RT Offers Hope for High-Risk Arrhythmia Patients
|
By MedImaging International staff writers Posted on 09 Oct 2019 |
Image: According to a new study, RT can offer hope the VT patients who have exhausted other options (Photo courtesy of SPL).
A single, high dose of radiation therapy (RT) can dramatically reduce episodes of ventricular tachycardia (VT) for more than two years, according to a new study.
Developed at the Washington University (WUSTL; St. Louis, MO, USA) School of Medicine, the noninvasive, outpatient procedure for treating VT is called EP-guided noninvasive cardiac radioablation (ENCORE). The novel therapy fuses electrocardiogram (ECG) and imaging data to pinpoint the scar tissue in the patient's heart responsible for the arrhythmias, and then targets it with a single dose of stereotactic body radiation therapy (SBRT). ENCORE requires no general anesthesia, and allows patients to go home immediately after treatment.
In a phase I/II prospective trial, 19 patients who had life-threatening VT were treated with a single fraction (25 Gy) of SBRT. ENCORE led to a 94% reduction in VT episodes in the first six months after SBRT, with longer-term follow-up data showing that the effect persisted in 78% of patients for more than two years; overall survival was 52% after the second year. Of the nine patients who died, six suffered from cardiac deaths (heart failure and VT recurrence) and three from non-cardiac deaths (accident, amiodarone toxicity, and pancreatic cancer). The study was presented at the 61st annual meeting of the American Society for Radiation Oncology (ASTRO), held during September 2019 in Chicago (IL, USA).
“Patients come to us as a last line of defense. They have few or no other options. Often, the primary reason we are treating them is because they were too sick to have more catheter ablation,” said lead author and study presenter Clifford Robinson, MD, an associate professor of radiation oncology and cardiology at WUSTL. “Given the relative novelty of this treatment approach, we are following our patients closely, conducting trials to gather more data and being careful not to make assumptions at this point.”
“An additional benefit to treatment was a reduction in the medications patients were taking, which resulted in fewer medication-related side effects and a higher quality of life,” concluded Dr. Robinson. “These patients were on heavy doses of medications, with side effects such as liver damage, lung damage, nausea, and thyroid problems. After they were treated, we could dramatically reduce their medications. We saw reduced VT, reduced medication and improved quality of life, at least in the intermediate term.”
In VT, the electrical signals in the heart’s lower chambers misfire, crippling the relaxation and refilling process and producing rapid arrhythmias. First line treatment for VT includes pharmaceuticals and an implantable cardioverter defibrillator (ICD). Patients with recurrent VT often also undergo catheter ablation, which requires general anesthesia, takes up to nine hours to perform, holds a 5% mortality risk, and has a 50% chance that it won't stop VT arrhythmias from recurring. If catheter ablation does not control the VT, patients are left with few options beyond a heart transplant.
Related Links:
Washington University
Developed at the Washington University (WUSTL; St. Louis, MO, USA) School of Medicine, the noninvasive, outpatient procedure for treating VT is called EP-guided noninvasive cardiac radioablation (ENCORE). The novel therapy fuses electrocardiogram (ECG) and imaging data to pinpoint the scar tissue in the patient's heart responsible for the arrhythmias, and then targets it with a single dose of stereotactic body radiation therapy (SBRT). ENCORE requires no general anesthesia, and allows patients to go home immediately after treatment.
In a phase I/II prospective trial, 19 patients who had life-threatening VT were treated with a single fraction (25 Gy) of SBRT. ENCORE led to a 94% reduction in VT episodes in the first six months after SBRT, with longer-term follow-up data showing that the effect persisted in 78% of patients for more than two years; overall survival was 52% after the second year. Of the nine patients who died, six suffered from cardiac deaths (heart failure and VT recurrence) and three from non-cardiac deaths (accident, amiodarone toxicity, and pancreatic cancer). The study was presented at the 61st annual meeting of the American Society for Radiation Oncology (ASTRO), held during September 2019 in Chicago (IL, USA).
“Patients come to us as a last line of defense. They have few or no other options. Often, the primary reason we are treating them is because they were too sick to have more catheter ablation,” said lead author and study presenter Clifford Robinson, MD, an associate professor of radiation oncology and cardiology at WUSTL. “Given the relative novelty of this treatment approach, we are following our patients closely, conducting trials to gather more data and being careful not to make assumptions at this point.”
