Functional Brain PET Imaging Effectively Forecasts Which Vegetative Patients Can Recover Consciousness
|
By MedImaging International staff writers Posted on 27 Apr 2014 |

Image: A functional brain imaging technique known as positron emission tomography (PET) is a promising tool for determining which severely brain damaged individuals in vegetative states have the potential to recover consciousness (Photo courtesy of sonap / Fotolia).
Positron emission tomography (PET) has the potential for determining which brain damaged individuals in vegetative states have the potential to recover consciousness, according to new research.
The study’s findings were published online April 16, 2014, in the Lancet. It is the first time that researchers have assessed the diagnostic accuracy of functional brain imaging techniques in clinical practice. “Our findings suggest that PET imaging can reveal cognitive processes that aren’t visible through traditional bedside tests, and could substantially complement standard behavioral assessments to identify unresponsive or ‘vegetative’ patients who have the potential for long-term recovery,” stated study leader Prof. Steven Laureys, from the University of Liége (Belgium).
In severely brain-damaged individuals, judging the level of consciousness has proved challenging. Traditionally, bedside clinical examinations have been used to decide whether patients are in a minimally conscious state (MCS), in which there is some evidence of awareness and response to stimuli, or are in a vegetative state (VS) also known as unresponsive wakefulness syndrome, where there is neither, and the chance of recovery is much lower. But up to 40% of patients are misdiagnosed using these scans.
“In patients with substantial cerebral edema, prediction of outcome on the basis of standard clinical examination and structural brain imaging is probably little better than flipping a coin,” wrote Jamie Sleigh from the University of Auckland (New Zealand), and Catherine Warnaby from the University of Oxford (UK), in a linked comment.
The study evaluated whether two new functional brain imaging techniques—PET with the imaging agent fluorodeoxyglucose (FDG) and functional MRI (fMRI) during mental imagery tasks—could differentiate between vegetative and MCS in 126 patients with severe brain injury (81 in a MCS, 41 in a VS, and four with locked-in syndrome—a behaviorally unresponsive but conscious control group) referred to the University Hospital of Liége, from across Europe. The researchers then compared their results with the well-established standardized Coma Recovery Scale-Revised (CSR-R) behavioral test, considered the most confirmed and sensitive technique for discriminating very low awareness.
FDG-PET was better overall than fMRI in differentiating conscious from unconscious patients. Mental imagery fMRI was less sensitive at diagnosis of a MCS than FDG-PET (45% vs. 93%), and had less agreement with behavioral CRS-R scores than FDG-PET (63% vs. 85%). FDG-PET was about 74% accurate in predicting the extent of recovery within the next year, compared with 56% for fMRI.
Significantly, one-third of the 36 patients diagnosed as behaviorally unresponsive on the CSR-R test who were scanned with FDG-PET showed brain activity consistent with the presence of some consciousness. Nine patients in this group consequently recovered a reasonable level of consciousness.
According to Prof. Laureys, “We confirm that a small but substantial proportion of behaviorally unresponsive patients retain brain activity compatible with awareness. Repeated testing with the CRS-R complemented with a cerebral FDG-PET examination provides a simple and reliable diagnostic tool with high sensitivity towards unresponsive but aware patients. fMRI during mental tasks might complement the assessment with information about preserved cognitive capability, but should not be the main or sole diagnostic imaging method.”
The authors noted that the study was conducted in a specialist unit focusing on the diagnostic neuroimaging of disorders of consciousness and therefore deployment might be more challenging in less specialist units.
Commenting on the study Drs. Sleigh and Warnaby added, “From these data, it would be hard to sustain a confident diagnosis of unresponsive wakefulness syndrome solely on behavioral grounds, without PET imaging for confirmation ... [This] work serves as a signpost for future studies. Functional brain imaging is expensive and technically challenging, but it will almost certainly become cheaper and easier. In the future, we will probably look back in amazement at how we were ever able to practice without it.”
Related Links:
University of Liége
The study’s findings were published online April 16, 2014, in the Lancet. It is the first time that researchers have assessed the diagnostic accuracy of functional brain imaging techniques in clinical practice. “Our findings suggest that PET imaging can reveal cognitive processes that aren’t visible through traditional bedside tests, and could substantially complement standard behavioral assessments to identify unresponsive or ‘vegetative’ patients who have the potential for long-term recovery,” stated study leader Prof. Steven Laureys, from the University of Liége (Belgium).
In severely brain-damaged individuals, judging the level of consciousness has proved challenging. Traditionally, bedside clinical examinations have been used to decide whether patients are in a minimally conscious state (MCS), in which there is some evidence of awareness and response to stimuli, or are in a vegetative state (VS) also known as unresponsive wakefulness syndrome, where there is neither, and the chance of recovery is much lower. But up to 40% of patients are misdiagnosed using these scans.
