Popular Mammography Tool Not Effective for Finding Invasive Breast Cancer
|
By MedImaging International staff writers Posted on 15 Aug 2011 |
Computer-aided detection (CAD) technology was shown to be ineffective in identifying breast tumors, and appears to increase a woman’s risk of being called back needlessly for further testing following mammography, a recent study has found.
The analysis of 1.6 million mammograms in seven states in the United States has delivered the most definitive findings to date on whether the popular mammography tool is effective in helping find breast cancer. “In real-world practice, CAD increases the chances of being unnecessarily called back for further testing because of false-positive results without clear benefits to women,” said Dr. Joshua Fenton, assistant professor in the University of California (UC) Davis (USA) department of family and community medicine. “Breast cancers were detected at a similar stage and size regardless of whether or not radiologists used CAD.”
The study examined screening mammograms performed on more than 680,000 women at 90 mammography facilities in seven US states, from 1998 to 2006. The false-positive rate normally increased from 8.1% before CAD to 8.6% after CAD was installed at the facilities in the study. Moreover, the detection rate of breast cancer and the stage and size of breast cancer tumors were similar regardless of CAD.
The study, was published online July 28, 2011, in the Journal of the National Cancer Institute and used data from the Breast Cancer Surveillance Consortium. Computer-aided detection software, approved by the US Food and Drug Administration (FDA) in 1998, analyzes the mammogram image and marks suspicious areas for radiologists to review. Its use has surged in recent years since Medicare began covering it in 2001. CAD is now applied to the large majority of screening mammograms in the United States with annual direct US Medicare costs exceeding US$30 million, according to a 2010 study in the Journal of the American College of Radiology.
According to 2009 Medicare data, insurers including Medicare typically paid approximately $12 per screening mammogram for CAD in addition to the costs of the mammogram (about $81 for film mammography and $130 for digital mammography), representing a 9% to 15% additional cost for CAD use.
The current study builds on Dr. Fenton’s initial assessment of the technology published in the New England Journal of Medicine (NEJM) in 2007. That report, which examined mammography-screening results in 43 facilities, including seven that utilized CAD, found that CAD was associated with reduced accuracy of interpretation of screening mammograms but no difference in the detection rate of invasive breast cancer.
Critics of the research findings in the NEJM said the study was based on use of an older kind of CAD technology, and so did not accurately reflect its usefulness. “In the current study, we evaluated newer technology in a larger sample and over a longer time period,” said Dr. Fenton. “We also looked for the first time at cancer stage and cancer size, which are critical for understanding how CAD may affect long-term breast cancer outcomes, such as mortality.”
The authors wrote that the results of real-world studies of CAD might differ from findings from preclinical studies. They suggest that these differences may arise because radiologists in clinical practice do not always adhere as strictly to use of the technology as designed, as have radiologists in protocol-driven studies.
Related Links:
University of California Davis
The analysis of 1.6 million mammograms in seven states in the United States has delivered the most definitive findings to date on whether the popular mammography tool is effective in helping find breast cancer. “In real-world practice, CAD increases the chances of being unnecessarily called back for further testing because of false-positive results without clear benefits to women,” said Dr. Joshua Fenton, assistant professor in the University of California (UC) Davis (USA) department of family and community medicine. “Breast cancers were detected at a similar stage and size regardless of whether or not radiologists used CAD.”
The study examined screening mammograms performed on more than 680,000 women at 90 mammography facilities in seven US states, from 1998 to 2006. The false-positive rate normally increased from 8.1% before CAD to 8.6% after CAD was installed at the facilities in the study. Moreover, the detection rate of breast cancer and the stage and size of breast cancer tumors were similar regardless of CAD.
The study, was published online July 28, 2011, in the Journal of the National Cancer Institute and used data from the Breast Cancer Surveillance Consortium. Computer-aided detection software, approved by the US Food and Drug Administration (FDA) in 1998, analyzes the mammogram image and marks suspicious areas for radiologists to review. Its use has surged in recent years since Medicare began covering it in 2001. CAD is now applied to the large majority of screening mammograms in the United States with annual direct US Medicare costs exceeding US$30 million, according to a 2010 study in the Journal of the American College of Radiology.
