Radioactive Iodine Treatment Increases Risk of Cancer Death
|
By MedImaging International staff writers Posted on 16 Jul 2019 |
Patients with hyperthyroidism treated with I-131 radioactive iodine (RAI) are at an increased risk of death due to solid cancer, according to a new study.
Researchers at the U.S. National Cancer Institute (NCI; Rockville, MD, USA), Vanderbilt University Medical Center (VUMC, Nashville, TN, USA), and other institutions undertook a 24-year extension review of a study that followed US and UK patients who were diagnosed and treated for hyperthyroidism, beginning in 1946. A total of 18,805 patients (78% women), who were treated with RAI and who had no prior history of cancer at the time of first treatment were included in the analysis. The excess relative risks (ERRs) per 100-mGy dose to the organ or tissue were calculated.
The mean total administered activity of the RAI was 375 megabecquerel (MBq) for patients with Graves disease, and 653 MBq for patients with toxic nodular goiter. Mean organ or tissue dose estimates ranged from 20-99 mGy (for colon or rectum, ovary, uterus, prostate, bladder, and brain/central nervous system), to 100-400 mGy (for pancreas, kidney, liver, stomach, female breast, lung, oral mucosa, and marrow), to 1.6 Gy (esophagus), and to 130 Gy (thyroid gland).
The researchers identified positive associations for all solid cancer mortality, including female breast cancer (RR 1.12), and all other solid cancers combined (RR 1.05). In patients with Graves disease, the 100-mGy dose to the stomach and breast corresponded to a mean administered activity of 243 and 266 MBq, respectively. The researchers estimated a lifetime excess of 19-32 solid cancer deaths for every 1,000 patients with hyperthyroidism that received typical doses to the stomach (150-250 mGy). The study was published on July 1, 2019, in JAMA Internal Medicine.
“RAI has been used extensively to treat hyperthyroidism since the 1940s. Although widely considered a safe and effective therapy, RAI has been associated with elevated risks of total and site-specific cancer death among patients with hypothyroidism,” concluded lead author Cari Kitahara, PhD, of the NCI, and colleagues. “Greater organ-absorbed doses appeared to be modestly positively associated with risk of death from solid cancer, including breast cancer. Additional studies are needed of the risks and advantages of all major treatment options available to patients with hyperthyroidism.”
In the United States, the prevalence of hyperthyroidism is 1.2% (0.5% overt and 0.7% subclinical), and most cases are due to Graves disease, an autoimmune disease that affects the thyroid, an endocrine gland located in the neck that produces two hormones secreted into the bloodstream, thyroxine (T4) and triiodothyronine (T3); T4 is converted to T3 in cells and tissues. The hormones regulate metabolism. Thyroid disorders include hypothyroidism, hyperthyroidism, nodules, cancer, Graves disease, and post-partum thyroiditis.
Related Links:
U.S. National Cancer Institute
Vanderbilt University Medical Center
Researchers at the U.S. National Cancer Institute (NCI; Rockville, MD, USA), Vanderbilt University Medical Center (VUMC, Nashville, TN, USA), and other institutions undertook a 24-year extension review of a study that followed US and UK patients who were diagnosed and treated for hyperthyroidism, beginning in 1946. A total of 18,805 patients (78% women), who were treated with RAI and who had no prior history of cancer at the time of first treatment were included in the analysis. The excess relative risks (ERRs) per 100-mGy dose to the organ or tissue were calculated.
The mean total administered activity of the RAI was 375 megabecquerel (MBq) for patients with Graves disease, and 653 MBq for patients with toxic nodular goiter. Mean organ or tissue dose estimates ranged from 20-99 mGy (for colon or rectum, ovary, uterus, prostate, bladder, and brain/central nervous system), to 100-400 mGy (for pancreas, kidney, liver, stomach, female breast, lung, oral mucosa, and marrow), to 1.6 Gy (esophagus), and to 130 Gy (thyroid gland).
The researchers identified positive associations for all solid cancer mortality, including female breast cancer (RR 1.12), and all other solid cancers combined (RR 1.05). In patients with Graves disease, the 100-mGy dose to the stomach and breast corresponded to a mean administered activity of 243 and 266 MBq, respectively. The researchers estimated a lifetime excess of 19-32 solid cancer deaths for every 1,000 patients with hyperthyroidism that received typical doses to the stomach (150-250 mGy). The study was published on July 1, 2019, in JAMA Internal Medicine.
