First Adaptive Radiotherapy Trial Initiated for Head and Neck Cancer Patients
|
By MedImaging International staff writers Posted on 28 Feb 2012 |
Researchers have released initial findings from a first-of-its-kind clinical trial in adaptive radiotherapy (ART) for head and neck cancer. The trial, sponsored by the US National Cancer Institute (Bethesda, MD, USA), provides indications that ART may benefit patients with less technical problems than previously believed.
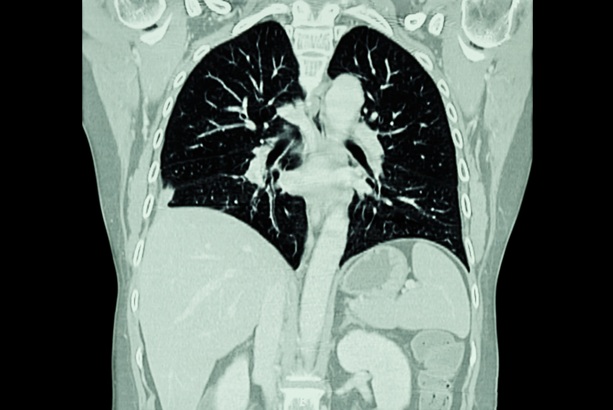
The findings of this trial were released online February 2012 in advance of publication in the International Journal of Radiation Oncology Biology Physics. Physicians commonly use radiotherapy to treat squamous cell carcinoma of the oropharynx. Current standard-of-care treatment is called intensity-modulated radiotherapy (IMRT). IMRT allows clinicians to “sculpt” radiation to fit the anatomy of individual patients. Although attractive, this technique has a major problem--it is based entirely on a computed (CT) or magnetic resonance imaging (MRI) scan taken before actual treatment begins. Because a typical course of radiation treatment for oropharynx cancer lasts six to seven weeks, standard IMRT cannot compensate for typical changes that take place in a patient’s body during this time, such as weight loss, shrinkage of tumor, or gradual movement of normal tissues. Recent work suggests that the inability of standard IMRT to keep up with these changes might lead to unanticipated toxicity, or potentially worse, missing of tumor.
For this new trial, which was conducted at the University of Texas M.D. Anderson Cancer Center (Houston, TX, USA), investigators began patients on standard IMRT. They then took CT scans while patients were lying in the radiation treatment room each day so they could track changes in tumor and normal tissues during the entire course of treatment. Through computerized techniques, the investigators adapted treatment if they noticed significant tumor or body changes that could affect quality of treatment. Most interestingly, the researchers found that most patients required only one or at most two adaptions of IMRT to maintain treatment quality.
“This is the first prospective clinical trial of its kind to gauge how ‘refitting’ of IMRT to a patient’s body actually impacts care for a patient who has head and neck cancer,” noted David Schwartz, MD, vice-chair of radiation medicine at the North Shore- Long Island Jewish (LIJ) Health System, associate professor at the Hofstra-North Shore Long Island Jewish LIJ School of Medicine (Hempstead, NY, USA), and a senior investigator at The Feinstein Institute for Medical Research (Manhasset, NY, USA).
“What most encouraged us was that ART appears effective with only one or two additional replans. This means that ART does not have to be overly burdensome or expensive to make a difference. This is something that is feasible, and could eventually make a real-world difference in many clinics. ART keeps radiation treatment tightly fitted to a patient’s body, almost as if it were being shrink-wrapped. It is as individualized as our current treatment can realistically be.”
Twenty-four patients enrolled onto this institutional review board approved trial; data for 22 of these patients were analyzed with at least 12 months follow-up. Treatment was initiated with a baseline IMRT plan, and computed tomography (CT) imaging was performed in the treatment room each day to map tumors and normal anatomy to assess need for ART replanning.
Primary site was base of tongue in 15 patients, tonsil in six patients, and glossopharyngeal sulcus in one patient. Twenty patients (9%) had American Joint Committee on Cancer (AJCC) stage IV disease. T stage distribution was two T1, 12 T2, three T3, and five T4. N stage distribution was one N0, two N1, five N2a, 12 N2b, and two N2c. Of the patients, 21 (95%) received systemic therapy.
