Breast Cancer Brachytherapy Benefits Still Unclear
|
By MedImaging International staff writers Posted on 17 Jan 2012 |
Accelerated partial breast irradiation using brachytherapy (APBIb) for the treatment of breast cancer has been rapidly increasing over the last several years in the United States as an alternative to conventional whole-breast irradiation (WBI), according to recent research.
The study’s findings were published online December 16, 2011, in the Journal of the National Cancer Institute. Various types of APBI recurrence (external beam radiation, intraoperative radiotherapy, brachytherapy using multiple interstitial catheters, or intracavitary brachytherapy using a balloon catheter) deliver radiation to breast tissue at the highest risk of recurrence. Benefits of these techniques include decreased treatment time and less radiation to uninvolved portions of the breast and normal tissues.
Disadvantages of APBI include the potential that tumor cells in a different part of the breast will remain untreated, which could lead to increased local recurrence. Because of the potential limitations of APBI, in 2009 the American Society for Radiation Oncology (ASTRO; Fairfax, VA, USA) convened a task force of breast cancer experts to develop criteria for use of APBI off-protocol. They proposed three groups of APBI appropriateness: suitable, cautionary and unsuitable, based on patient characteristics and clinical factors.
Because of the growing popularity of APBIb specifically, Jona Hattangadi, MD, from the department of radiation oncology at the Brigham and Women’s Hospital and Harvard Medical School (both based in Boston, MA, USA) and colleagues performed a retrospective analysis of data from the Surveillance, Epidemiology, and End Results (SEER) database of women who had received either APBIb or WBI between 2000 and 2007. In line with ASTRO guidelines, the researchers classified the 138,815 women as “suitable,” “cautionary,” or “unsuitable” for APBIb.
The investigators revealed that 3,576 of the 138,815 patients had received APBIb: 32% of whom would have been considered suitable, 29.6% cautionary, and 36.2% unsuitable. The overall use of APBIb increased from 0.4% in 2000 to 6.6% in 2007. There was a broad range of utilization patterns across the United States with specific geographic regions having higher APBIb use in spite of other patient and clinical factors. There were also considerable racial and ethnic discrepancies with respect to APBIb use. White women were more apt to get this treatment than black women among cautionary or unsuitable patients; and women living in cities were more likely to get it than those in rural areas even though it would potentially provide greater convenience for the rural women.
The authors concluded that, “the wide disparity in use of APBIb suggests that unwarranted variation--practice variation not explained by illness, patient preference, or evidence-based medicine--may be present. Future studies of APBIb use will help elucidate whether patterns change as [the ASTRO guidelines] diffuse into practice and whether the regional and temporal changes in APBIb cost, reimbursement, and insurance coverage affect utilization.”
In an accompanying editorial in the same issue, Simona F. Shaitelman, MD, from the department of radiation oncology at the University of Texas M.D. Anderson Cancer Center (Houston, USA), noted that it is encouraging that the authors discovered the fastest increase in utilization among patients classified as suitable, even if most of patients undergoing APBIb in their study were not classified as suitable. Dr. Shaitelman also commented on the authors’ suggestion that financial interests that might be fueling usage and noted that reimbursement was decreased for the procedure after the end of the period of the study. She wrote, “Moving forward, it will be useful to analyze more recent trends in the use of APBI and to document whether such changes in financial remuneration are indeed associated with the delivery of APBI.”
Dr. Shaitelman concluded that more research of the effectiveness of APBI is needed. “Although population based studies allow us to reflect on changes in patterns of practice, we are still left eagerly awaiting the results of large randomized trials that compare patients outcomes with WBI vs APBI.”
Related Links:
Brigham and Women’s Hospital
M.D. Anderson Cancer Center
The study’s findings were published online December 16, 2011, in the Journal of the National Cancer Institute. Various types of APBI recurrence (external beam radiation, intraoperative radiotherapy, brachytherapy using multiple interstitial catheters, or intracavitary brachytherapy using a balloon catheter) deliver radiation to breast tissue at the highest risk of recurrence. Benefits of these techniques include decreased treatment time and less radiation to uninvolved portions of the breast and normal tissues.
Disadvantages of APBI include the potential that tumor cells in a different part of the breast will remain untreated, which could lead to increased local recurrence. Because of the potential limitations of APBI, in 2009 the American Society for Radiation Oncology (ASTRO; Fairfax, VA, USA) convened a task force of breast cancer experts to develop criteria for use of APBI off-protocol. They proposed three groups of APBI appropriateness: suitable, cautionary and unsuitable, based on patient characteristics and clinical factors.
