Mathematical Model Improves Radiation Therapy
|
By MedImaging International staff writers Posted on 19 Sep 2019 |
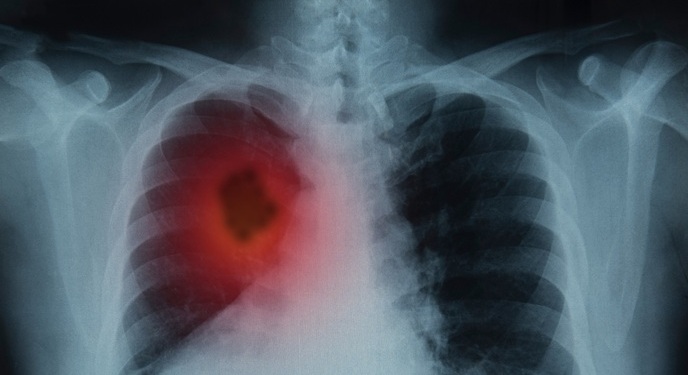
A new mathematical model spatially optimizes external beam radiation therapy (XRT) in order to significantly increase the number of brain tumor cells killed during treatment.
Developed at the University of Waterloo (UW; Canada) and the Massachusetts Institute of Technology (MIT, Cambridge, MA, USA), the new model optimizes one-step and two-step radiation profiles during the first and second XRT fractions, while setting a cap on the total dose a patient could receive throughout treatment. Tumor anatomy was then sectioned into multiple portions, with the area most densely populated with cells being one portion and the remainder of cells the other.
In some instances, they prescribed the dosage of radiation given to each portion, and in other cases, they allowed the model to determine the best ratio. The results suggested that spatial optimization requires imaging the tumor twice, determining the dose and treatment schedule, and optimizing the first radiation fraction using the model. Using the growth model deduced from the initial two images, oncologists can then use the derived cell density profile prior to each instance of XRT as input to optimize the shape of the radiation beam. The study was published on June 28, 2019, in PLOS One.
“Typically, cells in a tumor are packed at a higher density in the middle and less as you go further out, but that fact is not fully taken into account in current radiation treatment,” said lead author PhD candidate Cameron Meaney, MSc, of the Waterloo Department of Applied Mathematics. “What our model has shown is that perhaps what's best is if we take the total radiation dose that we're allowed to give a patient and administer it over a small area at high strength where the cells are most dense, instead of spreading it over a big area with semi-weak strength.”
Glioblastomas are the most aggressive, and unfortunately most common, form of primary brain tumor. They are characterized by rapid growth and invasiveness, yielding survival times that seldom exceed a year. As a result, treatments for glioblastomas are swift and aggressive, usually involving a combination of surgical intervention, chemotherapy, and XRT, with postoperative chemotherapy and XRT a crucial part of effective treatments.
Related Links:
University of Waterloo
Massachusetts Institute of Technology
Developed at the University of Waterloo (UW; Canada) and the Massachusetts Institute of Technology (MIT, Cambridge, MA, USA), the new model optimizes one-step and two-step radiation profiles during the first and second XRT fractions, while setting a cap on the total dose a patient could receive throughout treatment. Tumor anatomy was then sectioned into multiple portions, with the area most densely populated with cells being one portion and the remainder of cells the other.
In some instances, they prescribed the dosage of radiation given to each portion, and in other cases, they allowed the model to determine the best ratio. The results suggested that spatial optimization requires imaging the tumor twice, determining the dose and treatment schedule, and optimizing the first radiation fraction using the model. Using the growth model deduced from the initial two images, oncologists can then use the derived cell density profile prior to each instance of XRT as input to optimize the shape of the radiation beam. The study was published on June 28, 2019, in PLOS One.