All patients required at least one ART replan because of tumor and normal tissue changes; eight patients (36%) required a second ART replan. For the patients who required one adaptive replan, parotid salivary glands had shrunk by an average of 16% and tumors had shrunk by 5% by the time of the replan. For the patients who required a second adaptive replan, parotid glands and tumors had shrunk by 24% and 14%, respectively. Most ART replans were completed within one day.
With a 31-month median follow-up, there has been no primary site failure and one nodal relapse, yielding 100% local and 95% regional disease control at two years. Chronic toxicity and functional outcomes beyond one year remain favorable relative to published results for standard IMRT.
Related Links:
University of Texas M.D. Anderson Cancer Center
Hofstra-North Shore Long Island Jewish School of Medicine
Feinstein Institute for Medical Research
The findings of this trial were released online February 2012 in advance of publication in the International Journal of Radiation Oncology Biology Physics. Physicians commonly use radiotherapy to treat squamous cell carcinoma of the oropharynx. Current standard-of-care treatment is called intensity-modulated radiotherapy (IMRT). IMRT allows clinicians to “sculpt” radiation to fit the anatomy of individual patients. Although attractive, this technique has a major problem--it is based entirely on a computed (CT) or magnetic resonance imaging (MRI) scan taken before actual treatment begins. Because a typical course of radiation treatment for oropharynx cancer lasts six to seven weeks, standard IMRT cannot compensate for typical changes that take place in a patient’s body during this time, such as weight loss, shrinkage of tumor, or gradual movement of normal tissues. Recent work suggests that the inability of standard IMRT to keep up with these changes might lead to unanticipated toxicity, or potentially worse, missing of tumor.
For this new trial, which was conducted at the University of Texas M.D. Anderson Cancer Center (Houston, TX, USA), investigators began patients on standard IMRT. They then took CT scans while patients were lying in the radiation treatment room each day so they could track changes in tumor and normal tissues during the entire course of treatment. Through computerized techniques, the investigators adapted treatment if they noticed significant tumor or body changes that could affect quality of treatment. Most interestingly, the researchers found that most patients required only one or at most two adaptions of IMRT to maintain treatment quality.
“This is the first prospective clinical trial of its kind to gauge how ‘refitting’ of IMRT to a patient’s body actually impacts care for a patient who has head and neck cancer,” noted David Schwartz, MD, vice-chair of radiation medicine at the North Shore- Long Island Jewish (LIJ) Health System, associate professor at the Hofstra-North Shore Long Island Jewish LIJ School of Medicine (Hempstead, NY, USA), and a senior investigator at The Feinstein Institute for Medical Research (Manhasset, NY, USA).
“What most encouraged us was that ART appears effective with only one or two additional replans. This means that ART does not have to be overly burdensome or expensive to make a difference. This is something that is feasible, and could eventually make a real-world difference in many clinics. ART keeps radiation treatment tightly fitted to a patient’s body, almost as if it were being shrink-wrapped. It is as individualized as our current treatment can realistically be.”
Twenty-four patients enrolled onto this institutional review board approved trial; data for 22 of these patients were analyzed with at least 12 months follow-up. Treatment was initiated with a baseline IMRT plan, and computed tomography (CT) imaging was performed in the treatment room each day to map tumors and normal anatomy to assess need for ART replanning.
Primary site was base of tongue in 15 patients, tonsil in six patients, and glossopharyngeal sulcus in one patient. Twenty patients (9%) had American Joint Committee on Cancer (AJCC) stage IV disease. T stage distribution was two T1, 12 T2, three T3, and five T4. N stage distribution was one N0, two N1, five N2a, 12 N2b, and two N2c. Of the patients, 21 (95%) received systemic therapy.
All patients required at least one ART replan because of tumor and normal tissue changes; eight patients (36%) required a second ART replan. For the patients who required one adaptive replan, parotid salivary glands had shrunk by an average of 16% and tumors had shrunk by 5% by the time of the replan. For the patients who required a second adaptive replan, parotid glands and tumors had shrunk by 24% and 14%, respectively. Most ART replans were completed within one day.