Because of the growing popularity of APBIb specifically, Jona Hattangadi, MD, from the department of radiation oncology at the Brigham and Women’s Hospital and Harvard Medical School (both based in Boston, MA, USA) and colleagues performed a retrospective analysis of data from the Surveillance, Epidemiology, and End Results (SEER) database of women who had received either APBIb or WBI between 2000 and 2007. In line with ASTRO guidelines, the researchers classified the 138,815 women as “suitable,” “cautionary,” or “unsuitable” for APBIb.
The investigators revealed that 3,576 of the 138,815 patients had received APBIb: 32% of whom would have been considered suitable, 29.6% cautionary, and 36.2% unsuitable. The overall use of APBIb increased from 0.4% in 2000 to 6.6% in 2007. There was a broad range of utilization patterns across the United States with specific geographic regions having higher APBIb use in spite of other patient and clinical factors. There were also considerable racial and ethnic discrepancies with respect to APBIb use. White women were more apt to get this treatment than black women among cautionary or unsuitable patients; and women living in cities were more likely to get it than those in rural areas even though it would potentially provide greater convenience for the rural women.
The authors concluded that, “the wide disparity in use of APBIb suggests that unwarranted variation--practice variation not explained by illness, patient preference, or evidence-based medicine--may be present. Future studies of APBIb use will help elucidate whether patterns change as [the ASTRO guidelines] diffuse into practice and whether the regional and temporal changes in APBIb cost, reimbursement, and insurance coverage affect utilization.”
In an accompanying editorial in the same issue, Simona F. Shaitelman, MD, from the department of radiation oncology at the University of Texas M.D. Anderson Cancer Center (Houston, USA), noted that it is encouraging that the authors discovered the fastest increase in utilization among patients classified as suitable, even if most of patients undergoing APBIb in their