Radiotherapy After Mastectomy Helpful to Women with Breast Cancer That Metastasized to Only a Few Lymph Nodes
|
By MedImaging International staff writers Posted on 03 Apr 2014 |

Image: A new study by Oxford scientists has found that thousands more women with breast cancer should be given radiotherapy as part of their treatment for the disease (Photo courtesy of GlowImages / Corbis).
Women whose breast cancer has metastasized to only a few lymph nodes under their arm are less likely to have a recurrence of their disease or to die from it if they have radiotherapy after mastectomy, according to new findings.
Paul McGale, PhD, a senior statistician in the Early Breast Cancer Trialists’ Collaborative Group at the Clinical Trial Service Unit (CTSU) at Oxford University (UK), presented his findings March 19, 2014,at the European Breast Cancer Conference (EBCC-9), held in Glasgow (UK), and published March 19, 2014, in the Lancet, that, until now, there has been uncertainty over whether women with early breast cancer that has spread to just one, two, or three lymph nodes under the arm gain any benefit from radiotherapy after surgery. However, his findings revealed that radiotherapy improves their risks of remaining disease-free and slashes their chance of dying from breast cancer.
“Another result from our study is that the proportional benefits of radiotherapy were similar in women regardless of whether or not they had also received chemotherapy or hormonal therapy. This is important because most women today receive these therapies. Our results suggest that women being treated today are likely also to benefit from radiotherapy if they have any positive lymph nodes,” Dr. McGale stated.
Dr. McGale analyzed results from 3,786 women in 14 randomized trials starting between 1964–1982, who had been given mastectomies along with the surgical removal of lymph nodes under the arm (axillary dissection) and who were then randomized to receive either radiotherapy to the chest wall and surrounding regions or to no radiotherapy. The women fell into three categories: those with no cancer in the lymph nodes, those with cancer in one, two or three lymph nodes, and those with cancer in four or more lymph nodes. The women were followed up for an average of just over 11 years, and data on the number of recurrences and deaths were available up to 2009.
“In 700 women in whom the pathologists could find no sign that the nodes were affected, radiotherapy did not reduce the risk of recurrence or of dying from breast cancer,” said Dr. McGale. “However, in the 1,314 women who had between one and three positive nodes, radiotherapy reduced the recurrence rate by nearly a third [32%] and the breast cancer death rate by a fifth [20%]. Giving radiotherapy to these women led to nearly 12 fewer recurrences of breast cancer per 100 women after 10 years, and eight fewer deaths per 100 women after 20 years.”
Dr. McGale discovered that the percentage declines in the recurrence and death rates in the 405 women who had only one positive node were similar to those for the women who had two or three positive nodes.
For the 1,772 women with four or more positive nodes, radiotherapy also reduced the recurrence rate (by 21%) and the breast cancer death rate (by 13%). In this instance, radiotherapy for these women led to nine fewer recurrences of breast cancer after 10 years and nine fewer deaths after 20 years per 100 women. “It is already accepted that women with four or more positive nodes benefit from radiotherapy after mastectomy, and these findings confirm this benefit,” Dr. McGale said. “However, it is for women with between one and three positive nodes where the previous evidence has been unclear.”
The benefit occurred regardless of whether the women were in trials where hormonal therapy or chemotherapy was given to all women. Sixty-five percent of women with one, two, or three positive nodes received chemotherapy, and an additional 21% with hormone-sensitive tumors received hormonal therapy.
Dr. Carolyn Taylor, FRCR, a clinical oncologist in the Early Breast Cancer Trialists’ Collaborative Group, speaking before the conference, said, “In the past, most women with many positive lymph nodes were given chemotherapy, but usually those with few positive nodes were not. In recent years, larger numbers of women with just a few positive lymph nodes have received chemotherapy, and the types of chemotherapy have changed. Also, the vast majority of women with hormone-sensitive tumors are now given hormonal therapy. We will have to wait for results from new trials to observe directly the long-term effects of modern radiotherapy in women who are given modern chemotherapy and hormonal therapy. However, it is likely that the percentage reductions in disease recurrence and breast cancer mortality from today’s radiotherapy will be at least as big as the benefits seen here.”