With a 31-month median follow-up, there has been no primary site failure and one nodal relapse, yielding 100% local and 95% regional disease control at two years. Chronic toxicity and functional outcomes beyond one year remain favorable relative to published results for standard IMRT.
Related Links:
University of Texas M.D. Anderson Cancer Center
Hofstra-North Shore Long Island Jewish School of Medicine
Feinstein Institute for Medical Research
Latest Nuclear Medicine News
- Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
- Combining Advanced Imaging Technologies Offers Breakthrough in Glioblastoma Treatment
- New Molecular Imaging Agent Accurately Identifies Crucial Cancer Biomarker
- New Scans Light Up Aggressive Tumors for Better Treatment
- AI Stroke Brain Scan Readings Twice as Accurate as Current Method
- AI Analysis of PET/CT Images Predicts Side Effects of Immunotherapy in Lung Cancer
- New Imaging Agent to Drive Step-Change for Brain Cancer Imaging
- Portable PET Scanner to Detect Earliest Stages of Alzheimer’s Disease
Channels
MRI
view channel
Cutting-Edge MRI Technology to Revolutionize Diagnosis of Common Heart Problem
Aortic stenosis is a common and potentially life-threatening heart condition. It occurs when the aortic valve, which regulates blood flow from the heart to the rest of the body, becomes stiff and narrow.... Read more
New MRI Technique Reveals True Heart Age to Prevent Attacks and Strokes
Heart disease remains one of the leading causes of death worldwide. Individuals with conditions such as diabetes or obesity often experience accelerated aging of their hearts, sometimes by decades.... Read more
AI Tool Predicts Relapse of Pediatric Brain Cancer from Brain MRI Scans