study were not classified as suitable. Dr. Shaitelman also commented on the authors’ suggestion that financial interests that might be fueling usage and noted that reimbursement was decreased for the procedure after the end of the period of the study. She wrote, “Moving forward, it will be useful to analyze more recent trends in the use of APBI and to document whether such changes in financial remuneration are indeed associated with the delivery of APBI.”
Dr. Shaitelman concluded that more research of the effectiveness of APBI is needed. “Although population based studies allow us to reflect on changes in patterns of practice, we are still left eagerly awaiting the results of large randomized trials that compare patients outcomes with WBI vs APBI.”
Related Links:
Brigham and Women’s Hospital
M.D. Anderson Cancer Center
Latest Nuclear Medicine News
- Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
- Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
- Innovative PET Imaging Technique to Help Diagnose Neurodegeneration
- New Molecular Imaging Test to Improve Lung Cancer Diagnosis
- Novel PET Technique Visualizes Spinal Cord Injuries to Predict Recovery
- Next-Gen Tau Radiotracers Outperform FDA-Approved Imaging Agents in Detecting Alzheimer’s
- Breakthrough Method Detects Inflammation in Body Using PET Imaging
- Advanced Imaging Reveals Hidden Metastases in High-Risk Prostate Cancer Patients
- Combining Advanced Imaging Technologies Offers Breakthrough in Glioblastoma Treatment
- New Molecular Imaging Agent Accurately Identifies Crucial Cancer Biomarker
- New Scans Light Up Aggressive Tumors for Better Treatment
- AI Stroke Brain Scan Readings Twice as Accurate as Current Method
- AI Analysis of PET/CT Images Predicts Side Effects of Immunotherapy in Lung Cancer
- New Imaging Agent to Drive Step-Change for Brain Cancer Imaging
- Portable PET Scanner to Detect Earliest Stages of Alzheimer’s Disease
- New Immuno-PET Imaging Technique Identifies Glioblastoma Patients Who Would Benefit from Immunotherapy
Channels
Radiography
view channel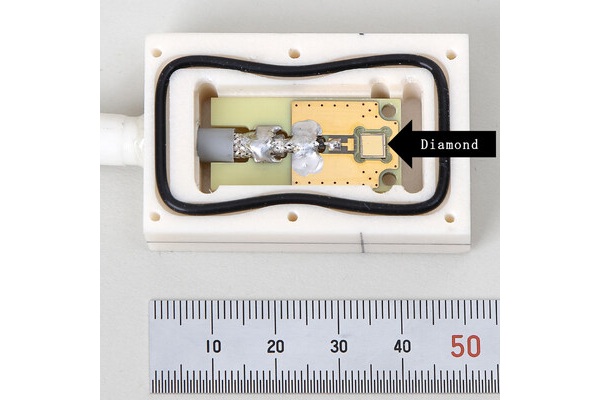
