New Method for Triggering and Imaging Seizures to Help Guide Epilepsy Surgery
Posted on 13 Mar 2024
Individuals experiencing epilepsy and seizures unmanageable with medication often find brain surgery beneficial. This procedure aims to excise the epileptic tissue while preserving healthy tissue, thus controlling seizures without inducing neurological damage. Accurately identifying the epileptic tissue is crucial for the success of such surgeries, and the acquisition of images during seizures can significantly enhance the precision of surgical planning. Traditionally, ictal SPECT has been the exclusive neuro-imaging technique capable of capturing seizures as they occur within the brain since the 1990s. Yet, the increasing demands on healthcare resources and time have led many epilepsy centers to forgo this informative method. A new approach for inducing and imaging seizures could now enable clinicians to obtain real-time insights for customizing epilepsy surgery more effectively.
In comparison to the previous approach, where physicians from neurology and nuclear medicine waited for hours to days to capture the onset of a seizure, the new method developed by researchers at University Hospital of Bern (Bern, Switzerland), is more convenient, requires fewer resources, and is clinically feasible. In their study involving three adult subjects with left temporal lobe epilepsy, the researchers decided not to wait for spontaneous occurrences and instead imaged planned seizures that were triggered with targeted electrical stimulation to the brain. The research team employed stereotactic electroencephalography (sEEG) leads placed in specific brain regions to induce seizures characteristic of each patient. A radiotracer, 99mTc-HMPAO, was administered within 12 seconds of the seizure's start, with SPECT imaging following within 40 minutes.
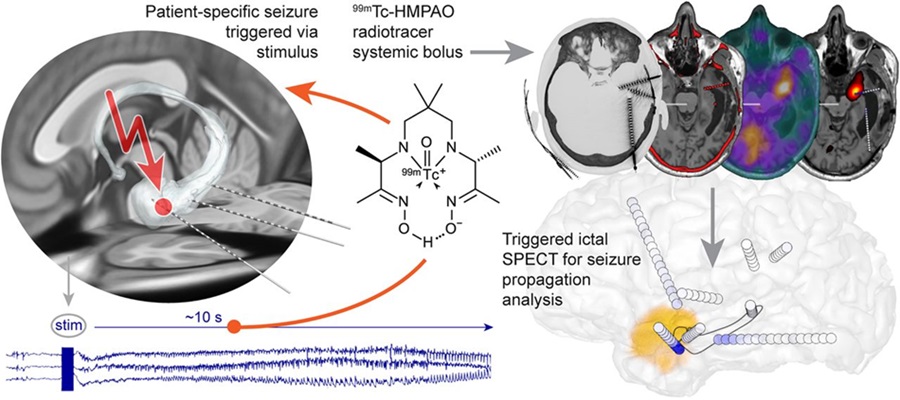
The method successfully triggered seizures in all the participants, replicating each patient's typical seizure presentation and electrographic pattern observed through sEEG, without causing any adverse effects. The seizures induced were specific for each patient, with early seizure spread being uniquely imaged. In the first two cases, ictal SPECT provided additional insights beyond those offered by sEEG, highlighting the early involvement of brain regions lacking electrode coverage. In the third case, both sEEG and ictal SPECT provided overlapping information.
“The finding of this study is of practical nature, as it greatly facilitates the acquisition of the ictal SPECT,” said Thomas Pyka, MD, Privatdozent in the Department of Nuclear Medicine at the University Hospital of Bern. “This may help obtain images of greater quality and could contribute to the refinement of resection planning, improving seizure and cognitive outcomes in epilepsy surgery.”
Related Links:
University Hospital of Bern