Dr. McGale concluded, “Since the time when the women in these trials were randomized there have been advances in radiotherapy and also in breast screening, surgery, lymph node staging, and systemic therapy. So the absolute benefits from postmastectomy radiotherapy today may be smaller than those we have reported here. But the proportional benefits from radiotherapy are likely to be at least as big.”
To study this and further follow-up on their findings, Dr. McGale, Dr. Taylor and their colleagues are inviting investigators of more recent trials comparing different radiotherapy regimens to contribute data to the Early Breast Cancer Trialists’ Group.
Prof. David Cameron, from the University of Edinburgh (UK), who is a member of the EBCC-9 executive scientific committee, commented, “These data highlight the power of combining information from individual patients recruited into a number of different clinical trials. The benefit of radiotherapy in women who needed a mastectomy for node positive breast cancer is now becoming clear; more data will emerge in a few years from the UK-led SUPREMO trial, which prospectively addresses this question for the exact same group of women that are the subject of this study.”
The 3,786 women were part of a larger group of 8,135 women in 22 randomized trials starting before 2000. During the follow-up period, 5,424 (67%) were known to have died, and the extent of surgery was known for all but 183 (2%) of the women.
Related Links:
Clinical Trial Service Unit at Oxford University
Paul McGale, PhD, a senior statistician in the Early Breast Cancer Trialists’ Collaborative Group at the Clinical Trial Service Unit (CTSU) at Oxford University (UK), presented his findings March 19, 2014,at the European Breast Cancer Conference (EBCC-9), held in Glasgow (UK), and published March 19, 2014, in the Lancet, that, until now, there has been uncertainty over whether women with early breast cancer that has spread to just one, two, or three lymph nodes under the arm gain any benefit from radiotherapy after surgery. However, his findings revealed that radiotherapy improves their risks of remaining disease-free and slashes their chance of dying from breast cancer.
“Another result from our study is that the proportional benefits of radiotherapy were similar in women regardless of whether or not they had also received chemotherapy or hormonal therapy. This is important because most women today receive these therapies. Our results suggest that women being treated today are likely also to benefit from radiotherapy if they have any positive lymph nodes,” Dr. McGale stated.
Dr. McGale analyzed results from 3,786 women in 14 randomized trials starting between 1964–1982, who had been given mastectomies along with the surgical removal of lymph nodes under the arm (axillary dissection) and who were then randomized to receive either radiotherapy to the chest wall and surrounding regions or to no radiotherapy. The women fell into three categories: those with no cancer in the lymph nodes, those with cancer in one, two or three lymph nodes, and those with cancer in four or more lymph nodes. The women were followed up for an average of just over 11 years, and data on the number of recurrences and deaths were available up to 2009.
“In 700 women in whom the pathologists could find no sign that the nodes were affected, radiotherapy did not reduce the risk of recurrence or of dying from breast cancer,” said Dr. McGale. “However, in the 1,314 women who had between one and three positive nodes, radiotherapy reduced the recurrence rate by nearly a third [32%] and the breast cancer death rate by a fifth [20%]. Giving radiotherapy to these women led to nearly 12 fewer recurrences of breast cancer per 100 women after 10 years, and eight fewer deaths per 100 women after 20 years.”
Dr. McGale discovered that the percentage declines in the recurrence and death rates in the 405 women who had only one positive node were similar to those for the women who had two or three positive nodes.
For the 1,772 women with four or more positive nodes, radiotherapy also reduced the recurrence rate (by 21%) and the breast cancer death rate (by 13%). In this instance, radiotherapy for these women led to nine fewer recurrences of breast cancer after 10 years and nine fewer deaths after 20 years per 100 women. “It is already accepted that women with four or more positive nodes benefit from radiotherapy after mastectomy, and these findings confirm this benefit,” Dr. McGale said. “However, it is for women with between one and three positive nodes where the previous evidence has been unclear.”