“An additional benefit to treatment was a reduction in the medications patients were taking, which resulted in fewer medication-related side effects and a higher quality of life,” concluded Dr. Robinson. “These patients were on heavy doses of medications, with side effects such as liver damage, lung damage, nausea, and thyroid problems. After they were treated, we could dramatically reduce their medications. We saw reduced VT, reduced medication and improved quality of life, at least in the intermediate term.”
In VT, the electrical signals in the heart’s lower chambers misfire, crippling the relaxation and refilling process and producing rapid arrhythmias. First line treatment for VT includes pharmaceuticals and an implantable cardioverter defibrillator (ICD). Patients with recurrent VT often also undergo catheter ablation, which requires general anesthesia, takes up to nine hours to perform, holds a 5% mortality risk, and has a 50% chance that it won't stop VT arrhythmias from recurring. If catheter ablation does not control the VT, patients are left with few options beyond a heart transplant.
Related Links:
Washington University
Latest Nuclear Medicine News
- PET Imaging of Inflammation Predicts Recovery and Guides Therapy After Heart Attack
- Radiotheranostic Approach Detects, Kills and Reprograms Aggressive Cancers
- New Imaging Solution Improves Survival for Patients with Recurring Prostate Cancer
- PET Tracer Enables Same-Day Imaging of Triple-Negative Breast and Urothelial Cancers
- New Camera Sees Inside Human Body for Enhanced Scanning and Diagnosis