“RAI has been used extensively to treat hyperthyroidism since the 1940s. Although widely considered a safe and effective therapy, RAI has been associated with elevated risks of total and site-specific cancer death among patients with hypothyroidism,” concluded lead author Cari Kitahara, PhD, of the NCI, and colleagues. “Greater organ-absorbed doses appeared to be modestly positively associated with risk of death from solid cancer, including breast cancer. Additional studies are needed of the risks and advantages of all major treatment options available to patients with hyperthyroidism.”
In the United States, the prevalence of hyperthyroidism is 1.2% (0.5% overt and 0.7% subclinical), and most cases are due to Graves disease, an autoimmune disease that affects the thyroid, an endocrine gland located in the neck that produces two hormones secreted into the bloodstream, thyroxine (T4) and triiodothyronine (T3); T4 is converted to T3 in cells and tissues. The hormones regulate metabolism. Thyroid disorders include hypothyroidism, hyperthyroidism, nodules, cancer, Graves disease, and post-partum thyroiditis.
Related Links:
U.S. National Cancer Institute
Vanderbilt University Medical Center
Latest Nuclear Medicine News
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
- Combining Advanced Imaging Technologies Offers Breakthrough in Glioblastoma Treatment
- New Molecular Imaging Agent Accurately Identifies Crucial Cancer Biomarker