The benefit occurred regardless of whether the women were in trials where hormonal therapy or chemotherapy was given to all women. Sixty-five percent of women with one, two, or three positive nodes received chemotherapy, and an additional 21% with hormone-sensitive tumors received hormonal therapy.
Dr. Carolyn Taylor, FRCR, a clinical oncologist in the Early Breast Cancer Trialists’ Collaborative Group, speaking before the conference, said, “In the past, most women with many positive lymph nodes were given chemotherapy, but usually those with few positive nodes were not. In recent years, larger numbers of women with just a few positive lymph nodes have received chemotherapy, and the types of chemotherapy have changed. Also, the vast majority of women with hormone-sensitive tumors are now given hormonal therapy. We will have to wait for results from new trials to observe directly the long-term effects of modern radiotherapy in women who are given modern chemotherapy and hormonal therapy. However, it is likely that the percentage reductions in disease recurrence and breast cancer mortality from today’s radiotherapy will be at least as big as the benefits seen here.”
Dr. McGale concluded, “Since the time when the women in these trials were randomized there have been advances in radiotherapy and also in breast screening, surgery, lymph node staging, and systemic therapy. So the absolute benefits from postmastectomy radiotherapy today may be smaller than those we have reported here. But the proportional benefits from radiotherapy are likely to be at least as big.”
To study this and further follow-up on their findings, Dr. McGale, Dr. Taylor and their colleagues are inviting investigators of more recent trials comparing different radiotherapy regimens to contribute data to the Early Breast Cancer Trialists’ Group.
