Younger, Just Diagnosed Breast Cancer Patients Often Undergo Unnecessary Imaging, Staging Procedures
|
By MedImaging International staff writers Posted on 08 Jan 2014 |
More than a third of younger, early-stage breast cancer patients undergo unnecessary imaging procedures, including position emission tomography (PET), computed tomography (CT), nuclear medicine bone scans (NMBS), and tumor markers (TMs) at the time of staging and diagnosis, according to new findings.
The new research was presented at the 2013 CTRC-AACR San Antonio (TX, USA) Breast Cancer Symposium, by Carlos Barcenas, MD, assistant professor at the University of Texas MD Anderson Cancer Center (Houston, TX, USA) breast medical oncology department. The study is the first to examine the issue of overuse of staging procedures, including imaging and tumor markers in the diagnosis setting, specifically in younger, early-stage breast cancer patients.
Over-testing and unnecessary procedures extends beyond cancer care across the healthcare continuum. To help tackle the issue, the American Board of Internal Medicine began “Choosing Wisely,” an initiative encouraging physicians and patients to have conversations that encourage its reduction.
In 2012, the American Society of Clinical Oncology (ASCO) generated a “top five list,” which recommended against the use of CT, PET, TM, and NMBS in the diagnosis and staging of early-stage breast cancer at low risk for metastasis. Instead, treatment guidelines clearly state that for women with early-stage breast cancer, the proper procedures for diagnosis include mammogram, ultrasound, clinical exam, and blood work, according to Dr. Barcenas.
“We’ve known that overuse of staging procedures is a problem as well it may affect the cost-effectiveness in diagnosing women with early breast cancer,” said Dr. Barcenas. “With ASCO’s inclusion of this issue in its top five recommendations last year as part of its ‘Choosing Wisely’ campaign, this gave us the idea for the study: to investigate and understand just how pervasive the problem really is.”
For the retrospective study, Dr. Barcenas and coworkers analyzed claims from a national employer-based database of 42,651 women between 2005 and 2010 with an initial diagnosis of breast cancer. All were younger than 65 years old and had undergone a mastectomy, lumpectomy and sentinel lymph node biopsy. Patients who underwent axillary lymph node dissection were excluded from the study because this is considered a surrogate for node-positive disease. Claims for imaging and tumor markers were analyzed between the specific period of three months prior to surgery and one month post-surgery. Researchers stratified for age, geographic location, treatment, and insurance coverage.
The researchers found that 37% of early stage breast-cancer patients had at least one claim for an unnecessary staging test, with minimal change in rate of that average over the five-year period. Of significance, according to Dr. Barcenas, 18% of the woman had tumor markers performed, which is a staging procedure with no role in the nonmetastatic diagnosis setting. Undergoing chemotherapy had the highest link to overuse of staging procedures, with hormone and radiation therapy also associated with overuse.
The investigators also found regional differences in overuse trends, as well a higher rate of unnecessary procedures in women with PPO (preferred provider organization) insurance coverage compared to those with HMO (health maintenance organization). Moreover, women with breast cancer under 35 years old were at higher changes of having one of these tests, they explained. However, when diagnosed at such a young age, this patient population is perceived by the physician to be at higher risk of metastatic and/or aggressive disease.
“While hypothesis-generating, our study is not without limitations. For example, we don't know the receptor status of the tumor, or if the patients had a more aggressive pathology, such as triple negative disease, or if they presented with specific clinical characteristics such as back pain or an elevated blood level of a liver function test that called for more investigation. In some instances, there will be justification for the additional imaging procedures,” said Dr. Barcenas.
The researchers plan to track this trend to see if the rate of unnecessary imaging decreases with the continued propagation of the “Choosing Wisely” campaign. They also plan to evaluate for cost effectiveness.
Sharon Giordano, MD, professor and chair, health services research at MD Anderson believes the findings plainly support the need for the ASCO recommendations. She said the research shed some light on the issue of over-use and over-care and offers confirmation to physicians so that they have consent not to order unnecessary tests. “Often, doctors think they’re not being good to their patients if they don’t do all they can. Yet there’s been a shift in focus to doing what matters for the patient and what’s proven to improve outcomes, rather than testing for the sake of testing,” said Dr. Giordano, also a professor of breast medical oncology and the study’s senior author. “Ultimately, our goal is to bring the best care and value care to our patients.”
Related Links:
University of Texas MD Anderson Cancer Center
The new research was presented at the 2013 CTRC-AACR San Antonio (TX, USA) Breast Cancer Symposium, by Carlos Barcenas, MD, assistant professor at the University of Texas MD Anderson Cancer Center (Houston, TX, USA) breast medical oncology department. The study is the first to examine the issue of overuse of staging procedures, including imaging and tumor markers in the diagnosis setting, specifically in younger, early-stage breast cancer patients.
