Artificial Intelligence Accurately Predicts Radiation Treatment Side Effects
|
By MedImaging International staff writers Posted on 01 Oct 2019 |

Image: New research has shown that a computer model can predict side effects associated with radiation therapy (Photo courtesy of Technology Networks).
Researchers from the University of Texas MD Anderson Cancer Center (Houston, Texas, USA) have demonstrated that a sophisticated computer model can accurately predict two of the most challenging side effects associated with radiation therapy for head and neck cancer. This precision oncology approach has the potential to better identify patients who might benefit from early interventions that could help prevent significant weight loss after treatment or reduce the need for feeding tube placement.
The team of researchers developed models to analyze large sets of data merged from three sources: electronic health records (Epic), an internal web-based charting tool (Brocade) and the record/verify system (Mosaiq). The data included more than 700 clinical and treatment variables for patients with head and neck cancer (75% male/25% female, with a median age of 62 years) who received more than 2,000 courses of radiation therapy (median dose 60 Gy) across five practice sites at MD Anderson from 2016 to 2018.
The researchers used the models to predict three endpoints: significant weight loss, feeding tube placement and unplanned hospitalizations. Results from the best-performing model were then validated against 225 subsequent consecutive radiation therapy treatments. Models with a performance rate that met a pre-specified threshold of area under the curve (AUC) of 0.70 or higher were considered clinically valid (an AUC score of 1.0 would mean the model’s predictions were 100% accurate, while a score of 0.0 would mean the predictions were never accurate). The models predicted the likelihood of significant weight loss (AUC = 0.751) and need for feeding tube placement (AUC = 0.755) with a high degree of accuracy.
“Being able to identify which patients are at greatest risk would allow radiation oncologists to take steps to prevent or mitigate these possible side effects,” said Jay Reddy, MD, PhD, an assistant professor of radiation oncology at The University of Texas MD Anderson Cancer Center and lead author on the study. “If the patient has an intermediate risk, and they might get through treatment without needing a feeding tube, we could take precautions such as setting them up with a nutritionist and providing them with nutritional supplements. If we know their risk for feeding tube placement is extremely high – a better than 50% chance they would need one – we could place it ahead of time so they wouldn’t have to be admitted to the hospital after treatment. We’d know to keep a closer eye on that patient.”
The machine learning approach cannot isolate the single-most predictive factor or combination of factors that lead to negative side effects, but can provide patients and their clinicians with a better understanding of what to expect during the course of treatment. In addition to predicting the likelihood of side effects, machine learning models could potentially predict which treatment plans would be most effective for different types of patients and allow for more personalized approaches to radiation oncology.
“Machine learning can make doctors more efficient and treatment safer by reducing the risk of error,” added Dr. Reddy. “It has the potential for influencing all aspects of radiation oncology today – anything where a computer can look at data and recognize a pattern.”
Related Links:
University of Texas MD Anderson Cancer Center
The team of researchers developed models to analyze large sets of data merged from three sources: electronic health records (Epic), an internal web-based charting tool (Brocade) and the record/verify system (Mosaiq). The data included more than 700 clinical and treatment variables for patients with head and neck cancer (75% male/25% female, with a median age of 62 years) who received more than 2,000 courses of radiation therapy (median dose 60 Gy) across five practice sites at MD Anderson from 2016 to 2018.
The researchers used the models to predict three endpoints: significant weight loss, feeding tube placement and unplanned hospitalizations. Results from the best-performing model were then validated against 225 subsequent consecutive radiation therapy treatments. Models with a performance rate that met a pre-specified threshold of area under the curve (AUC) of 0.70 or higher were considered clinically valid (an AUC score of 1.0 would mean the model’s predictions were 100% accurate, while a score of 0.0 would mean the predictions were never accurate). The models predicted the likelihood of significant weight loss (AUC = 0.751) and need for feeding tube placement (AUC = 0.755) with a high degree of accuracy.
