Potential in MRI and PET-CT Lymphoma Cancer Characterization
|
By MedImaging International staff writers Posted on 01 Apr 2013 |
Image: T1- and T2-weighted MR images of focal lesions before and after systemic treatment (Photo courtesy of Dr. Jens Hillengass, German Cancer Research Center in Heidelberg, Germany).
Image: Pre-treatment image of a patient with uptake in a mediastinal mass (Photo courtesy of Dr. Sally Barrington, London’s St. Thomas’ PET Imaging Center, UK).
Image: Complete metabolic response on interim PET scan (Photo courtesy of Dr. Sally Barrington, London’s St. Thomas’ PET Imaging Center, UK).
Images: Pre-treatment image of a patient with uptake in a mediastinal mass (Photo courtesy of Dr. Sally Barrington, London’s St. Thomas’ PET Imaging Center, UK).
Image: High-grade uptake on interim PET scan indicating chemoresistance (Photo courtesy of Dr. Sally Barrington, London’s St. Thomas’ PET Imaging Center, UK).
Utilizing magnetic resonance imaging (MRI) in disease evaluation and positron emission computed tomography-computed tomography (PET-CT) imaging in therapy response assessment could optimize patient outcome in lymphoma cancer.
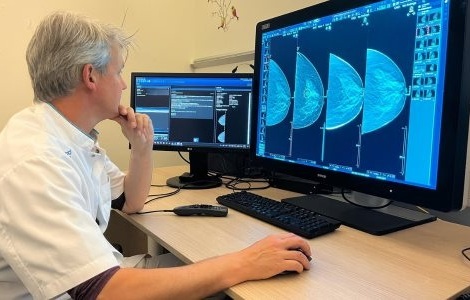
“MRI gives us more information and is probably the most important imaging technique in assessing disease activity in myeloma,” said Dr. Jens Hillengass, a physician scientist from the German Cancer Research Center (Heidelberg, Germany) who presented his findings on March 9, 2013, during the State of the Art symposium at the European Congress of Radiology (ECR), held in Vienna (Austria).
Current guidelines for the evaluation of therapy response are chiefly based on serologic markers and reference imaging to track large soft-tissue tumors. However, Dr. Hillengass thinks that imaging, and in particular MRI and PET, should be included in the recommendations, at least in some patients. For instance, many myeloma patients show changes on MRI that are not visible on a skeletal survey. MRI helps to differentiate between bone and bone marrow; it also has higher sensitivity for imaging of bone marrow effects in total, and demonstrates the first infiltration of plasma cells before overstimulation of osteoclasts and the resulting bone destruction.
Recent research indicates that some patients show diffuse infiltration of bone marrow with malignant plasma cells while others show focal infiltration. Several studies have looked at the prognostic significance of findings from MRI and PET, and suggest that a higher number of focal lesions are associated with a worse prognosis, Dr. Hillengass explained. His research group found that if focal lesions in bone marrow disappear upon MRI, then the patient outcome is better than if remission is defined according to serological markers. Being able to show that lesions are still there could help indicate relapse, which is the case for most patients.
If additional indications suggest that MRI can be used to evaluate disease activity and the extent of bone marrow infiltration with plasma cells prior to bone destruction, there might be a stronger case for earlier treatment, before bone destruction has started, Dr. Hillengass believes. “There are good data to say that if lesions persist, then treatment should continue; these data are on high-risk disease based on cytogenetics, and suggest treating patients for a long time is beneficial,” he said.
Interim PET could be used to monitor response-adapted therapy in Hodgkin lymphoma and aggressive non-Hodgkin lymphoma, according to Dr. Sally Barrington, a consultant physician in nuclear medicine at London’s St. Thomas’ PET Imaging Center (UK), who also spoke during the symposium.
PET was added to new response criteria for lymphoma in 2007 for assessment of the end of treatment response. Adding PET to CT response criteria improved the accuracy of measurement of treatment response after chemotherapy, but earlier assessment of response is needed during the course of therapy to improve patient outcome, she explained. “After only one to two cycles of chemotherapy, interim PET can accurately predict response by monitoring the reduction in FDG [fluorodeoxyglucose] uptake, even before there is a change in tumor size,” said Dr. Barrington, who made her point by presenting the five-point scale (5-PS), also called the Deauville criteria, which has been used in trials to score response on early PET scans.
Related Links:
German Cancer Research Center
“MRI gives us more information and is probably the most important imaging technique in assessing disease activity in myeloma,” said Dr. Jens Hillengass, a physician scientist from the German Cancer Research Center (Heidelberg, Germany) who presented his findings on March 9, 2013, during the State of the Art symposium at the European Congress of Radiology (ECR), held in Vienna (Austria).
