PET Scans Reveal How Psychodynamic Therapy for Depressed Patients May Alter Brain Function
|
By MedImaging International staff writers Posted on 19 Nov 2014 |
New imaging findings show that metabolic differences in a major brain region could predict which patients are most likely to respond to psychodynamic therapy.
A study from Massachusetts General Hospital (MGH; Boston, MA, USA) has identified for the first time changes in the metabolic activity of a key brain region in patients successfully treated for depression with psychodynamic psychotherapy, suggesting a process behind one of the most generally significantly and widely practiced forms of therapy. The investigators also found evidence that pretreatment metabolism in a different brain structure might predict which patients are likely to respond to that form of therapy. Their report was published online November 2014 in the journal Psychotherapy and Psychosomatics.
Psychodynamic psychotherapy, believed to be a replacement for Freudian analysis, focuses on how a patient’s earlier life experiences, especially important relationships, influence their character and how they relate to others. By studying a patient’s past and current relationships—including the relationship with the therapist—therapy focuses on helping the patient gain insights that can change both mood and behavior.
“Psychodynamic psychotherapy might be considered the original form of ‘personalized medicine,’ since it draws directly from a patient’s unique experiences to shape the course of treatment,” said Joshua Roffman, MD, MGH department of psychiatry, lead author of the report. “While it has been a core part of psychiatric training for decades and continues to be widely practiced, psychodynamic psychotherapy hasn’t been studied as broadly as have other approaches for a number of reasons, including its greater subjectivity and treatment-by-treatment variability. We do know that psychodynamic treatments are effective for some patients, and this study examined whether differences in neural activity could predict which patients would complete the course of therapy and which would drop out, a common occurrence for any type of therapy.”
The study enrolled 16 patients diagnosed with major depression for whom previous treatment with medication had not been successful. Prior to beginning the therapy program, participants received standardized assessments of their depression symptoms and of psychological mindedness—the capacity to recognize and understand their own emotions, motivations and actions. Before the first therapy session, participants had a PET imaging procedure that assesses metabolic activity within the brain by measuring glucose uptake.
The study protocol involved 16 weekly individual psychodynamic psychotherapy sessions that, while flexible enough to be adapted to individual patients’ needs, followed a predefined theme and sequence. With participants’ permission, sessions were videotaped and later reviewed by another member of the study team, both to insure that sessions followed the defined pattern and to assess how well participants developed new insights through the therapy. Seven participants discontinued therapy while nine completed all therapy sessions, which were followed by a second set of PET images, taken within a week of therapy’s conclusion, and repeat evaluation of depression symptoms.
The PET scans captured before the beginning of therapy revealed that metabolic activity of the right insula—a brain region known to be important for emotional regulation and previously implicated in depression—was higher in participants with more severe depression symptoms. Almost all of those who completed the therapy had a greater than 50% reduction in depression symptoms, although improvement was not clinically evident until after the fourth week of treatment, on average. Reduced metabolic activity within the insula from pre- to post-treatment was associated with greater symptom reduction and was correlated with the degree of insight each participant achieved, as determined by the outside observers.
The pretreatment PET scans also revealed significant metabolic differences in an area called the right precuneus between those who went on to complete the therapy and those who dropped out, with a higher metabolic level being observed in the completers. Activity in the precuneus—which has previously been associated with self-awareness and memory—also was associated with the pretreatment level of psychologic mindedness, a capacity that has been considered fundamental to effective psychodynamic treatment.
“As with all psychiatric interventions, it is notoriously difficult to know ahead of time who is likely to have a good response to psychodynamic psychotherapy and who is not,” said Dr. Roffman, an assistant professor of psychiatry at Harvard Medical School (Boston, MA, USA). “Identification of biological markers that could predict treatment success is a ‘holy grail’ in psychiatry; and while the measured differences in psychological mindedness between completers and non-completers were insignificant, the significant difference in precuneus metabolism suggests that it may a sensitive predictor of treatment response, something that needs to be confirmed in larger trials.”
Related Links:
Massachusetts General Hospital
A study from Massachusetts General Hospital (MGH; Boston, MA, USA) has identified for the first time changes in the metabolic activity of a key brain region in patients successfully treated for depression with psychodynamic psychotherapy, suggesting a process behind one of the most generally significantly and widely practiced forms of therapy. The investigators also found evidence that pretreatment metabolism in a different brain structure might predict which patients are likely to respond to that form of therapy. Their report was published online November 2014 in the journal Psychotherapy and Psychosomatics.
Psychodynamic psychotherapy, believed to be a replacement for Freudian analysis, focuses on how a patient’s earlier life experiences, especially important relationships, influence their character and how they relate to others. By studying a patient’s past and current relationships—including the relationship with the therapist—therapy focuses on helping the patient gain insights that can change both mood and behavior.