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read more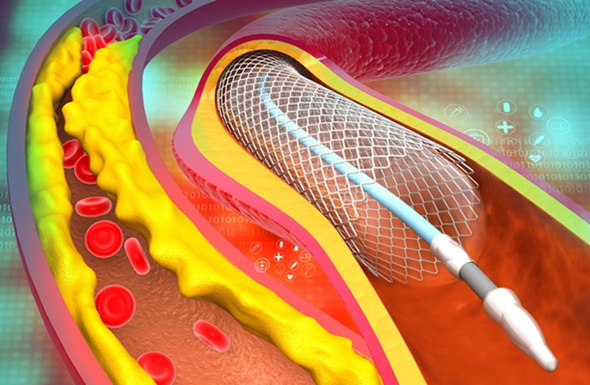
AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure where small metal tubes called stents are inserted into partially blocked coronary arteries... Read moreMRI
view channel
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read more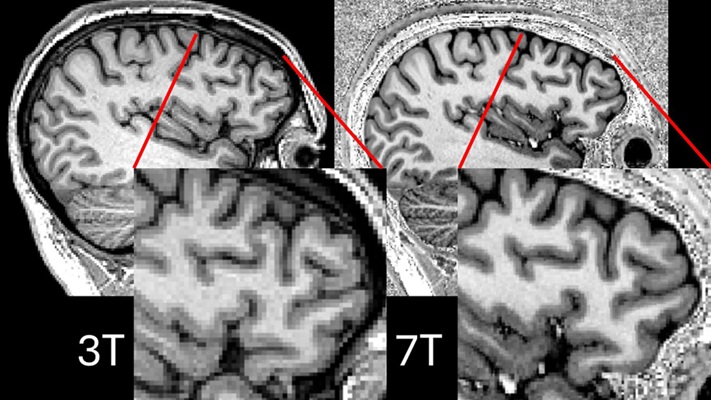
Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
Approximately 360,000 individuals in the UK suffer from focal epilepsy, a condition in which seizures spread from one part of the brain. Around a third of these patients experience persistent seizures... Read more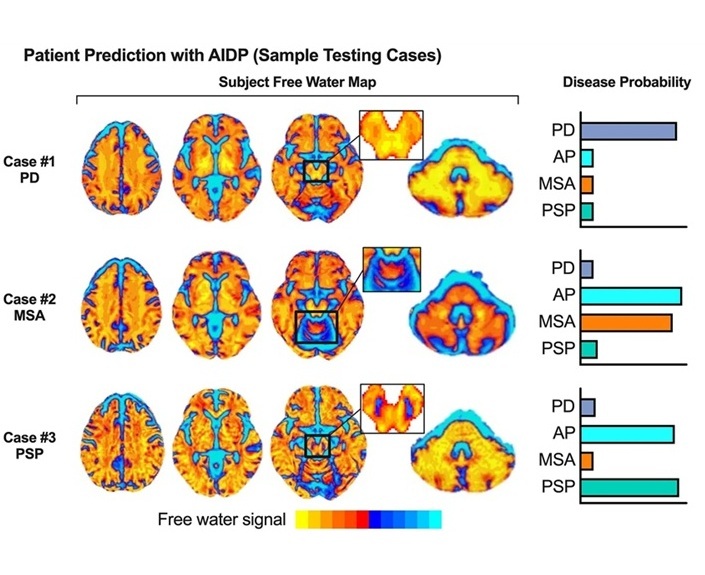
AI-Powered MRI Technology Improves Parkinson’s Diagnoses
Current research shows that the accuracy of diagnosing Parkinson’s disease typically ranges from 55% to 78% within the first five years of assessment. This is partly due to the similarities shared by Parkinson’s... Read more
Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
Artificial intelligence (AI) technologies are transforming the way medical images are analyzed, offering unprecedented capabilities in quantitatively extracting features that go beyond traditional visual... Read moreUltrasound
view channel
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read more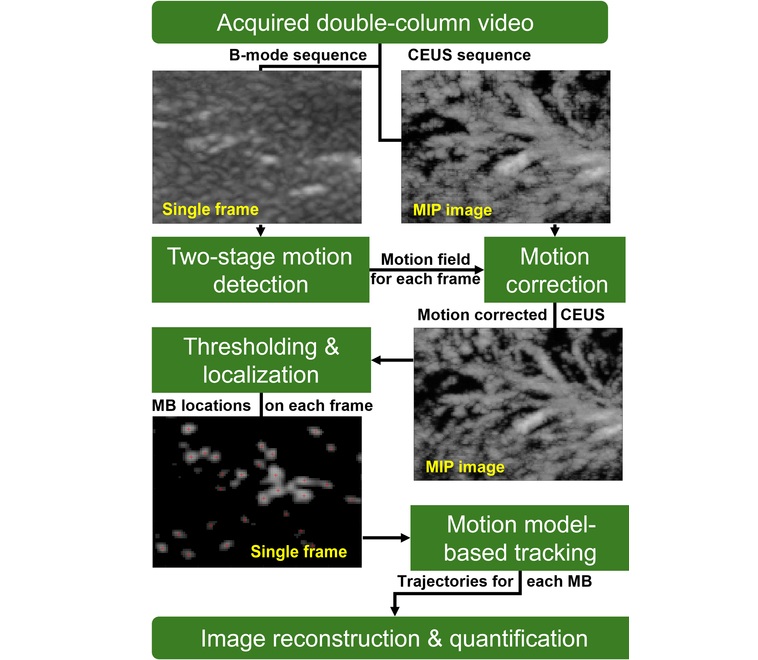
Novel Imaging Method Enables Early Diagnosis and Treatment Monitoring of Type 2 Diabetes
Type 2 diabetes is recognized as an autoimmune inflammatory disease, where chronic inflammation leads to alterations in pancreatic islet microvasculature, a key factor in β-cell dysfunction.... Read moreGeneral/Advanced Imaging
view channel
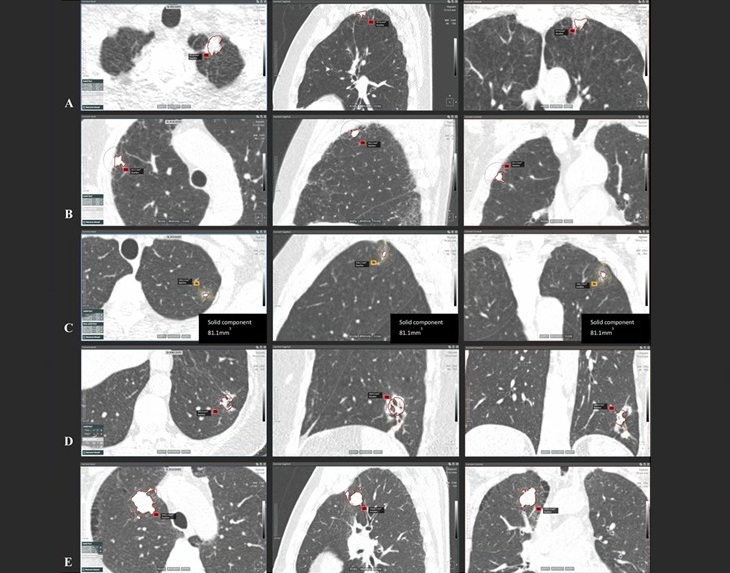
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read more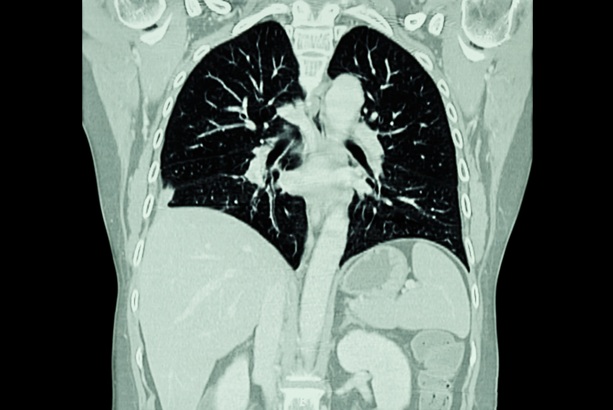
AI Model Significantly Enhances Low-Dose CT Capabilities
Lung cancer remains one of the most challenging diseases, making early diagnosis vital for effective treatment. Fortunately, advancements in artificial intelligence (AI) are revolutionizing lung cancer... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more