“In patients with substantial cerebral edema, prediction of outcome on the basis of standard clinical examination and structural brain imaging is probably little better than flipping a coin,” wrote Jamie Sleigh from the University of Auckland (New Zealand), and Catherine Warnaby from the University of Oxford (UK), in a linked comment.
The study evaluated whether two new functional brain imaging techniques—PET with the imaging agent fluorodeoxyglucose (FDG) and functional MRI (fMRI) during mental imagery tasks—could differentiate between vegetative and MCS in 126 patients with severe brain injury (81 in a MCS, 41 in a VS, and four with locked-in syndrome—a behaviorally unresponsive but conscious control group) referred to the University Hospital of Liége, from across Europe. The researchers then compared their results with the well-established standardized Coma Recovery Scale-Revised (CSR-R) behavioral test, considered the most confirmed and sensitive technique for discriminating very low awareness.
FDG-PET was better overall than fMRI in differentiating conscious from unconscious patients. Mental imagery fMRI was less sensitive at diagnosis of a MCS than FDG-PET (45% vs. 93%), and had less agreement with behavioral CRS-R scores than FDG-PET (63% vs. 85%). FDG-PET was about 74% accurate in predicting the extent of recovery within the next year, compared with 56% for fMRI.
Significantly, one-third of the 36 patients diagnosed as behaviorally unresponsive on the CSR-R test who were scanned with FDG-PET showed brain activity consistent with the presence of some consciousness. Nine patients in this group consequently recovered a reasonable level of consciousness.
According to Prof. Laureys, “We confirm that a small but substantial proportion of behaviorally unresponsive patients retain brain activity compatible with awareness. Repeated testing with the CRS-R complemented with a cerebral FDG-PET examination provides a simple and reliable diagnostic tool with high sensitivity towards unresponsive but aware patients. fMRI during mental tasks might complement the assessment with information about preserved cognitive capability, but should not be the main or sole diagnostic imaging method.”
The authors noted that the study was conducted in a specialist unit focusing on the diagnostic neuroimaging of disorders of consciousness and therefore deployment might be more challenging in less specialist units.
Commenting on the study Drs. Sleigh and Warnaby added, “From these data, it would be hard to sustain a confident diagnosis of unresponsive wakefulness syndrome solely on behavioral grounds, without PET imaging for confirmation ... [This] work serves as a signpost for future studies. Functional brain imaging is expensive and technically challenging, but it will almost certainly become cheaper and easier. In the future, we will probably look back in amazement at how we were ever able to practice without it.”
Related Links:
University of Liége
Latest Nuclear Medicine News
- Novel Bacteria-Specific PET Imaging Approach Detects Hard-To-Diagnose Lung Infections
- New Imaging Approach Could Reduce Need for Biopsies to Monitor Prostate Cancer
- Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
- Combining Advanced Imaging Technologies Offers Breakthrough in Glioblastoma Treatment