“Psychodynamic psychotherapy might be considered the original form of ‘personalized medicine,’ since it draws directly from a patient’s unique experiences to shape the course of treatment,” said Joshua Roffman, MD, MGH department of psychiatry, lead author of the report. “While it has been a core part of psychiatric training for decades and continues to be widely practiced, psychodynamic psychotherapy hasn’t been studied as broadly as have other approaches for a number of reasons, including its greater subjectivity and treatment-by-treatment variability. We do know that psychodynamic treatments are effective for some patients, and this study examined whether differences in neural activity could predict which patients would complete the course of therapy and which would drop out, a common occurrence for any type of therapy.”
The study enrolled 16 patients diagnosed with major depression for whom previous treatment with medication had not been successful. Prior to beginning the therapy program, participants received standardized assessments of their depression symptoms and of psychological mindedness—the capacity to recognize and understand their own emotions, motivations and actions. Before the first therapy session, participants had a PET imaging procedure that assesses metabolic activity within the brain by measuring glucose uptake.
The study protocol involved 16 weekly individual psychodynamic psychotherapy sessions that, while flexible enough to be adapted to individual patients’ needs, followed a predefined theme and sequence. With participants’ permission, sessions were videotaped and later reviewed by another member of the study team, both to insure that sessions followed the defined pattern and to assess how well participants developed new insights through the therapy. Seven participants discontinued therapy while nine completed all therapy sessions, which were followed by a second set of PET images, taken within a week of therapy’s conclusion, and repeat evaluation of depression symptoms.
The PET scans captured before the beginning of therapy revealed that metabolic activity of the right insula—a brain region known to be important for emotional regulation and previously implicated in depression—was higher in participants with more severe depression symptoms. Almost all of those who completed the therapy had a greater than 50% reduction in depression symptoms, although improvement was not clinically evident until after the fourth week of treatment, on average. Reduced metabolic activity within the insula from pre- to post-treatment was associated with greater symptom reduction and was correlated with the degree of insight each participant achieved, as determined by the outside observers.
The pretreatment PET scans also revealed significant metabolic differences in an area called the right precuneus between those who went on to complete the therapy and those who dropped out, with a higher metabolic level being observed in the completers. Activity in the precuneus—which has previously been associated with self-awareness and memory—also was associated with the pretreatment level of psychologic mindedness, a capacity that has been considered fundamental to effective psychodynamic treatment.