Current guidelines for the evaluation of therapy response are chiefly based on serologic markers and reference imaging to track large soft-tissue tumors. However, Dr. Hillengass thinks that imaging, and in particular MRI and PET, should be included in the recommendations, at least in some patients. For instance, many myeloma patients show changes on MRI that are not visible on a skeletal survey. MRI helps to differentiate between bone and bone marrow; it also has higher sensitivity for imaging of bone marrow effects in total, and demonstrates the first infiltration of plasma cells before overstimulation of osteoclasts and the resulting bone destruction.
Recent research indicates that some patients show diffuse infiltration of bone marrow with malignant plasma cells while others show focal infiltration. Several studies have looked at the prognostic significance of findings from MRI and PET, and suggest that a higher number of focal lesions are associated with a worse prognosis, Dr. Hillengass explained. His research group found that if focal lesions in bone marrow disappear upon MRI, then the patient outcome is better than if remission is defined according to serological markers. Being able to show that lesions are still there could help indicate relapse, which is the case for most patients.
If additional indications suggest that MRI can be used to evaluate disease activity and the extent of bone marrow infiltration with plasma cells prior to bone destruction, there might be a stronger case for earlier treatment, before bone destruction has started, Dr. Hillengass believes. “There are good data to say that if lesions persist, then treatment should continue; these data are on high-risk disease based on cytogenetics, and suggest treating patients for a long time is beneficial,” he said.
Interim PET could be used to monitor response-adapted therapy in Hodgkin lymphoma and aggressive non-Hodgkin lymphoma, according to Dr. Sally Barrington, a consultant physician in nuclear medicine at London’s St. Thomas’ PET Imaging Center (UK), who also spoke during the symposium.
PET was added to new response criteria for lymphoma in 2007 for assessment of the end of treatment response. Adding PET to CT response criteria improved the accuracy of measurement of treatment response after chemotherapy, but earlier assessment of response is needed during the course of therapy to improve patient outcome, she explained. “After only one to two cycles of chemotherapy, interim PET can accurately predict response by monitoring the reduction in FDG [fluorodeoxyglucose] uptake, even before there is a change in tumor size,” said Dr. Barrington, who made her point by presenting the five-point scale (5-PS), also called the Deauville criteria, which has been used in trials to score response on early PET scans.