- Novel Bacteria-Specific PET Imaging Approach Detects Hard-To-Diagnose Lung Infections
- New Imaging Approach Could Reduce Need for Biopsies to Monitor Prostate Cancer
- Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
Channels
Radiography
view channel
AI Detects Early Signs of Aging from Chest X-Rays
Chronological age does not always reflect how fast the body is truly aging, and current biological age tests often rely on DNA-based markers that may miss early organ-level decline. Detecting subtle, age-related... Read more
X-Ray Breakthrough Captures Three Image-Contrast Types in Single Shot
Detecting early-stage cancer or subtle changes deep inside tissues has long challenged conventional X-ray systems, which rely only on how structures absorb radiation. This limitation keeps many microstructural... Read moreMRI
view channel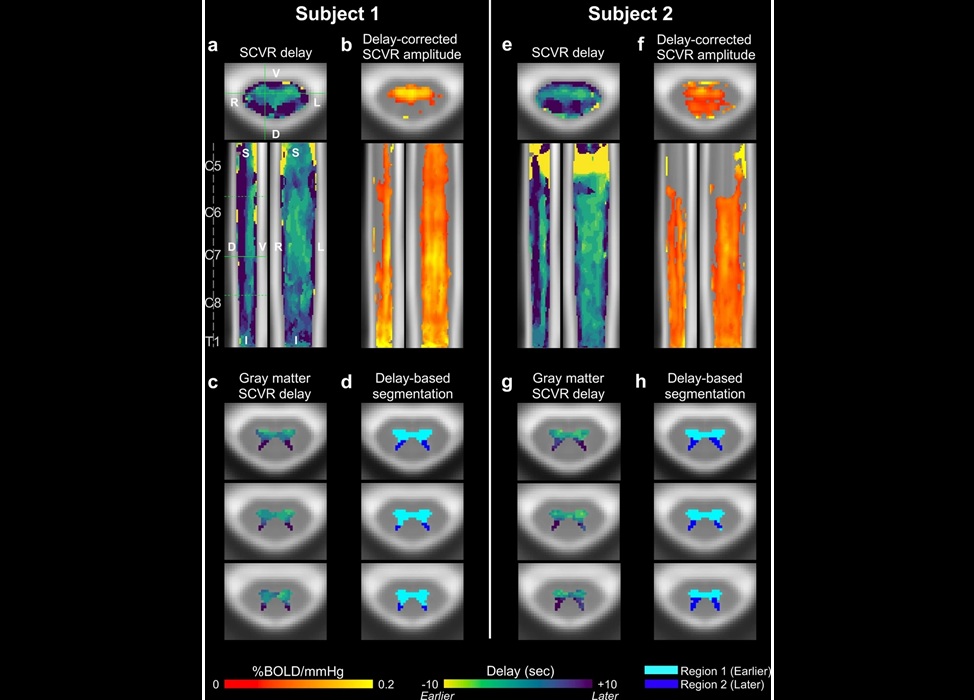
Novel Imaging Approach to Improve Treatment for Spinal Cord Injuries
Vascular dysfunction in the spinal cord contributes to multiple neurological conditions, including traumatic injuries and degenerative cervical myelopathy, where reduced blood flow can lead to progressive... Read more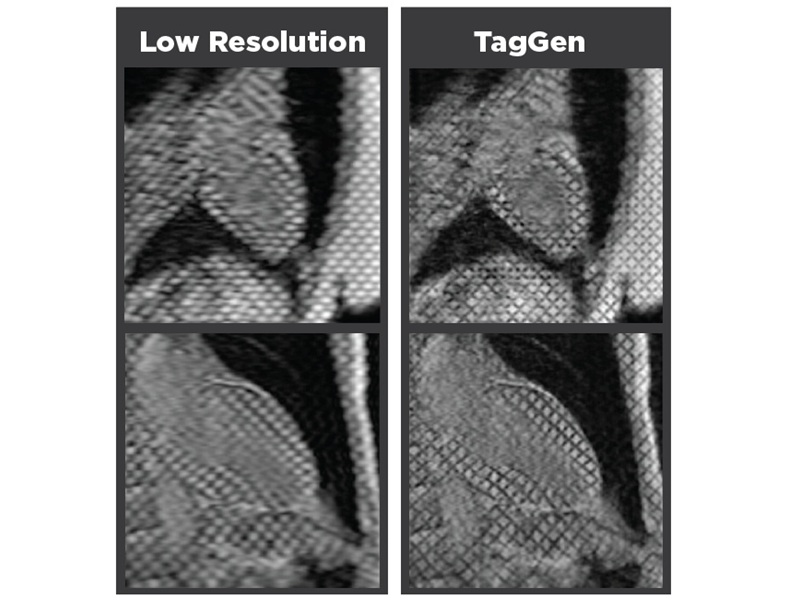
AI-Assisted Model Enhances MRI Heart Scans
A cardiac MRI can reveal critical information about the heart’s function and any abnormalities, but traditional scans take 30 to 90 minutes and often suffer from poor image quality due to patient movement.... Read more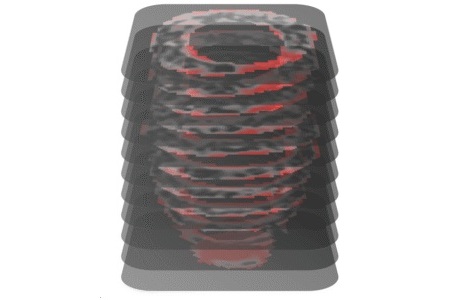
AI Model Outperforms Doctors at Identifying Patients Most At-Risk of Cardiac Arrest