Over-testing and unnecessary procedures extends beyond cancer care across the healthcare continuum. To help tackle the issue, the American Board of Internal Medicine began “Choosing Wisely,” an initiative encouraging physicians and patients to have conversations that encourage its reduction.
In 2012, the American Society of Clinical Oncology (ASCO) generated a “top five list,” which recommended against the use of CT, PET, TM, and NMBS in the diagnosis and staging of early-stage breast cancer at low risk for metastasis. Instead, treatment guidelines clearly state that for women with early-stage breast cancer, the proper procedures for diagnosis include mammogram, ultrasound, clinical exam, and blood work, according to Dr. Barcenas.
“We’ve known that overuse of staging procedures is a problem as well it may affect the cost-effectiveness in diagnosing women with early breast cancer,” said Dr. Barcenas. “With ASCO’s inclusion of this issue in its top five recommendations last year as part of its ‘Choosing Wisely’ campaign, this gave us the idea for the study: to investigate and understand just how pervasive the problem really is.”
For the retrospective study, Dr. Barcenas and coworkers analyzed claims from a national employer-based database of 42,651 women between 2005 and 2010 with an initial diagnosis of breast cancer. All were younger than 65 years old and had undergone a mastectomy, lumpectomy and sentinel lymph node biopsy. Patients who underwent axillary lymph node dissection were excluded from the study because this is considered a surrogate for node-positive disease. Claims for imaging and tumor markers were analyzed between the specific period of three months prior to surgery and one month post-surgery. Researchers stratified for age, geographic location, treatment, and insurance coverage.
The researchers found that 37% of early stage breast-cancer patients had at least one claim for an unnecessary staging test, with minimal change in rate of that average over the five-year period. Of significance, according to Dr. Barcenas, 18% of the woman had tumor markers performed, which is a staging procedure with no role in the nonmetastatic diagnosis setting. Undergoing chemotherapy had the highest link to overuse of staging procedures, with hormone and radiation therapy also associated with overuse.
The investigators also found regional differences in overuse trends, as well a higher rate of unnecessary procedures in women with PPO (preferred provider organization) insurance coverage compared to those with HMO (health maintenance organization). Moreover, women with breast cancer under 35 years old were at higher changes of having one of these tests, they explained. However, when diagnosed at such a young age, this patient population is perceived by the physician to be at higher risk of metastatic and/or aggressive disease.
“While hypothesis-generating, our study is not without limitations. For example, we don't know the receptor status of the tumor, or if the patients had a more aggressive pathology, such as triple negative disease, or if they presented with specific clinical characteristics such as back pain or an elevated blood level of a liver function test that called for more investigation. In some instances, there will be justification for the additional imaging procedures,” said Dr. Barcenas.
The researchers plan to track this trend to see if the rate of unnecessary imaging decreases with the continued propagation of the “Choosing Wisely” campaign. They also plan to evaluate for cost effectiveness.
Sharon Giordano, MD, professor and chair, health services research at MD Anderson believes the findings plainly support the need for the ASCO recommendations. She said the research shed some light on the issue of over-use and over-care and offers confirmation to physicians so that they have consent not to order unnecessary tests. “Often, doctors think they’re not being good to their patients if they don’t do all they can. Yet there’s been a shift in focus to doing what matters for the patient and what’s proven to improve outcomes, rather than testing for the sake of testing,” said Dr. Giordano, also a professor of breast medical oncology and the study’s senior author. “Ultimately, our goal is to bring the best care and value care to our patients.”