- New Scans Light Up Aggressive Tumors for Better Treatment
- AI Stroke Brain Scan Readings Twice as Accurate as Current Method
- AI Analysis of PET/CT Images Predicts Side Effects of Immunotherapy in Lung Cancer
- New Imaging Agent to Drive Step-Change for Brain Cancer Imaging
- Portable PET Scanner to Detect Earliest Stages of Alzheimer’s Disease
- New Immuno-PET Imaging Technique Identifies Glioblastoma Patients Who Would Benefit from Immunotherapy
Channels
Radiography
view channel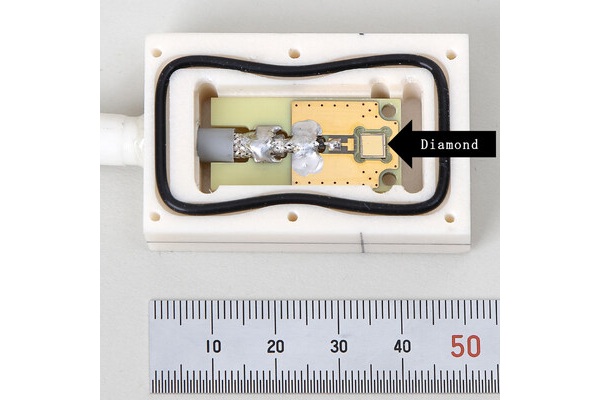
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read more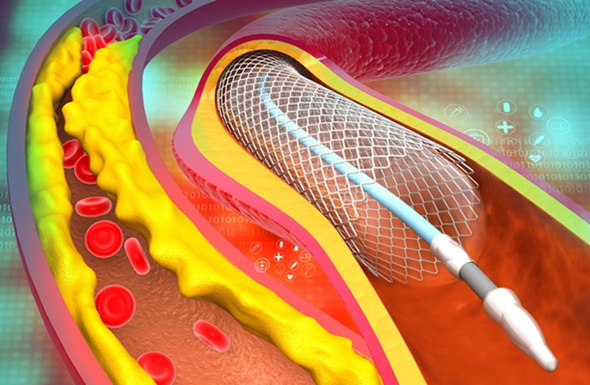
AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure where small metal tubes called stents are inserted into partially blocked coronary arteries... Read moreMRI
view channel
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read more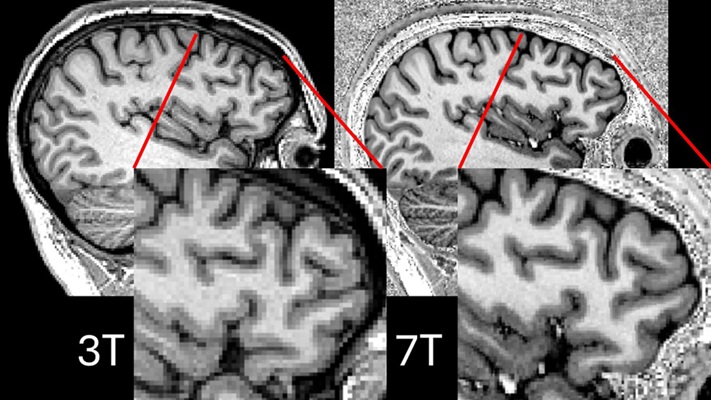
Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
Approximately 360,000 individuals in the UK suffer from focal epilepsy, a condition in which seizures spread from one part of the brain. Around a third of these patients experience persistent seizures... Read more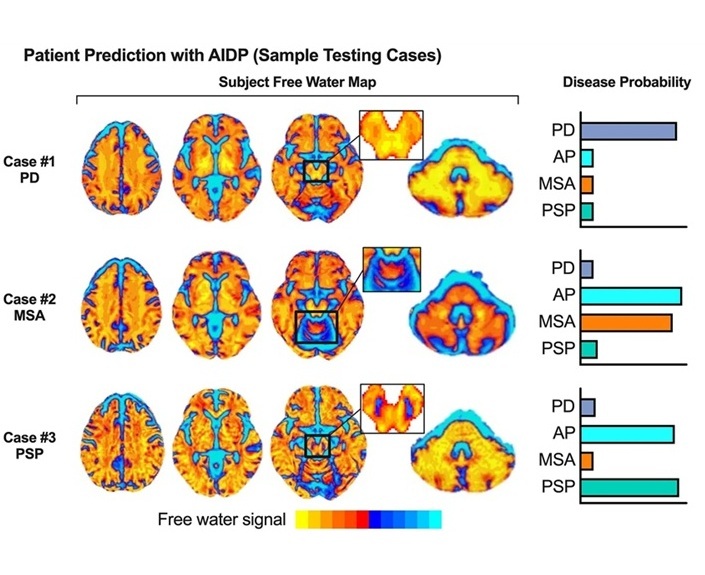
AI-Powered MRI Technology Improves Parkinson’s Diagnoses
Current research shows that the accuracy of diagnosing Parkinson’s disease typically ranges from 55% to 78% within the first five years of assessment. This is partly due to the similarities shared by Parkinson’s... Read more
Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
Artificial intelligence (AI) technologies are transforming the way medical images are analyzed, offering unprecedented capabilities in quantitatively extracting features that go beyond traditional visual... Read moreUltrasound
view channel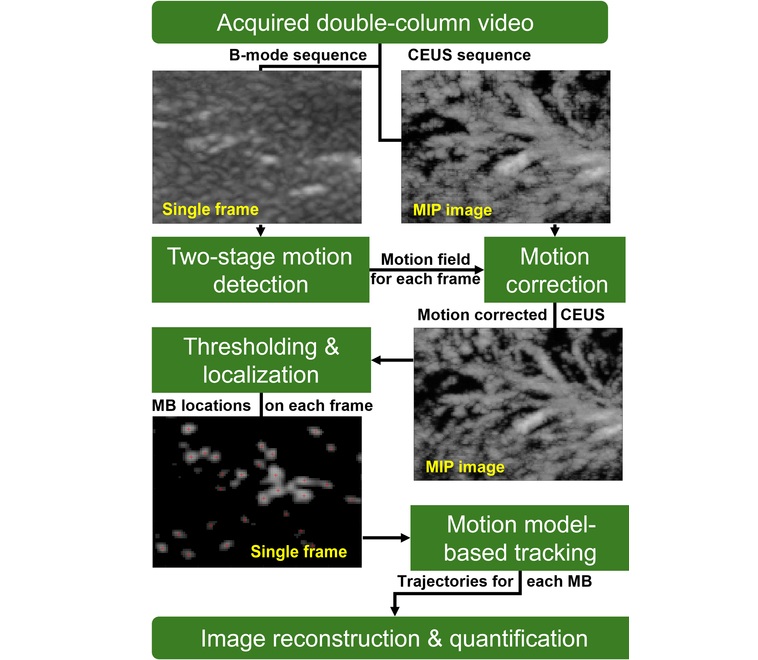
Novel Imaging Method Enables Early Diagnosis and Treatment Monitoring of Type 2 Diabetes
Type 2 diabetes is recognized as an autoimmune inflammatory disease, where chronic inflammation leads to alterations in pancreatic islet microvasculature, a key factor in β-cell dysfunction.... Read more
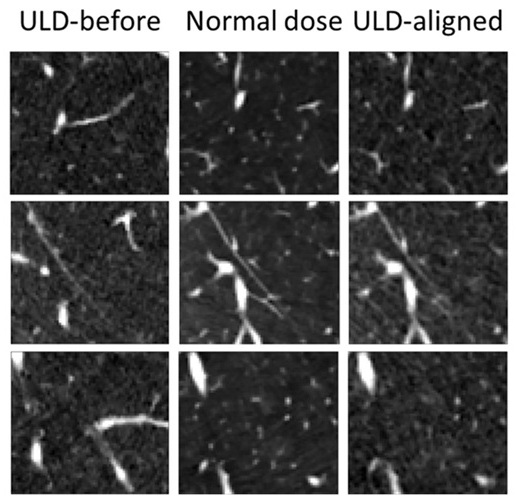
Ultrasound-Based Microscopy Technique to Help Diagnose Small Vessel Diseases
Clinical ultrasound, commonly used in pregnancy scans, provides real-time images of body structures. It is one of the most widely used imaging techniques in medicine, but until recently, it had little... Read moreGeneral/Advanced Imaging
view channel
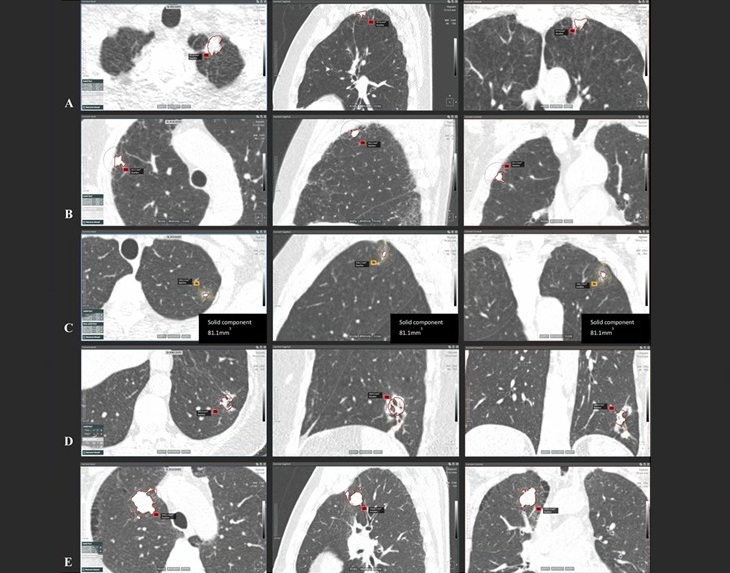
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read more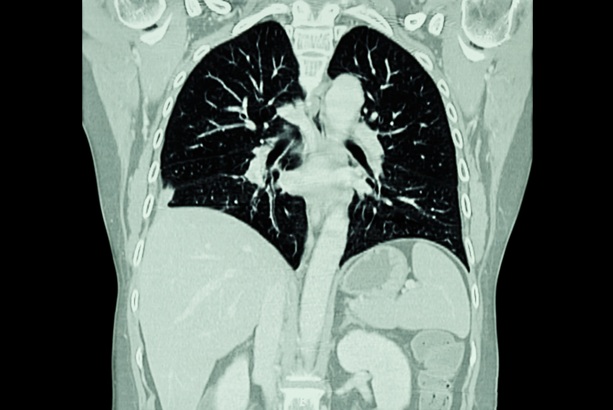
AI Model Significantly Enhances Low-Dose CT Capabilities
Lung cancer remains one of the most challenging diseases, making early diagnosis vital for effective treatment. Fortunately, advancements in artificial intelligence (AI) are revolutionizing lung cancer... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more