“Typically, cells in a tumor are packed at a higher density in the middle and less as you go further out, but that fact is not fully taken into account in current radiation treatment,” said lead author PhD candidate Cameron Meaney, MSc, of the Waterloo Department of Applied Mathematics. “What our model has shown is that perhaps what's best is if we take the total radiation dose that we're allowed to give a patient and administer it over a small area at high strength where the cells are most dense, instead of spreading it over a big area with semi-weak strength.”
Glioblastomas are the most aggressive, and unfortunately most common, form of primary brain tumor. They are characterized by rapid growth and invasiveness, yielding survival times that seldom exceed a year. As a result, treatments for glioblastomas are swift and aggressive, usually involving a combination of surgical intervention, chemotherapy, and XRT, with postoperative chemotherapy and XRT a crucial part of effective treatments.
Related Links:
University of Waterloo
Massachusetts Institute of Technology
Latest General/Advanced Imaging News
- AI-Powered Imaging System Improves Lung Cancer Diagnosis
- AI Model Significantly Enhances Low-Dose CT Capabilities
- Ultra-Low Dose CT Aids Pneumonia Diagnosis in Immunocompromised Patients
- AI Reduces CT Lung Cancer Screening Workload by Almost 80%
- Cutting-Edge Technology Combines Light and Sound for Real-Time Stroke Monitoring
- AI System Detects Subtle Changes in Series of Medical Images Over Time
- New CT Scan Technique to Improve Prognosis and Treatments for Head and Neck Cancers
- World’s First Mobile Whole-Body CT Scanner to Provide Diagnostics at POC
- Comprehensive CT Scans Could Identify Atherosclerosis Among Lung Cancer Patients
- AI Improves Detection of Colorectal Cancer on Routine Abdominopelvic CT Scans
- Super-Resolution Technology Enhances Clinical Bone Imaging to Predict Osteoporotic Fracture Risk
- AI-Powered Abdomen Map Enables Early Cancer Detection
- Deep Learning Model Detects Lung Tumors on CT
- AI Predicts Cardiovascular Risk from CT Scans
- Deep Learning Based Algorithms Improve Tumor Detection in PET/CT Scans