Hypertrophic cardiomyopathy is one of the most common inherited heart conditions and a leading cause of sudden cardiac death in young individuals and athletes. While many patients live normal lives, some... Read moreUltrasound
view channel
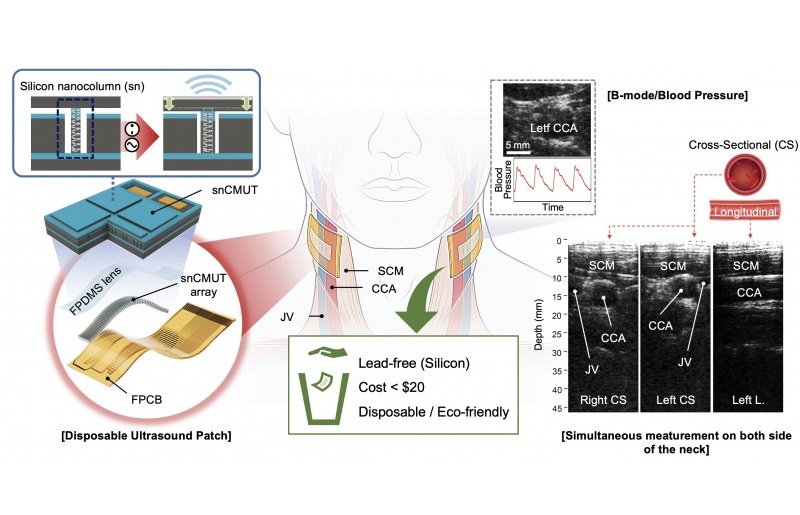
Wearable Ultrasound Imaging System to Enable Real-Time Disease Monitoring
Chronic conditions such as hypertension and heart failure require close monitoring, yet today’s ultrasound imaging is largely confined to hospitals and short, episodic scans. This reactive model limits... Read more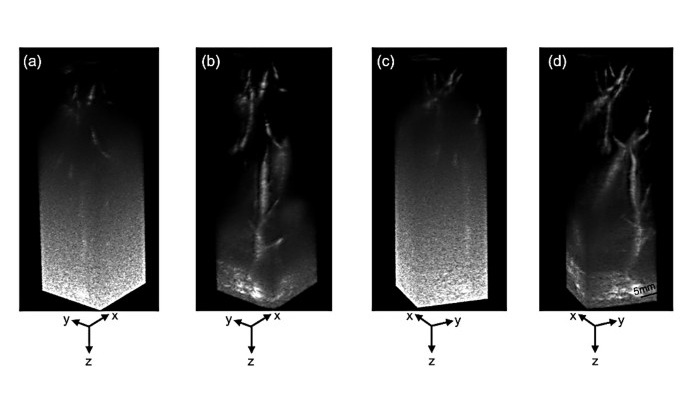
Ultrasound Technique Visualizes Deep Blood Vessels in 3D Without Contrast Agents
Producing clear 3D images of deep blood vessels has long been difficult without relying on contrast agents, CT scans, or MRI. Standard ultrasound typically provides only 2D cross-sections, limiting clinicians’... Read moreGeneral/Advanced Imaging
view channel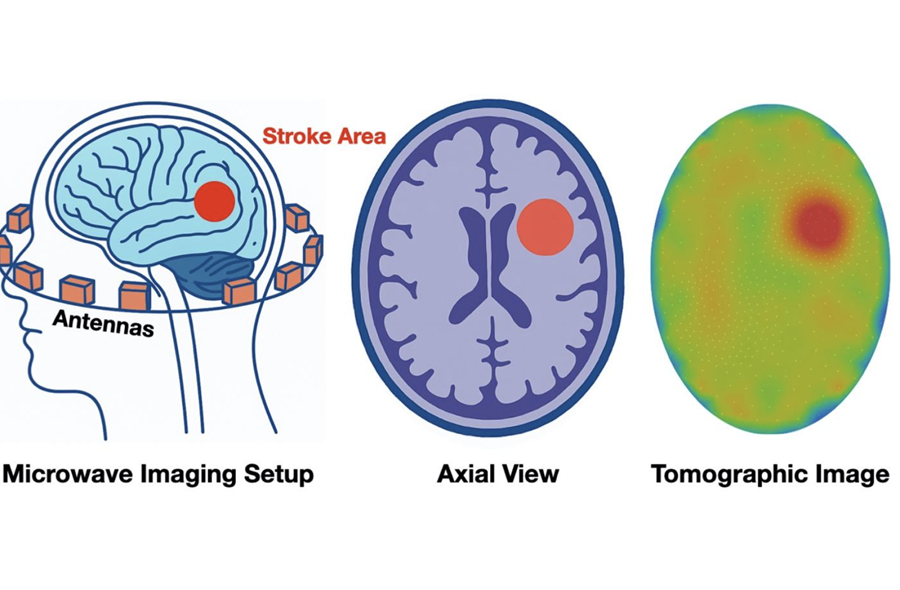
New Algorithm Dramatically Speeds Up Stroke Detection Scans
When patients arrive at emergency rooms with stroke symptoms, clinicians must rapidly determine whether the cause is a blood clot or a brain bleed, as treatment decisions depend on this distinction.... Read more
3D Scanning Approach Enables Ultra-Precise Brain Surgery
Precise navigation is critical in neurosurgery, yet even small alignment errors can affect outcomes when operating deep within the brain. A new 3D surface-scanning approach now provides a radiation-free... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more