Related Links:
German Cancer Research Center
Latest MRI News
- Novel Imaging Approach to Improve Treatment for Spinal Cord Injuries
- AI-Assisted Model Enhances MRI Heart Scans
- AI Model Outperforms Doctors at Identifying Patients Most At-Risk of Cardiac Arrest
- New MRI Technique Reveals Hidden Heart Issues
- Shorter MRI Exam Effectively Detects Cancer in Dense Breasts
- MRI to Replace Painful Spinal Tap for Faster MS Diagnosis
- MRI Scans Can Identify Cardiovascular Disease Ten Years in Advance
- Simple Brain Scan Diagnoses Parkinson's Disease Years Before It Becomes Untreatable
- Cutting-Edge MRI Technology to Revolutionize Diagnosis of Common Heart Problem
- New MRI Technique Reveals True Heart Age to Prevent Attacks and Strokes
- AI Tool Predicts Relapse of Pediatric Brain Cancer from Brain MRI Scans
- AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
- Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
- AI-Powered MRI Technology Improves Parkinson’s Diagnoses
- Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
- First-Of-Its-Kind AI-Driven Brain Imaging Platform to Better Guide Stroke Treatment Options
Channels
Radiography
view channel
X-Ray Breakthrough Captures Three Image-Contrast Types in Single Shot
Detecting early-stage cancer or subtle changes deep inside tissues has long challenged conventional X-ray systems, which rely only on how structures absorb radiation. This limitation keeps many microstructural... Read more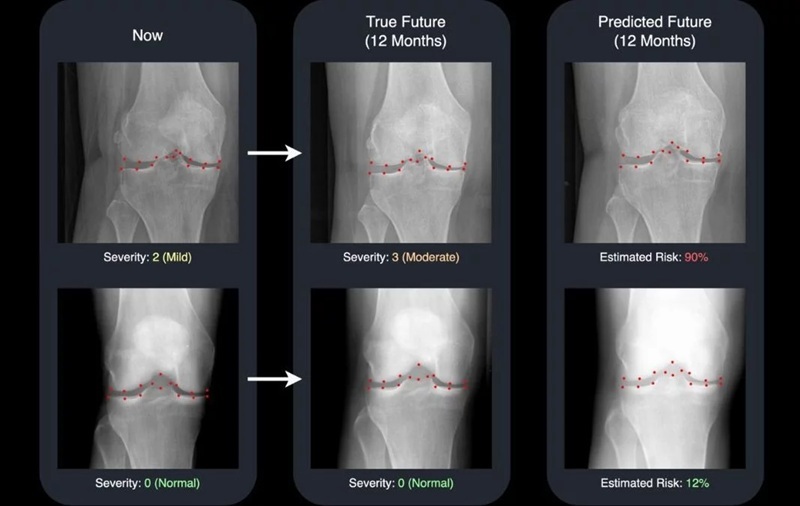
AI Generates Future Knee X-Rays to Predict Osteoarthritis Progression Risk
Osteoarthritis, a degenerative joint disease affecting over 500 million people worldwide, is the leading cause of disability among older adults. Current diagnostic tools allow doctors to assess damage... Read moreUltrasound
view channel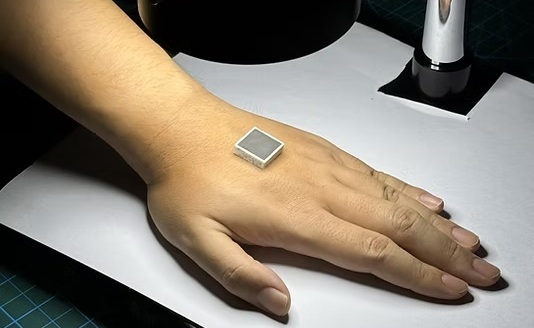
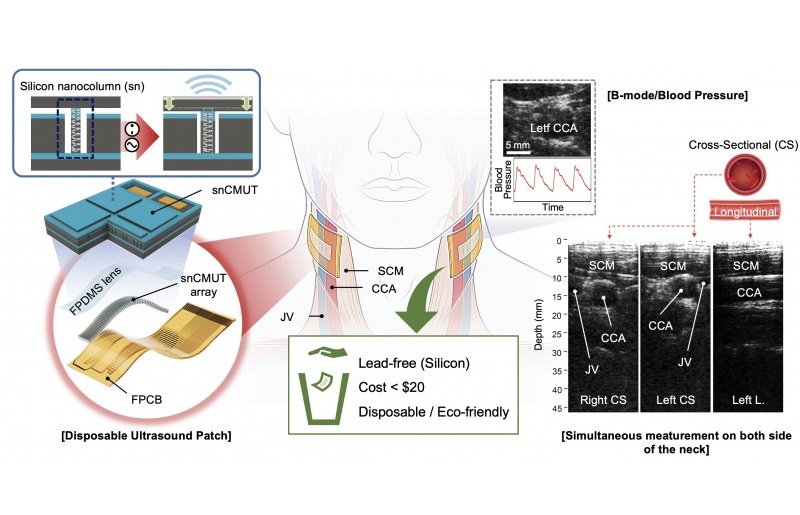
Wearable Ultrasound Imaging System to Enable Real-Time Disease Monitoring
Chronic conditions such as hypertension and heart failure require close monitoring, yet today’s ultrasound imaging is largely confined to hospitals and short, episodic scans. This reactive model limits... Read more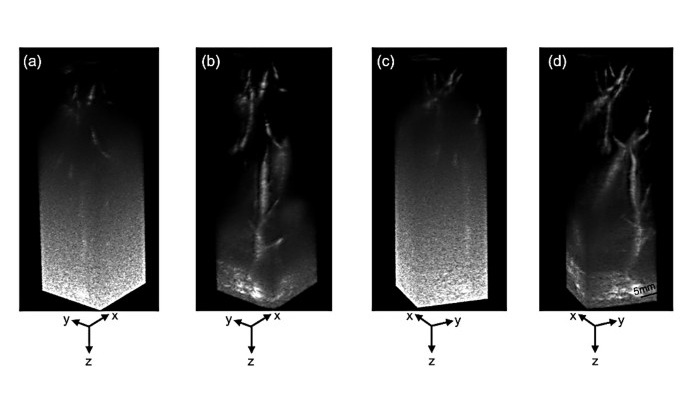