“Being able to identify which patients are at greatest risk would allow radiation oncologists to take steps to prevent or mitigate these possible side effects,” said Jay Reddy, MD, PhD, an assistant professor of radiation oncology at The University of Texas MD Anderson Cancer Center and lead author on the study. “If the patient has an intermediate risk, and they might get through treatment without needing a feeding tube, we could take precautions such as setting them up with a nutritionist and providing them with nutritional supplements. If we know their risk for feeding tube placement is extremely high – a better than 50% chance they would need one – we could place it ahead of time so they wouldn’t have to be admitted to the hospital after treatment. We’d know to keep a closer eye on that patient.”
The machine learning approach cannot isolate the single-most predictive factor or combination of factors that lead to negative side effects, but can provide patients and their clinicians with a better understanding of what to expect during the course of treatment. In addition to predicting the likelihood of side effects, machine learning models could potentially predict which treatment plans would be most effective for different types of patients and allow for more personalized approaches to radiation oncology.
“Machine learning can make doctors more efficient and treatment safer by reducing the risk of error,” added Dr. Reddy. “It has the potential for influencing all aspects of radiation oncology today – anything where a computer can look at data and recognize a pattern.”
Related Links:
University of Texas MD Anderson Cancer Center
Latest Industry News News
- Nuclear Medicine Set for Continued Growth Driven by Demand for Precision Diagnostics
- GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
- Patient-Specific 3D-Printed Phantoms Transform CT Imaging
- Siemens and Sectra Collaborate on Enhancing Radiology Workflows
- Bracco Diagnostics and ColoWatch Partner to Expand Availability CRC Screening Tests Using Virtual Colonoscopy
- Mindray Partners with TeleRay to Streamline Ultrasound Delivery
- Philips and Medtronic Partner on Stroke Care
- Siemens and Medtronic Enter into Global Partnership for Advancing Spine Care Imaging Technologies
- RSNA 2024 Technical Exhibits to Showcase Latest Advances in Radiology
- Bracco Collaborates with Arrayus on Microbubble-Assisted Focused Ultrasound Therapy for Pancreatic Cancer
- Innovative Collaboration to Enhance Ischemic Stroke Detection and Elevate Standards in Diagnostic Imaging
- RSNA 2024 Registration Opens
- Microsoft collaborates with Leading Academic Medical Systems to Advance AI in Medical Imaging
- GE HealthCare Acquires Intelligent Ultrasound Group’s Clinical Artificial Intelligence Business
- Bayer and Rad AI Collaborate on Expanding Use of Cutting Edge AI Radiology Operational Solutions
- Polish Med-Tech Company BrainScan to Expand Extensively into Foreign Markets
Channels
Radiography
view channel
Routine Mammograms Could Predict Future Cardiovascular Disease in Women
Mammograms are widely used to screen for breast cancer, but they may also contain overlooked clues about cardiovascular health. Calcium deposits in the arteries of the breast signal stiffening blood vessels,... Read more
