomography (CT) scans, plays a crucial role in oncology, offering essential data for cancer detection, treatment planning, and monitoring of response to therapies.... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel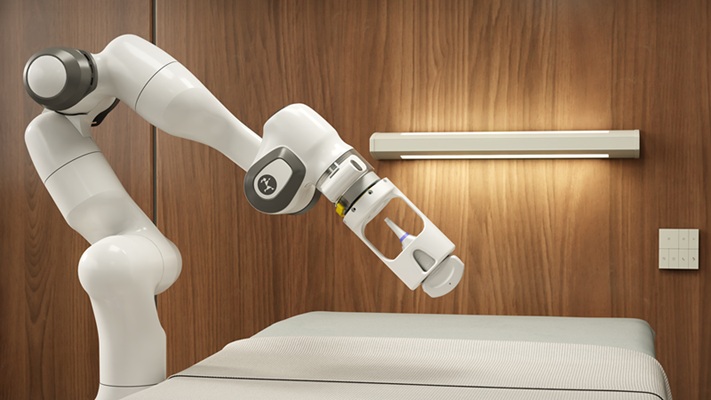
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more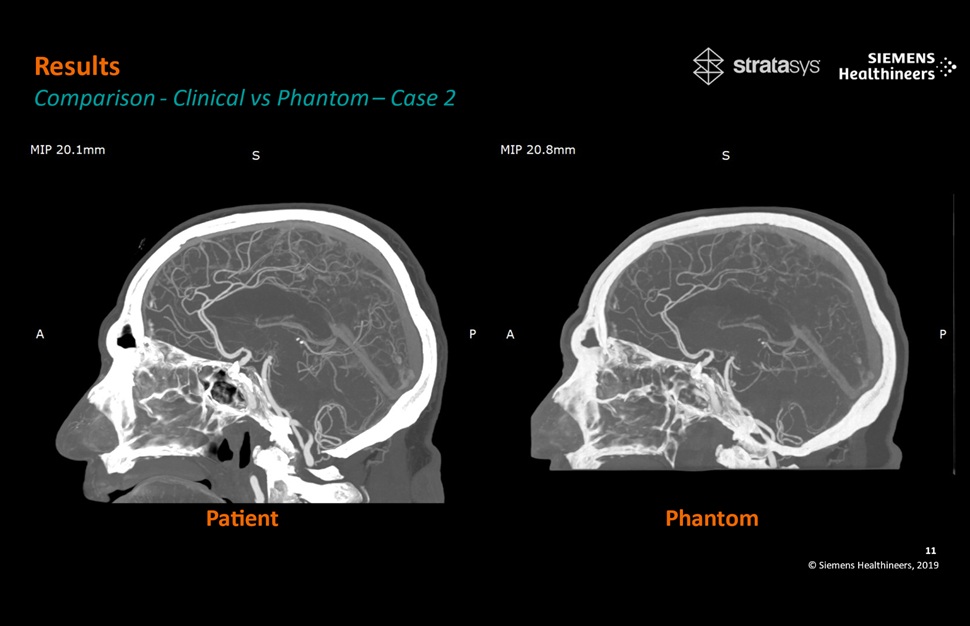
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more