- New Technology Provides Coronary Artery Calcification Scoring on Ungated Chest CT Scans
Channels
Radiography
view channel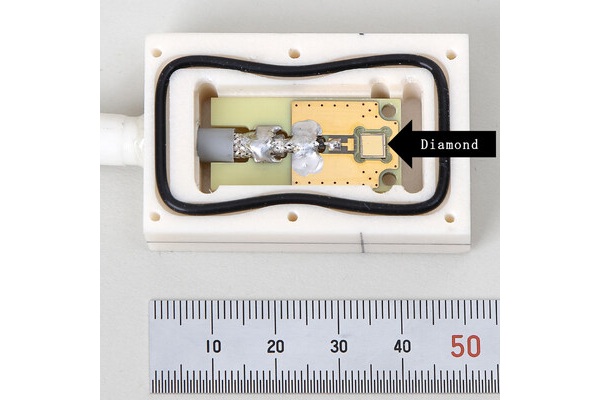
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read more
AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure where small metal tubes called stents are inserted into partially blocked coronary arteries... Read moreMRI
view channel
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read more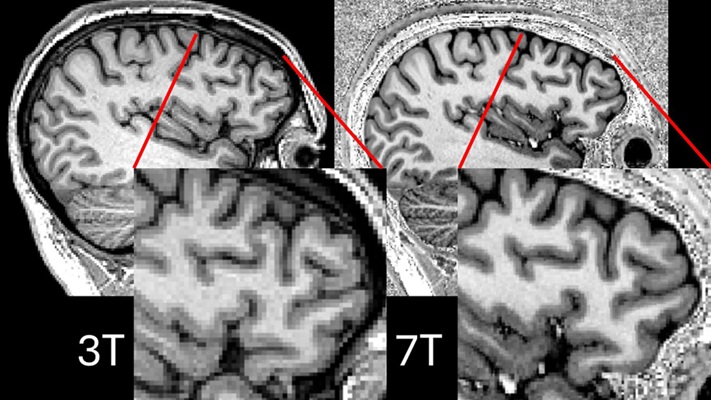
Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
Approximately 360,000 individuals in the UK suffer from focal epilepsy, a condition in which seizures spread from one part of the brain. Around a third of these patients experience persistent seizures... Read more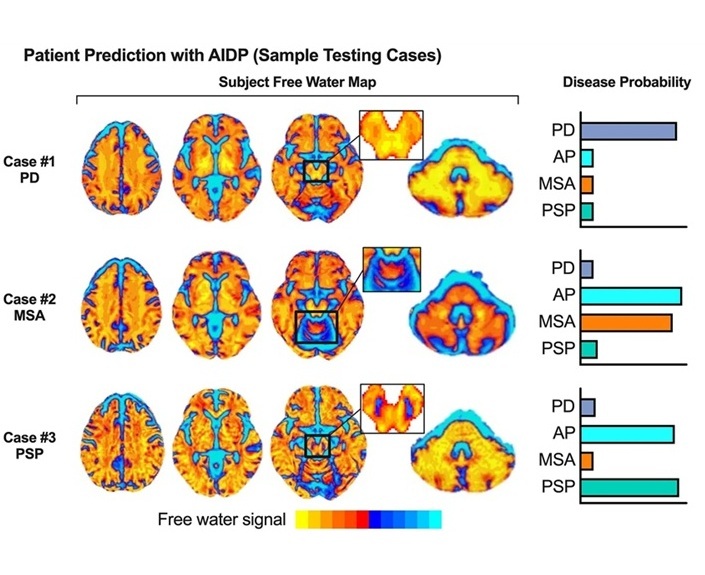
AI-Powered MRI Technology Improves Parkinson’s Diagnoses
Current research shows that the accuracy of diagnosing Parkinson’s disease typically ranges from 55% to 78% within the first five years of assessment. This is partly due to the similarities shared by Parkinson’s... Read more
Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
Artificial intelligence (AI) technologies are transforming the way medical images are analyzed, offering unprecedented capabilities in quantitatively extracting features that go beyond traditional visual... Read moreUltrasound
view channel.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read more
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read moreNuclear Medicine
view channel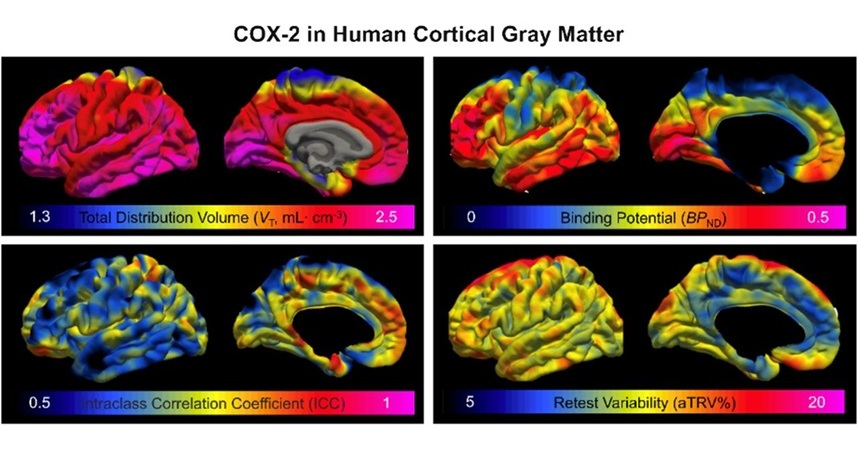
Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
COX-2, an enzyme that plays a key role in brain inflammation, can be significantly upregulated by inflammatory stimuli and neuroexcitation. Researchers suggest that COX-2 density in the brain could serve... Read more
Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC), which represents 15-20% of all breast cancer cases, is one of the most aggressive subtypes, with a five-year survival rate of about 40%. Due to its significant heterogeneity... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more






 Guided Devices.jpg)