Related Links:
University of Texas MD Anderson Cancer Center
Latest Radiography News
- World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
- AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
- Higher Chest X-Ray Usage Catches Lung Cancer Earlier and Improves Survival
- AI-Powered Mammograms Predict Cardiovascular Risk
- Generative AI Model Significantly Reduces Chest X-Ray Reading Time
- AI-Powered Mammography Screening Boosts Cancer Detection in Single-Reader Settings
- Photon Counting Detectors Promise Fast Color X-Ray Images
- AI Can Flag Mammograms for Supplemental MRI
- 3D CT Imaging from Single X-Ray Projection Reduces Radiation Exposure
- AI Method Accurately Predicts Breast Cancer Risk by Analyzing Multiple Mammograms
- Printable Organic X-Ray Sensors Could Transform Treatment for Cancer Patients
- Highly Sensitive, Foldable Detector to Make X-Rays Safer
- Novel Breast Cancer Screening Technology Could Offer Superior Alternative to Mammogram
- Artificial Intelligence Accurately Predicts Breast Cancer Years Before Diagnosis
- AI-Powered Chest X-Ray Detects Pulmonary Nodules Three Years Before Lung Cancer Symptoms
- AI Model Identifies Vertebral Compression Fractures in Chest Radiographs
Channels
MRI
view channel
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read more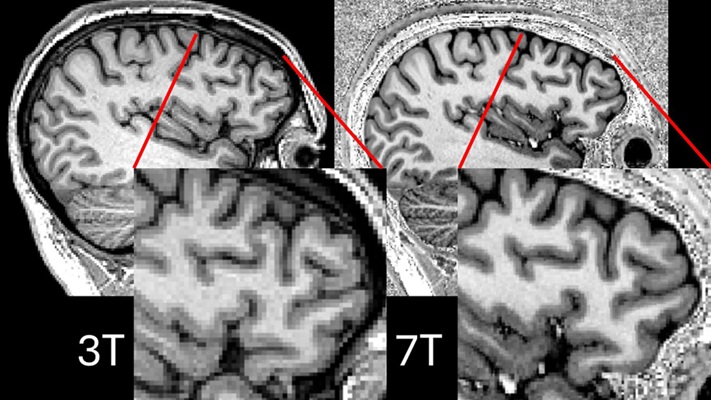
Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
Approximately 360,000 individuals in the UK suffer from focal epilepsy, a condition in which seizures spread from one part of the brain. Around a third of these patients experience persistent seizures... Read more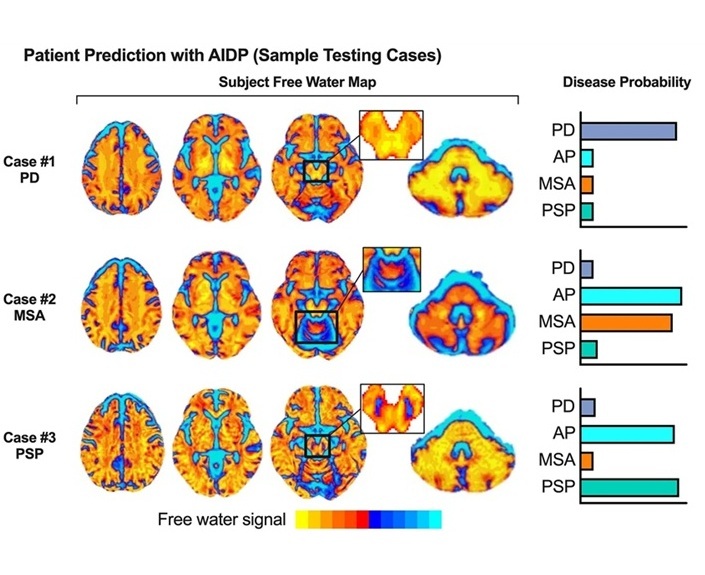
AI-Powered MRI Technology Improves Parkinson’s Diagnoses
Current research shows that the accuracy of diagnosing Parkinson’s disease typically ranges from 55% to 78% within the first five years of assessment. This is partly due to the similarities shared by Parkinson’s... Read more
Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
Artificial intelligence (AI) technologies are transforming the way medical images are analyzed, offering unprecedented capabilities in quantitatively extracting features that go beyond traditional visual... Read moreUltrasound
view channel
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read more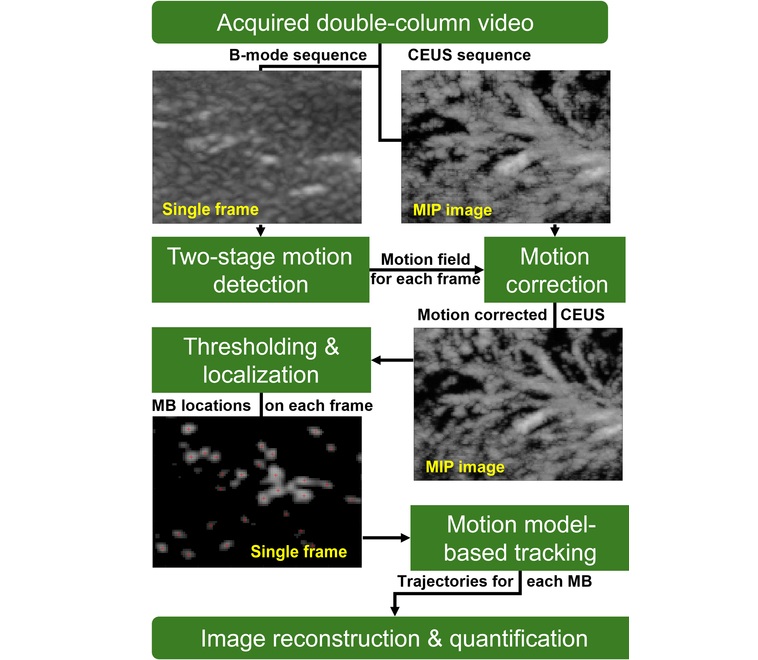
Novel Imaging Method Enables Early Diagnosis and Treatment Monitoring of Type 2 Diabetes
Type 2 diabetes is recognized as an autoimmune inflammatory disease, where chronic inflammation leads to alterations in pancreatic islet microvasculature, a key factor in β-cell dysfunction.... Read moreNuclear Medicine
view channel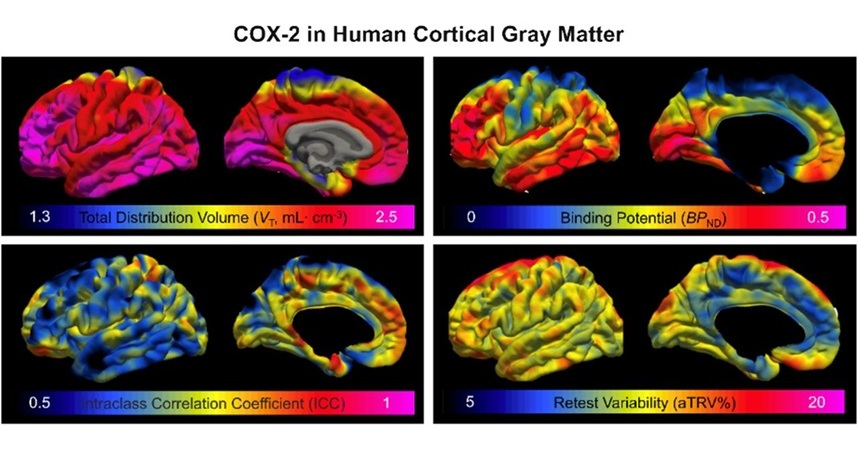
Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
COX-2, an enzyme that plays a key role in brain inflammation, can be significantly upregulated by inflammatory stimuli and neuroexcitation. Researchers suggest that COX-2 density in the brain could serve... Read more
Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC), which represents 15-20% of all breast cancer cases, is one of the most aggressive subtypes, with a five-year survival rate of about 40%. Due to its significant heterogeneity... Read moreGeneral/Advanced Imaging
view channel
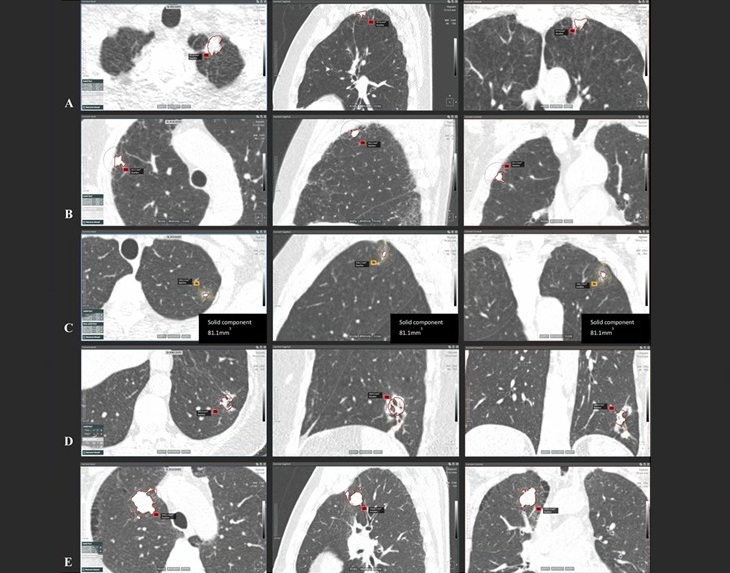
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read more
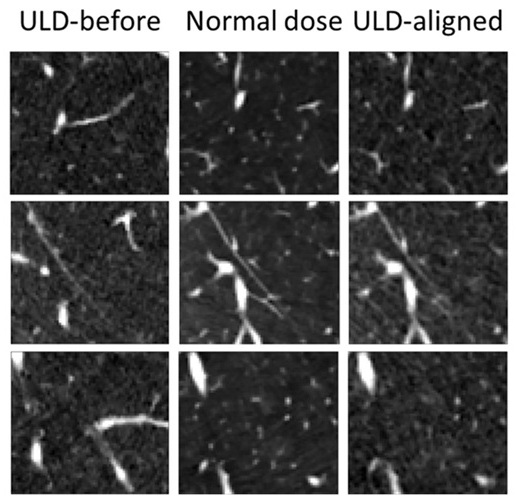
AI Model Significantly Enhances Low-Dose CT Capabilities
Lung cancer remains one of the most challenging diseases, making early diagnosis vital for effective treatment. Fortunately, advancements in artificial intelligence (AI) are revolutionizing lung cancer... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more