Prof. David Cameron, from the University of Edinburgh (UK), who is a member of the EBCC-9 executive scientific committee, commented, “These data highlight the power of combining information from individual patients recruited into a number of different clinical trials. The benefit of radiotherapy in women who needed a mastectomy for node positive breast cancer is now becoming clear; more data will emerge in a few years from the UK-led SUPREMO trial, which prospectively addresses this question for the exact same group of women that are the subject of this study.”
The 3,786 women were part of a larger group of 8,135 women in 22 randomized trials starting before 2000. During the follow-up period, 5,424 (67%) were known to have died, and the extent of surgery was known for all but 183 (2%) of the women.
Related Links:
Clinical Trial Service Unit at Oxford University
Latest Nuclear Medicine News
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
- Combining Advanced Imaging Technologies Offers Breakthrough in Glioblastoma Treatment
- New Molecular Imaging Agent Accurately Identifies Crucial Cancer Biomarker
- New Scans Light Up Aggressive Tumors for Better Treatment
- AI Stroke Brain Scan Readings Twice as Accurate as Current Method
- AI Analysis of PET/CT Images Predicts Side Effects of Immunotherapy in Lung Cancer
- New Imaging Agent to Drive Step-Change for Brain Cancer Imaging
- Portable PET Scanner to Detect Earliest Stages of Alzheimer’s Disease
- New Immuno-PET Imaging Technique Identifies Glioblastoma Patients Who Would Benefit from Immunotherapy
Channels
Radiography
view channel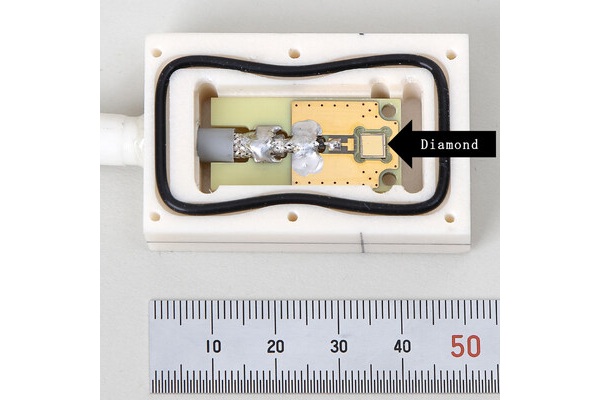
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read more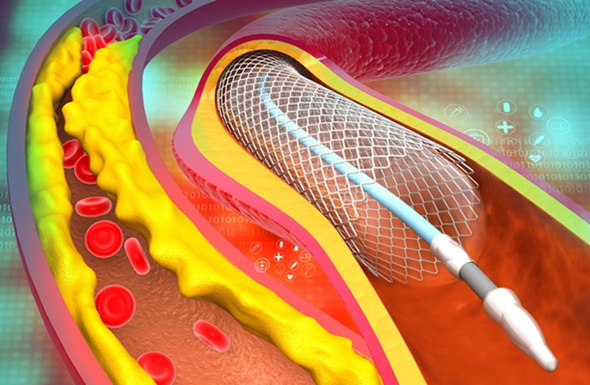
AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure where small metal tubes called stents are inserted into partially blocked coronary arteries... Read moreMRI
view channel