“As with all psychiatric interventions, it is notoriously difficult to know ahead of time who is likely to have a good response to psychodynamic psychotherapy and who is not,” said Dr. Roffman, an assistant professor of psychiatry at Harvard Medical School (Boston, MA, USA). “Identification of biological markers that could predict treatment success is a ‘holy grail’ in psychiatry; and while the measured differences in psychological mindedness between completers and non-completers were insignificant, the significant difference in precuneus metabolism suggests that it may a sensitive predictor of treatment response, something that needs to be confirmed in larger trials.”
Related Links:
Massachusetts General Hospital
Latest Nuclear Medicine News
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
- Combining Advanced Imaging Technologies Offers Breakthrough in Glioblastoma Treatment
- New Molecular Imaging Agent Accurately Identifies Crucial Cancer Biomarker
- New Scans Light Up Aggressive Tumors for Better Treatment
- AI Stroke Brain Scan Readings Twice as Accurate as Current Method
- AI Analysis of PET/CT Images Predicts Side Effects of Immunotherapy in Lung Cancer
- New Imaging Agent to Drive Step-Change for Brain Cancer Imaging
- Portable PET Scanner to Detect Earliest Stages of Alzheimer’s Disease
- New Immuno-PET Imaging Technique Identifies Glioblastoma Patients Who Would Benefit from Immunotherapy
Channels
Radiography
view channel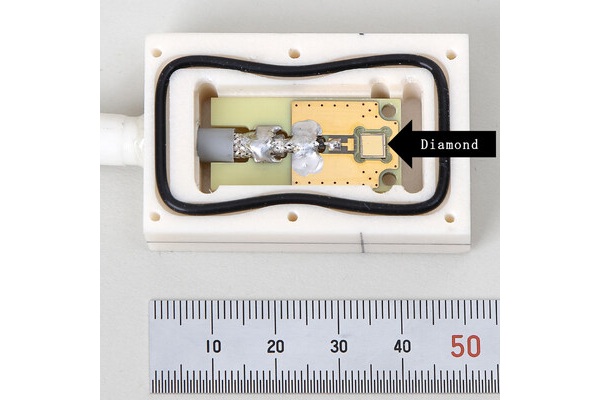
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read more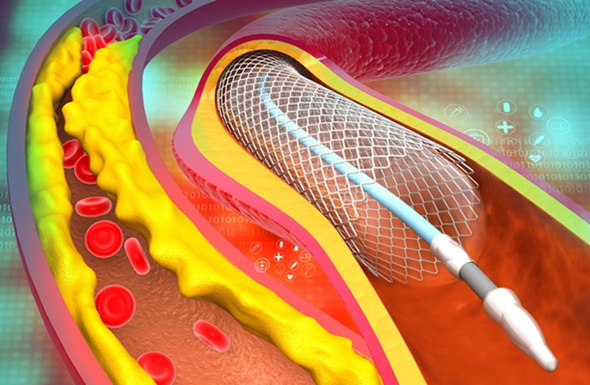
AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure where small metal tubes called stents are inserted into partially blocked coronary arteries... Read moreMRI
view channel
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read more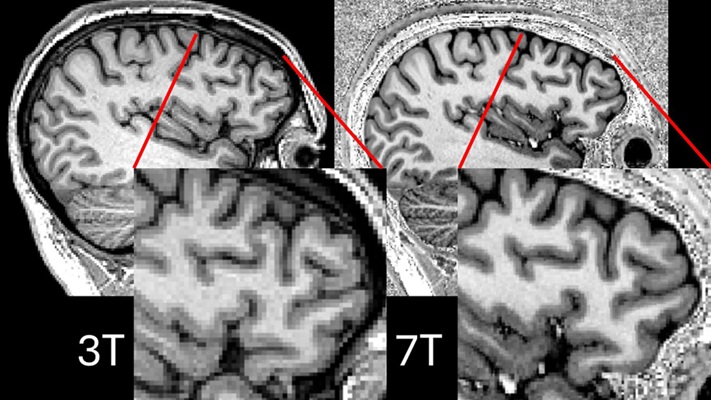
Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
Approximately 360,000 individuals in the UK suffer from focal epilepsy, a condition in which seizures spread from one part of the brain. Around a third of these patients experience persistent seizures... Read more
AI-Powered MRI Technology Improves Parkinson’s Diagnoses
Current research shows that the accuracy of diagnosing Parkinson’s disease typically ranges from 55% to 78% within the first five years of assessment. This is partly due to the similarities shared by Parkinson’s... Read more
Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
Artificial intelligence (AI) technologies are transforming the way medical images are analyzed, offering unprecedented capabilities in quantitatively extracting features that go beyond traditional visual... Read moreUltrasound
view channel
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read more
Novel Imaging Method Enables Early Diagnosis and Treatment Monitoring of Type 2 Diabetes
Type 2 diabetes is recognized as an autoimmune inflammatory disease, where chronic inflammation leads to alterations in pancreatic islet microvasculature, a key factor in β-cell dysfunction.... Read moreGeneral/Advanced Imaging
view channel
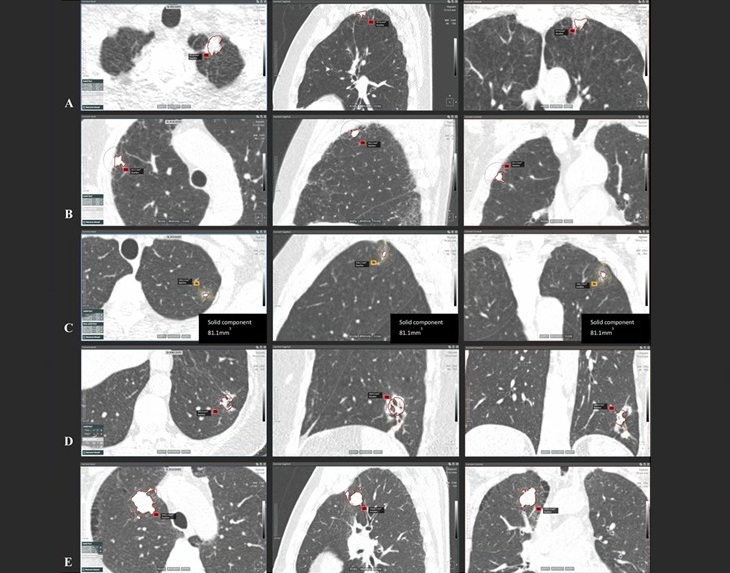
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read more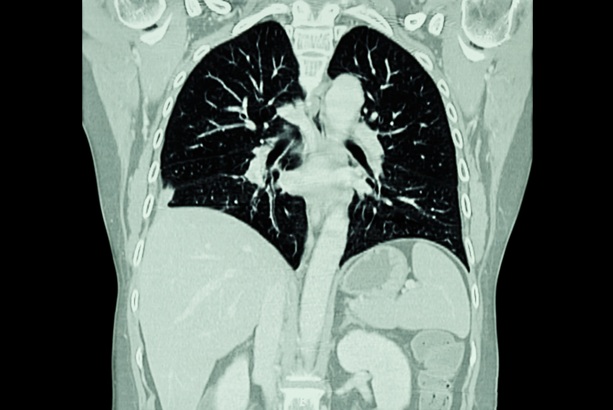
AI Model Significantly Enhances Low-Dose CT Capabilities
Lung cancer remains one of the most challenging diseases, making early diagnosis vital for effective treatment. Fortunately, advancements in artificial intelligence (AI) are revolutionizing lung cancer... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more