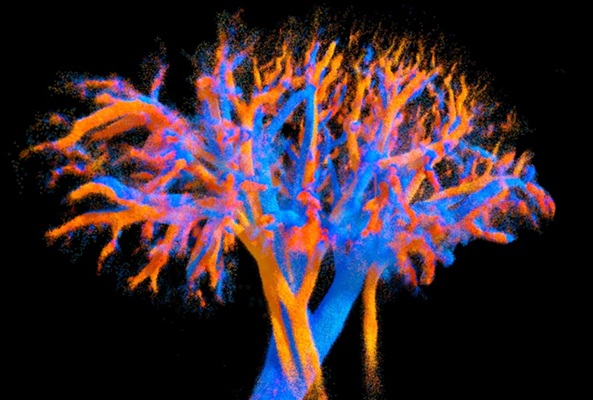
Ultrasound Technique Visualizes Deep Blood Vessels in 3D Without Contrast Agents
Producing clear 3D images of deep blood vessels has long been difficult without relying on contrast agents, CT scans, or MRI. Standard ultrasound typically provides only 2D cross-sections, limiting clinicians’... Read moreNuclear Medicine
view channel
PET Imaging of Inflammation Predicts Recovery and Guides Therapy After Heart Attack
Acute myocardial infarction can trigger lasting heart damage, yet clinicians still lack reliable tools to identify which patients will regain function and which may develop heart failure.... Read more
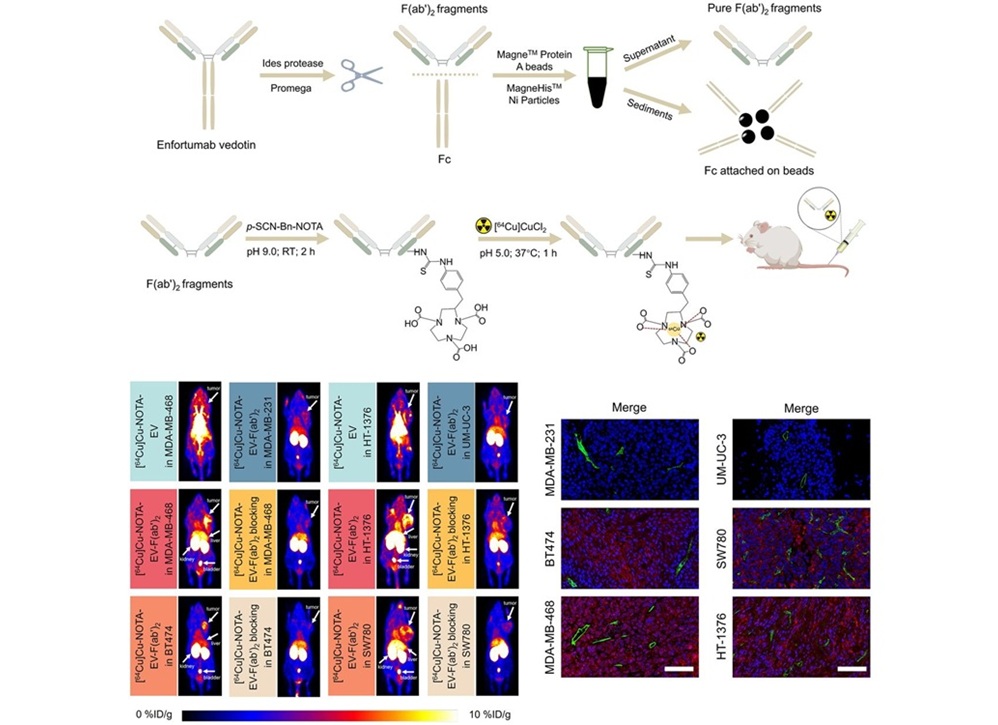
Radiotheranostic Approach Detects, Kills and Reprograms Aggressive Cancers
Aggressive cancers such as osteosarcoma and glioblastoma often resist standard therapies, thrive in hostile tumor environments, and recur despite surgery, radiation, or chemotherapy. These tumors also... Read more
New Imaging Solution Improves Survival for Patients with Recurring Prostate Cancer
Detecting recurrent prostate cancer remains one of the most difficult challenges in oncology, as standard imaging methods such as bone scans and CT scans often fail to accurately locate small or early-stage tumors.... Read moreGeneral/Advanced Imaging
view channel
3D Scanning Approach Enables Ultra-Precise Brain Surgery
Precise navigation is critical in neurosurgery, yet even small alignment errors can affect outcomes when operating deep within the brain. A new 3D surface-scanning approach now provides a radiation-free... Read more
AI Tool Improves Medical Imaging Process by 90%
Accurately labeling different regions within medical scans, a process known as medical image segmentation, is critical for diagnosis, surgery planning, and research. Traditionally, this has been a manual... Read more
New Ultrasmall, Light-Sensitive Nanoparticles Could Serve as Contrast Agents
Medical imaging technologies face ongoing challenges in capturing accurate, detailed views of internal processes, especially in conditions like cancer, where tracking disease development and treatment... Read more
AI Algorithm Accurately Predicts Pancreatic Cancer Metastasis Using Routine CT Images
In pancreatic cancer, detecting whether the disease has spread to other organs is critical for determining whether surgery is appropriate. If metastasis is present, surgery is not recommended, yet current... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more