Many pediatric gliomas are treatable with surgery alone, but relapses can be catastrophic. Predicting which patients are at risk for recurrence remains challenging, leading to frequent follow-ups with... Read more
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read moreUltrasound
view channel.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read more
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read moreNuclear Medicine
view channel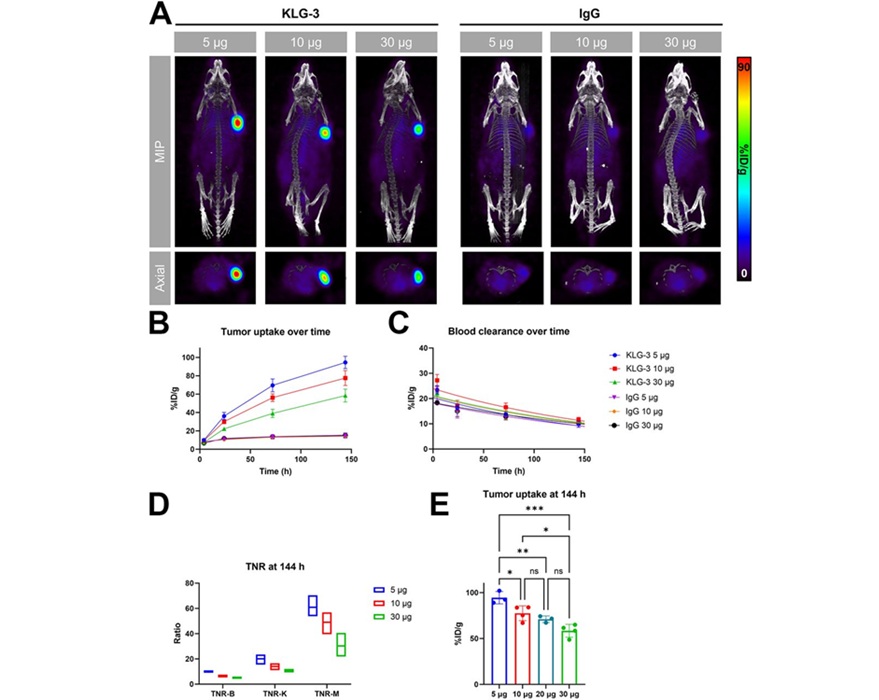
Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
Interleukin-13 receptor α-2 (IL13Rα2) is a cell surface receptor commonly found in solid tumors such as glioblastoma, melanoma, and breast cancer. It is minimally expressed in normal tissues, making it... Read more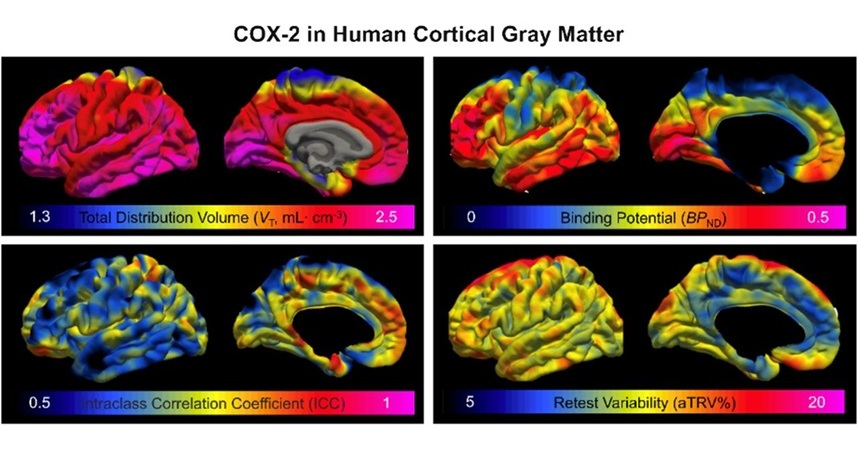
Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
COX-2, an enzyme that plays a key role in brain inflammation, can be significantly upregulated by inflammatory stimuli and neuroexcitation. Researchers suggest that COX-2 density in the brain could serve... Read moreGeneral/Advanced Imaging
view channel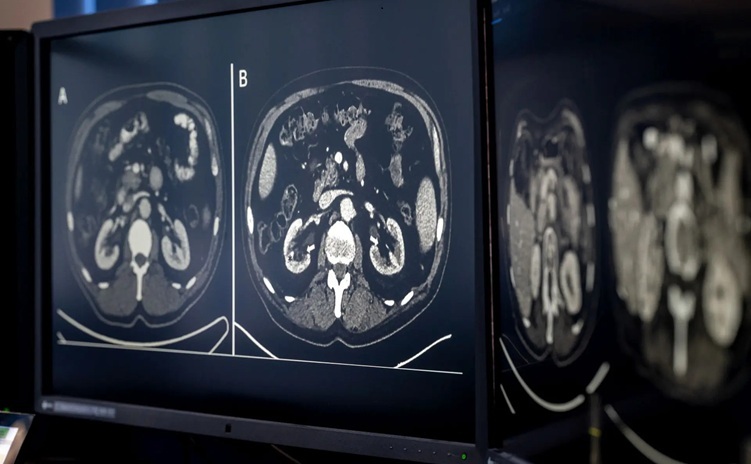
AI-Based CT Scan Analysis Predicts Early-Stage Kidney Damage Due to Cancer Treatments
Radioligand therapy, a form of targeted nuclear medicine, has recently gained attention for its potential in treating specific types of tumors. However, one of the potential side effects of this therapy... Read more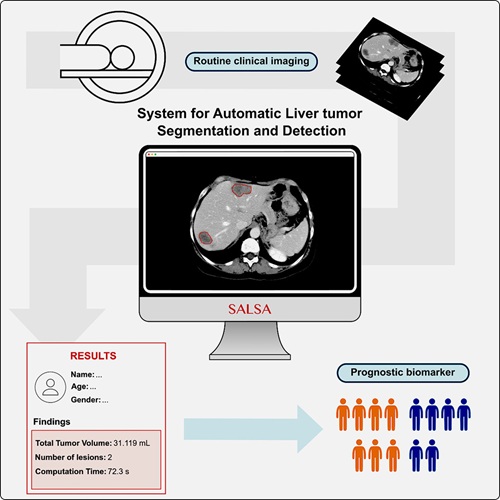
CT-Based Deep Learning-Driven Tool to Enhance Liver Cancer Diagnosis
Medical imaging, such as computed tomography (CT) scans, plays a crucial role in oncology, offering essential data for cancer detection, treatment planning, and monitoring of response to therapies.... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more