AI Detects Early Signs of Aging from Chest X-Rays
Chronological age does not always reflect how fast the body is truly aging, and current biological age tests often rely on DNA-based markers that may miss early organ-level decline. Detecting subtle, age-related... Read moreMRI
view channel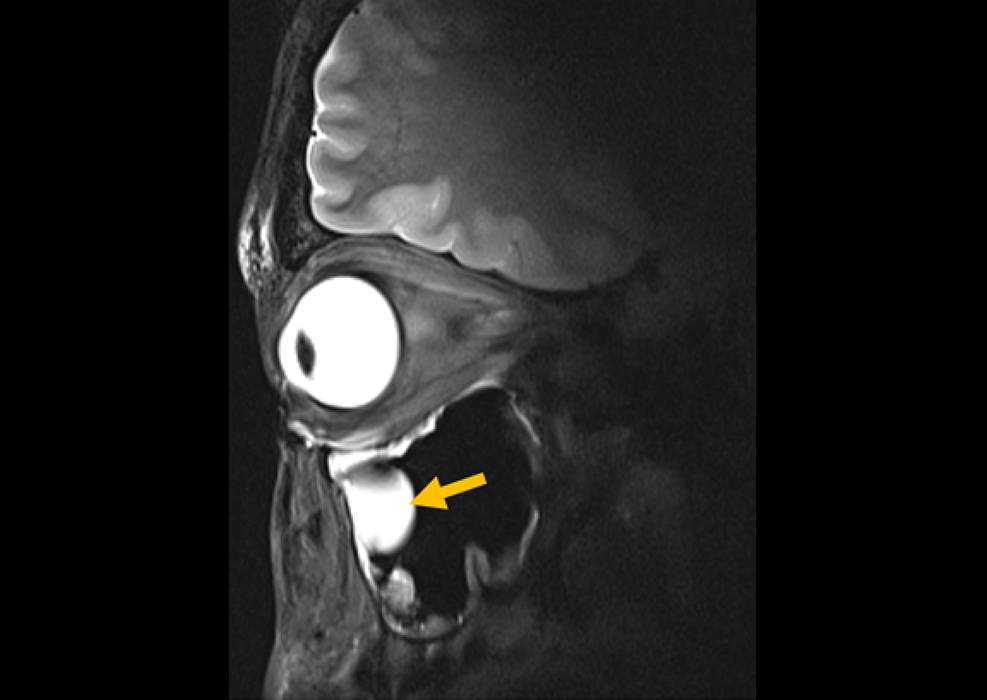
New Material Boosts MRI Image Quality
Magnetic resonance imaging (MRI) is a cornerstone of modern diagnostics, yet certain deep or anatomically complex tissues, including delicate structures of the eye and orbit, remain difficult to visualize clearly.... Read more
AI Model Reads and Diagnoses Brain MRI in Seconds
Brain MRI scans are critical for diagnosing strokes, hemorrhages, and other neurological disorders, but interpreting them can take hours or even days due to growing demand and limited specialist availability.... Read moreMRI Scan Breakthrough to Help Avoid Risky Invasive Tests for Heart Patients
Heart failure patients often require right heart catheterization to assess how severely their heart is struggling to pump blood, a procedure that involves inserting a tube into the heart to measure blood... Read more
MRI Scans Reveal Signature Patterns of Brain Activity to Predict Recovery from TBI
Recovery after traumatic brain injury (TBI) varies widely, with some patients regaining full function while others are left with lasting disabilities. Prognosis is especially difficult to assess in patients... Read moreUltrasound
view channel
Reusable Gel Pad Made from Tamarind Seed Could Transform Ultrasound Examinations
Ultrasound imaging depends on a conductive gel to eliminate air between the probe and the skin so sound waves can pass clearly into the body. While the imaging technology is fast, safe, and noninvasive,... Read more
AI Model Accurately Detects Placenta Accreta in Pregnancy Before Delivery
Placenta accreta spectrum (PAS) is a life-threatening pregnancy complication in which the placenta abnormally attaches to the uterine wall. The condition is a leading cause of maternal mortality and morbidity... Read moreNuclear Medicine
view channel
Radiopharmaceutical Molecule Marker to Improve Choice of Bladder Cancer Therapies
Targeted cancer therapies only work when tumor cells express the specific molecular structures they are designed to attack. In urothelial carcinoma, a common form of bladder cancer, the cell surface protein... Read more
Cancer “Flashlight” Shows Who Can Benefit from Targeted Treatments
Targeted cancer therapies can be highly effective, but only when a patient’s tumor expresses the specific protein the treatment is designed to attack. Determining this usually requires biopsies or advanced... Read moreGeneral/Advanced Imaging
view channel
AI Tool Predicts Side Effects from Lung Cancer Treatment
Radiation therapy is a central treatment for lung cancer, but even carefully targeted radiation can affect surrounding healthy tissue. Patients may develop side effects such as lung inflammation, coughing,... Read more
AI Tool Offers Prognosis for Patients with Head and Neck Cancer
Oropharyngeal cancer is a form of head and neck cancer that can spread through lymph nodes, significantly affecting survival and treatment decisions. Current therapies often involve combinations of surgery,... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more