Early Imaging, Diagnosis of Alzheimer’s Leads to Better Outcomes for Patients in Early Stages of the Disease
|
By MedImaging International staff writers Posted on 02 Oct 2013 |
Patients has present with early symptoms of Alzheimer’s disease (AD) who were diagnosed sooner using a brain imaging modality received Alzheimer-specific drugs earlier than those who did not have the brain imaging findings available. These patients also had substantially better clinical outcomes during the following years they were clinically tracked.
The study, called Metabolic Cerebral Imaging in Incipient Dementia, is an ongoing US national clinical trial sponsored by the US Centers for Medicare and Medicaid Services (CMS; Washington DC, USA). These interim data revealed that patients whose physicians gathered data from a brain positron emission tomography (PET) imaging scan performed with the tracer fluorodeoxyglucose (FDG) did better over two years than those whose doctors were randomized to not have access to the scan information.
Study lead investigator Dr. Daniel Silverman, a University of California, Los Angeles (UCLA; USA) professor of molecular and medical pharmacology, said, “During the subsequent two years after their PET scans, these patients had superior executive function, better memory abilities and greater preservation of overall cognitive function, providing the first direct evidence that patients whose early Alzheimer’s disease is revealed by FDG-PET will do better than patients with the same condition, but with their brain metabolism pattern remaining unknown to their doctors and themselves.”
The findings from the study were presented September 26, 2013, at the Medical Biotech Forum, held in Shenzhen (China). US Medicare currently does not reimburse for PET scans for patients showing signs of persistent cognitive decline, but who do not yet have dementia, according to Dr. Silverman. By the time Medicare covers an FDG-PET scan, for which they reimburse roughly USD 1,200 per patient, a lot of impairment, some of it irreversible, has already been done to the brain tissue.
Medicare currently is reexamining reimbursement policies for PET scans obtained in dementia cases, specifically with respect to amyloid imaging. A US healthcare coverage decision is expected October 1, 2013, according to Dr. Silverman. Prior to the findings of the study being presented, there was no thoroughly controlled scientific data available that evaluated the long-term clinical advantages associated with obtaining a PET scan, or any other kind of neuroimaging, in the assessment of cognitively declining patients.
According to the investigators, this multicenter, prospective, randomized and blinded study demonstrates significant clinical benefit, which may also cost less healthcare dollars. “Patients who don’t have Alzheimer’s disease may be prescribed drugs that won’t help them, or even make them worse,” Dr. Silverman said.
An undiagnosed AD patient, furthermore, will not get drugs that the study is showing will help them maintain their cognitive abilities when administered earlier. This may lead to the need for nursing home care six to nine months earlier than for those with the same AD brain pattern, but who are diagnosed and treated sooner as a result of the early availability of the PET scan data. “With nursing home care costing an average of about USD 7,000 a month, there is the potential for CMS and American taxpayers to save several billion dollars per year,” Dr. Silverman said.
These interim findings included 63 patients who underwent FDG-PET and neuropsychologic testing at baseline. The doctors in the arm of the study who were able to view the PET scan immediately treated their patients differently than the physicians in the other arm, who did not get scan results until the end of the two-year study. Approximately 40% of the patients whose clinicians were informed of the presence of the AD brain metabolism pattern were given drugs specifically indicated for dementia within the first six months of the study.
Of the patients whose brain PET scans showed the Alzheimer metabolism patterns randomized to a two-year delay of release of their scan results, none were prescribed Alzheimer drugs in the first six months, and only 12% were prescribed those medications by the end of the first year, according to Dr. Silverman. “[…] This study provides the first direct evidence for improved cognitive outcomes attributable to a neuroimaging test of any kind.”
Related Links:
US Centers for Medicare and Medicaid Services
University of California, Los Angeles
The study, called Metabolic Cerebral Imaging in Incipient Dementia, is an ongoing US national clinical trial sponsored by the US Centers for Medicare and Medicaid Services (CMS; Washington DC, USA). These interim data revealed that patients whose physicians gathered data from a brain positron emission tomography (PET) imaging scan performed with the tracer fluorodeoxyglucose (FDG) did better over two years than those whose doctors were randomized to not have access to the scan information.
Study lead investigator Dr. Daniel Silverman, a University of California, Los Angeles (UCLA; USA) professor of molecular and medical pharmacology, said, “During the subsequent two years after their PET scans, these patients had superior executive function, better memory abilities and greater preservation of overall cognitive function, providing the first direct evidence that patients whose early Alzheimer’s disease is revealed by FDG-PET will do better than patients with the same condition, but with their brain metabolism pattern remaining unknown to their doctors and themselves.”