- New Molecular Imaging Agent Accurately Identifies Crucial Cancer Biomarker
- New Scans Light Up Aggressive Tumors for Better Treatment
- AI Stroke Brain Scan Readings Twice as Accurate as Current Method
- AI Analysis of PET/CT Images Predicts Side Effects of Immunotherapy in Lung Cancer
Channels
Radiography
view channel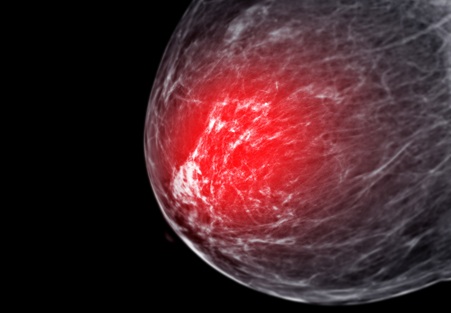
AI Helps Radiologists Spot More Lesions in Mammograms
Breast cancer is a critical health issue, and accurate detection through mammography is essential for effective treatment. However, interpreting mammograms can be challenging for radiologists, particularly... Read more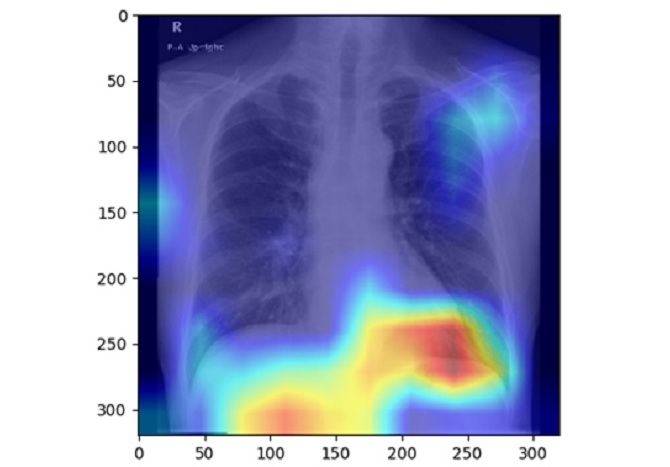
AI Detects Fatty Liver Disease from Chest X-Rays
Fatty liver disease, which results from excess fat accumulation in the liver, is believed to impact approximately one in four individuals globally. If not addressed in time, it can progress to severe conditions... Read moreMRI
view channel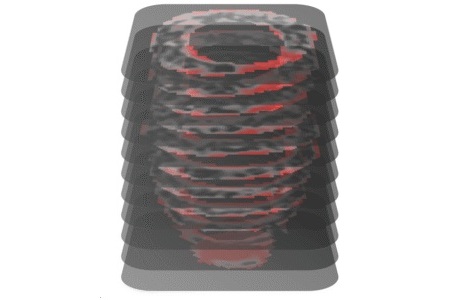
AI Model Outperforms Doctors at Identifying Patients Most At-Risk of Cardiac Arrest
Hypertrophic cardiomyopathy is one of the most common inherited heart conditions and a leading cause of sudden cardiac death in young individuals and athletes. While many patients live normal lives, some... Read more
New MRI Technique Reveals Hidden Heart Issues
Traditional exercise stress tests conducted within an MRI machine require patients to lie flat, a position that artificially improves heart function by increasing stroke volume due to gravity-driven blood... Read moreUltrasound
view channel
Pain-Free Breast Imaging System Performs One Minute Cancer Scan
Breast cancer is one of the leading causes of death for women worldwide, and early detection is key to improving outcomes. Traditional methods like mammograms and ultrasound have their limitations, particularly... Read more
Wireless Chronic Pain Management Device to Reduce Need for Painkillers and Surgery
Chronic pain affects millions of people globally, often leading to long-term disability and dependence on opioid medications, which carry significant risks of side effects and addiction.... Read moreGeneral/Advanced Imaging
view channel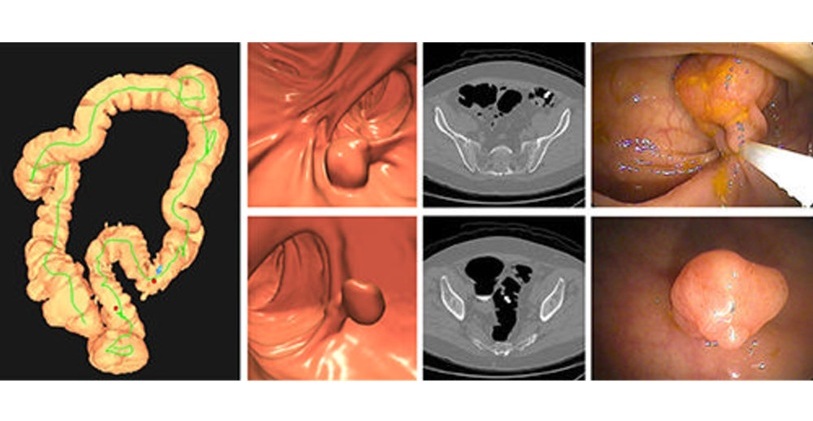
CT Colonography Beats Stool DNA Testing for Colon Cancer Screening
As colorectal cancer remains the second leading cause of cancer-related deaths worldwide, early detection through screening is vital to reduce advanced-stage treatments and associated costs.... Read more
First-Of-Its-Kind Wearable Device Offers Revolutionary Alternative to CT Scans
Currently, patients with conditions such as heart failure, pneumonia, or respiratory distress often require multiple imaging procedures that are intermittent, disruptive, and involve high levels of radiation.... Read more
AI-Based CT Scan Analysis Predicts Early-Stage Kidney Damage Due to Cancer Treatments
Radioligand therapy, a form of targeted nuclear medicine, has recently gained attention for its potential in treating specific types of tumors. However, one of the potential side effects of this therapy... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
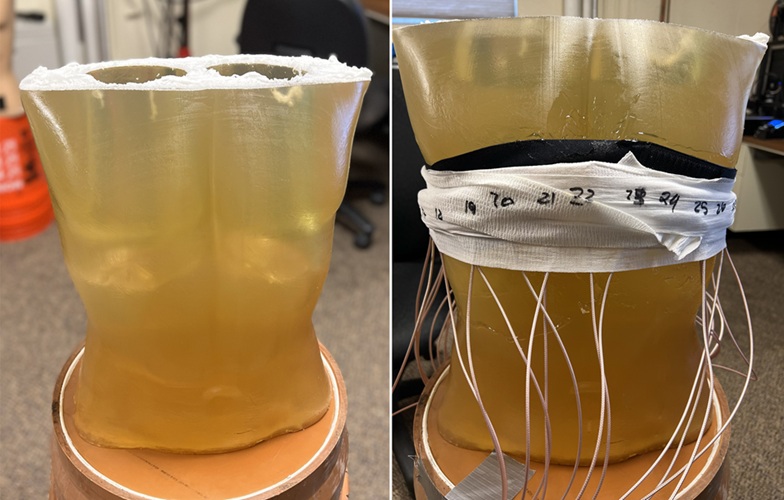
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more