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read more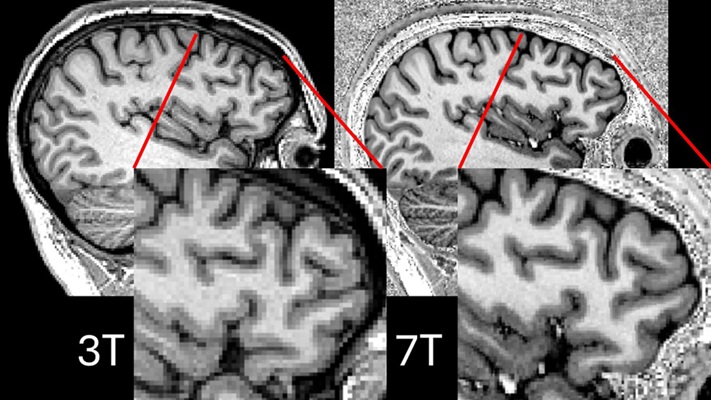
Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
Approximately 360,000 individuals in the UK suffer from focal epilepsy, a condition in which seizures spread from one part of the brain. Around a third of these patients experience persistent seizures... Read more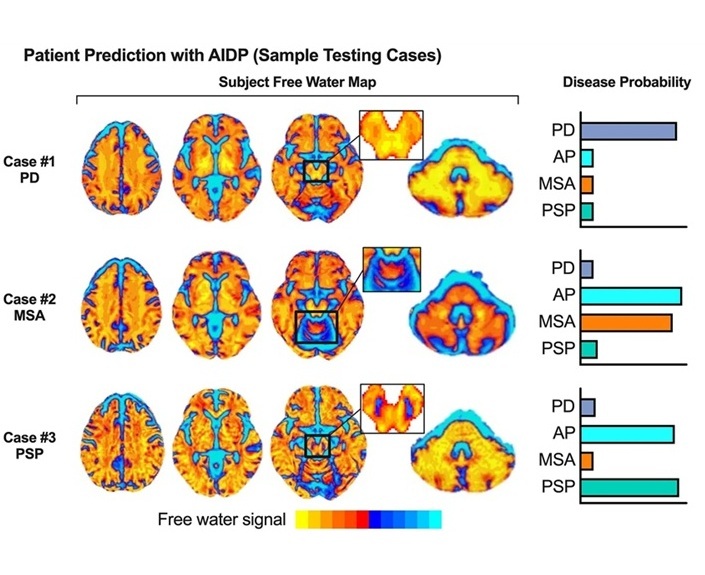
AI-Powered MRI Technology Improves Parkinson’s Diagnoses
Current research shows that the accuracy of diagnosing Parkinson’s disease typically ranges from 55% to 78% within the first five years of assessment. This is partly due to the similarities shared by Parkinson’s... Read more
Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
Artificial intelligence (AI) technologies are transforming the way medical images are analyzed, offering unprecedented capabilities in quantitatively extracting features that go beyond traditional visual... Read moreUltrasound
view channel
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read more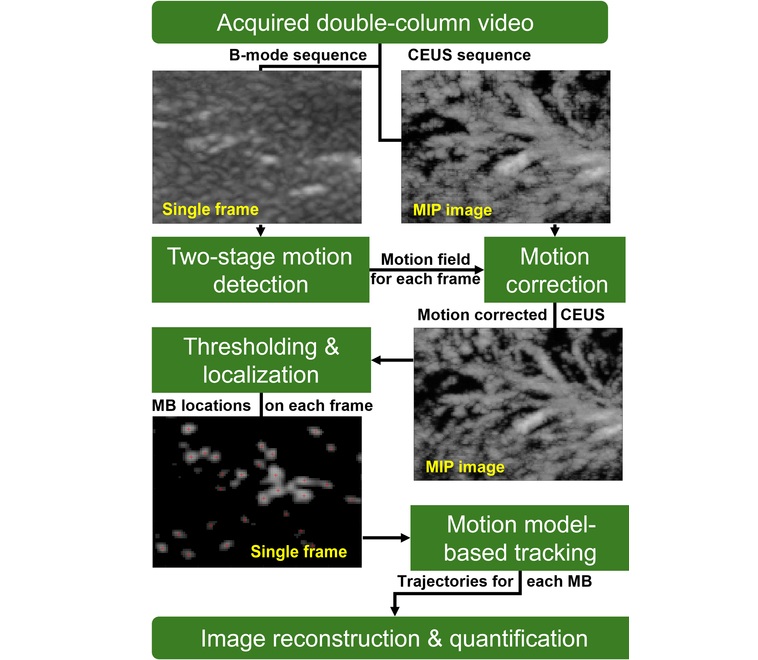
Novel Imaging Method Enables Early Diagnosis and Treatment Monitoring of Type 2 Diabetes
Type 2 diabetes is recognized as an autoimmune inflammatory disease, where chronic inflammation leads to alterations in pancreatic islet microvasculature, a key factor in β-cell dysfunction.... Read moreGeneral/Advanced Imaging
view channel
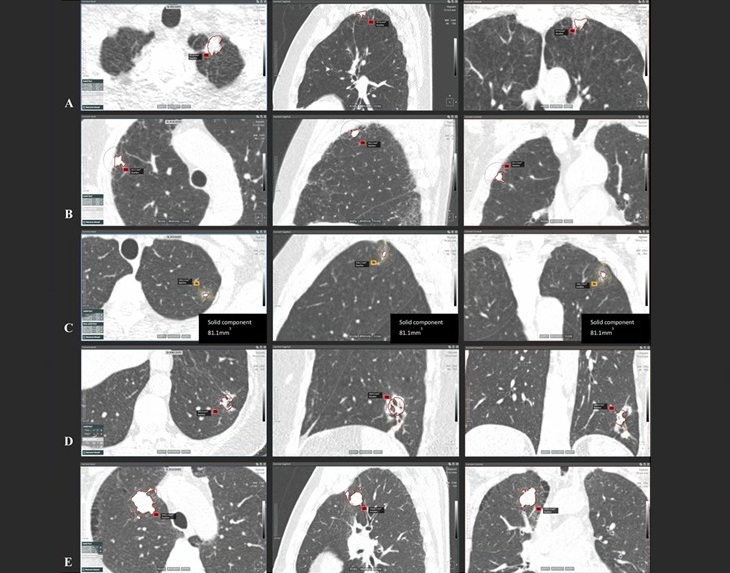
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read more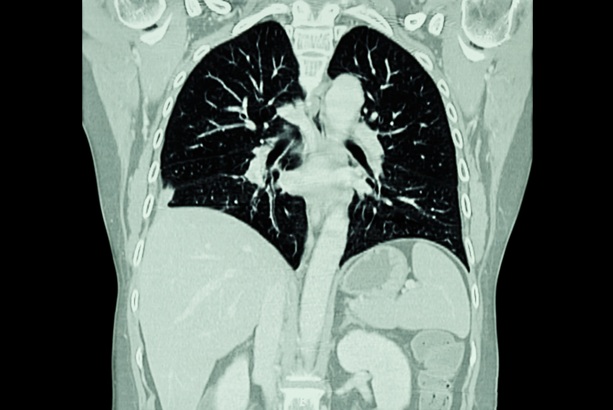
AI Model Significantly Enhances Low-Dose CT Capabilities
Lung cancer remains one of the most challenging diseases, making early diagnosis vital for effective treatment. Fortunately, advancements in artificial intelligence (AI) are revolutionizing lung cancer... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more