The findings from the study were presented September 26, 2013, at the Medical Biotech Forum, held in Shenzhen (China). US Medicare currently does not reimburse for PET scans for patients showing signs of persistent cognitive decline, but who do not yet have dementia, according to Dr. Silverman. By the time Medicare covers an FDG-PET scan, for which they reimburse roughly USD 1,200 per patient, a lot of impairment, some of it irreversible, has already been done to the brain tissue.
Medicare currently is reexamining reimbursement policies for PET scans obtained in dementia cases, specifically with respect to amyloid imaging. A US healthcare coverage decision is expected October 1, 2013, according to Dr. Silverman. Prior to the findings of the study being presented, there was no thoroughly controlled scientific data available that evaluated the long-term clinical advantages associated with obtaining a PET scan, or any other kind of neuroimaging, in the assessment of cognitively declining patients.
According to the investigators, this multicenter, prospective, randomized and blinded study demonstrates significant clinical benefit, which may also cost less healthcare dollars. “Patients who don’t have Alzheimer’s disease may be prescribed drugs that won’t help them, or even make them worse,” Dr. Silverman said.
An undiagnosed AD patient, furthermore, will not get drugs that the study is showing will help them maintain their cognitive abilities when administered earlier. This may lead to the need for nursing home care six to nine months earlier than for those with the same AD brain pattern, but who are diagnosed and treated sooner as a result of the early availability of the PET scan data. “With nursing home care costing an average of about USD 7,000 a month, there is the potential for CMS and American taxpayers to save several billion dollars per year,” Dr. Silverman said.
These interim findings included 63 patients who underwent FDG-PET and neuropsychologic testing at baseline. The doctors in the arm of the study who were able to view the PET scan immediately treated their patients differently than the physicians in the other arm, who did not get scan results until the end of the two-year study. Approximately 40% of the patients whose clinicians were informed of the presence of the AD brain metabolism pattern were given drugs specifically indicated for dementia within the first six months of the study.
Of the patients whose brain PET scans showed the Alzheimer metabolism patterns randomized to a two-year delay of release of their scan results, none were prescribed Alzheimer drugs in the first six months, and only 12% were prescribed those medications by the end of the first year, according to Dr. Silverman. “[…] This study provides the first direct evidence for improved cognitive outcomes attributable to a neuroimaging test of any kind.”
Related Links:
US Centers for Medicare and Medicaid Services
University of California, Los Angeles
Latest Nuclear Medicine News
- New SPECT/CT Technique Could Change Imaging Practices and Increase Patient Access
- New Radiotheranostic System Detects and Treats Ovarian Cancer Noninvasively
- AI System Automatically and Reliably Detects Cardiac Amyloidosis Using Scintigraphy Imaging
- Early 30-Minute Dynamic FDG-PET Acquisition Could Halve Lung Scan Times
- New Method for Triggering and Imaging Seizures to Help Guide Epilepsy Surgery
- Radioguided Surgery Accurately Detects and Removes Metastatic Lymph Nodes in Prostate Cancer Patients
- New PET Tracer Detects Inflammatory Arthritis Before Symptoms Appear
- Novel PET Tracer Enhances Lesion Detection in Medullary Thyroid Cancer
- Targeted Therapy Delivers Radiation Directly To Cells in Hard-To-Treat Cancers
- New PET Tracer Noninvasively Identifies Cancer Gene Mutation for More Precise Diagnosis
- Algorithm Predicts Prostate Cancer Recurrence in Patients Treated by Radiation Therapy
- Novel PET Imaging Tracer Noninvasively Identifies Cancer Gene Mutation for More Precise Diagnosis
- Ultrafast Laser Technology to Improve Cancer Treatment
- Low-Dose Radiation Therapy Demonstrates Potential for Treatment of Heart Failure
- New PET Radiotracer Aids Early, Noninvasive Detection of Inflammatory Bowel Disease
- Combining Amino Acid PET and MRI Imaging to Help Treat Aggressive Brain Tumors
Channels
Radiography
view channel
Novel Breast Imaging System Proves As Effective As Mammography
Breast cancer remains the most frequently diagnosed cancer among women. It is projected that one in eight women will be diagnosed with breast cancer during her lifetime, and one in 42 women who turn 50... Read more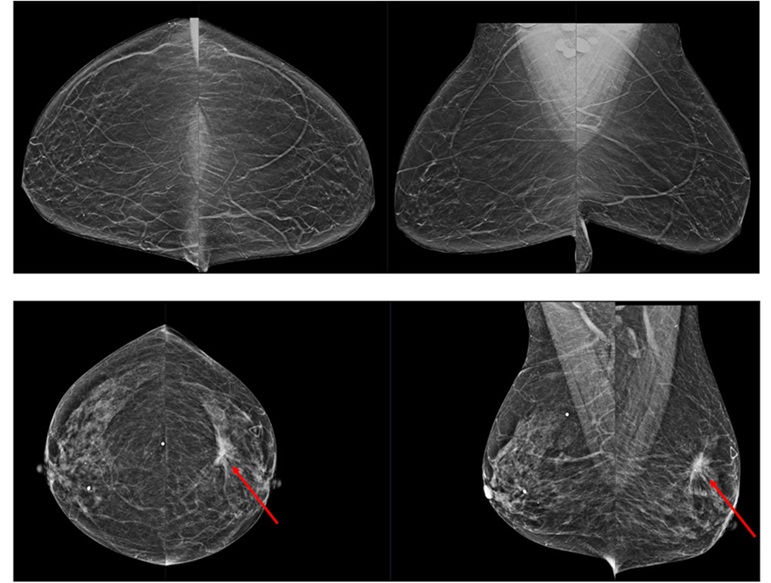
AI Assistance Improves Breast-Cancer Screening by Reducing False Positives
Radiologists typically detect one case of cancer for every 200 mammograms reviewed. However, these evaluations often result in false positives, leading to unnecessary patient recalls for additional testing,... Read moreMRI
view channel
Diamond Dust Could Offer New Contrast Agent Option for Future MRI Scans
Gadolinium, a heavy metal used for over three decades as a contrast agent in medical imaging, enhances the clarity of MRI scans by highlighting affected areas. Despite its utility, gadolinium not only... Read more.jpg)
Combining MRI with PSA Testing Improves Clinical Outcomes for Prostate Cancer Patients
Prostate cancer is a leading health concern globally, consistently being one of the most common types of cancer among men and a major cause of cancer-related deaths. In the United States, it is the most... Read more
PET/MRI Improves Diagnostic Accuracy for Prostate Cancer Patients
The Prostate Imaging Reporting and Data System (PI-RADS) is a five-point scale to assess potential prostate cancer in MR images. PI-RADS category 3 which offers an unclear suggestion of clinically significant... Read more
Next Generation MR-Guided Focused Ultrasound Ushers In Future of Incisionless Neurosurgery
Essential tremor, often called familial, idiopathic, or benign tremor, leads to uncontrollable shaking that significantly affects a person’s life. When traditional medications do not alleviate symptoms,... Read moreUltrasound
view channel.jpg)
Groundbreaking Technology Enables Precise, Automatic Measurement of Peripheral Blood Vessels
The current standard of care of using angiographic information is often inadequate for accurately assessing vessel size in the estimated 20 million people in the U.S. who suffer from peripheral vascular disease.... Read more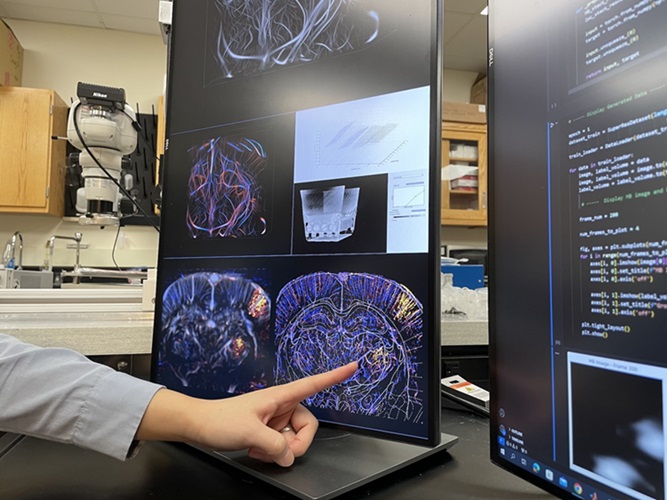
Deep Learning Advances Super-Resolution Ultrasound Imaging
Ultrasound localization microscopy (ULM) is an advanced imaging technique that offers high-resolution visualization of microvascular structures. It employs microbubbles, FDA-approved contrast agents, injected... Read more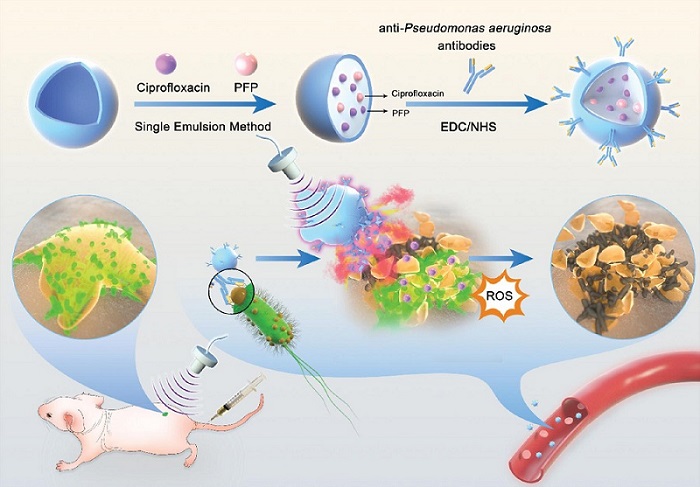
Novel Ultrasound-Launched Targeted Nanoparticle Eliminates Biofilm and Bacterial Infection
Biofilms, formed by bacteria aggregating into dense communities for protection against harsh environmental conditions, are a significant contributor to various infectious diseases. Biofilms frequently... Read moreGeneral/Advanced Imaging
view channel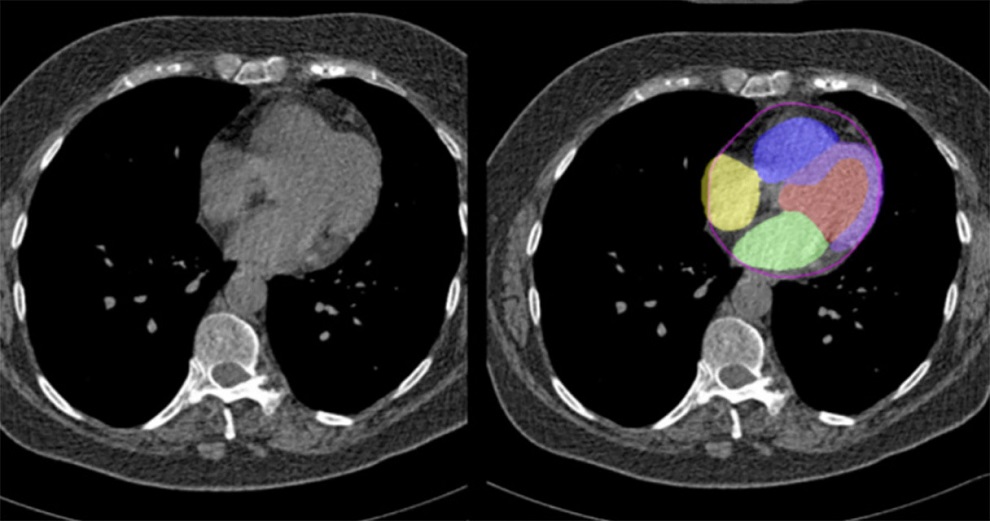
Artificial Intelligence Evaluates Cardiovascular Risk from CT Scans
Chest computed tomography (CT) is a common diagnostic tool, with approximately 15 million scans conducted each year in the United States, though many are underutilized or not fully explored.... Read more
New AI Method Captures Uncertainty in Medical Images
In the field of biomedicine, segmentation is the process of annotating pixels from an important structure in medical images, such as organs or cells. Artificial Intelligence (AI) models are utilized to... Read more.jpg)
CT Coronary Angiography Reduces Need for Invasive Tests to Diagnose Coronary Artery Disease
Coronary artery disease (CAD), one of the leading causes of death worldwide, involves the narrowing of coronary arteries due to atherosclerosis, resulting in insufficient blood flow to the heart muscle.... Read more
Novel Blood Test Could Reduce Need for PET Imaging of Patients with Alzheimer’s
Alzheimer's disease (AD), a condition marked by cognitive decline and the presence of beta-amyloid (Aβ) plaques and neurofibrillary tangles in the brain, poses diagnostic challenges. Amyloid positron emission... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
Bayer and Google Partner on New AI Product for Radiologists
Medical imaging data comprises around 90% of all healthcare data, and it is a highly complex and rich clinical data modality and serves as a vital tool for diagnosing patients. Each year, billions of medical... Read more