According to 2009 Medicare data, insurers including Medicare typically paid approximately $12 per screening mammogram for CAD in addition to the costs of the mammogram (about $81 for film mammography and $130 for digital mammography), representing a 9% to 15% additional cost for CAD use.
The current study builds on Dr. Fenton’s initial assessment of the technology published in the New England Journal of Medicine (NEJM) in 2007. That report, which examined mammography-screening results in 43 facilities, including seven that utilized CAD, found that CAD was associated with reduced accuracy of interpretation of screening mammograms but no difference in the detection rate of invasive breast cancer.
Critics of the research findings in the NEJM said the study was based on use of an older kind of CAD technology, and so did not accurately reflect its usefulness. “In the current study, we evaluated newer technology in a larger sample and over a longer time period,” said Dr. Fenton. “We also looked for the first time at cancer stage and cancer size, which are critical for understanding how CAD may affect long-term breast cancer outcomes, such as mortality.”
The authors wrote that the results of real-world studies of CAD might differ from findings from preclinical studies. They suggest that these differences may arise because radiologists in clinical practice do not always adhere as strictly to use of the technology as designed, as have radiologists in protocol-driven studies.
Related Links:
University of California Davis
Latest Radiography News
- World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
- AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
- Higher Chest X-Ray Usage Catches Lung Cancer Earlier and Improves Survival
- AI-Powered Mammograms Predict Cardiovascular Risk
- Generative AI Model Significantly Reduces Chest X-Ray Reading Time
- AI-Powered Mammography Screening Boosts Cancer Detection in Single-Reader Settings
- Photon Counting Detectors Promise Fast Color X-Ray Images
- AI Can Flag Mammograms for Supplemental MRI
- 3D CT Imaging from Single X-Ray Projection Reduces Radiation Exposure
- AI Method Accurately Predicts Breast Cancer Risk by Analyzing Multiple Mammograms
- Printable Organic X-Ray Sensors Could Transform Treatment for Cancer Patients
- Highly Sensitive, Foldable Detector to Make X-Rays Safer
- Novel Breast Cancer Screening Technology Could Offer Superior Alternative to Mammogram
- Artificial Intelligence Accurately Predicts Breast Cancer Years Before Diagnosis
- AI-Powered Chest X-Ray Detects Pulmonary Nodules Three Years Before Lung Cancer Symptoms
- AI Model Identifies Vertebral Compression Fractures in Chest Radiographs
Channels
MRI
view channel
AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
Multiple sclerosis (MS) is a condition in which the immune system attacks the brain and spinal cord, leading to impairments in movement, sensation, and cognition. Magnetic Resonance Imaging (MRI) markers... Read more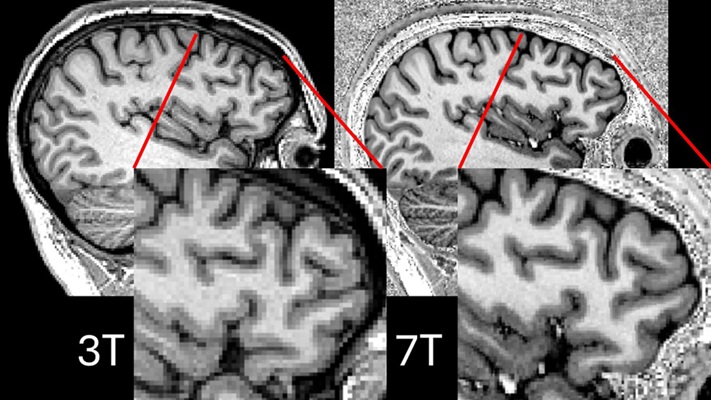
Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
Approximately 360,000 individuals in the UK suffer from focal epilepsy, a condition in which seizures spread from one part of the brain. Around a third of these patients experience persistent seizures... Read more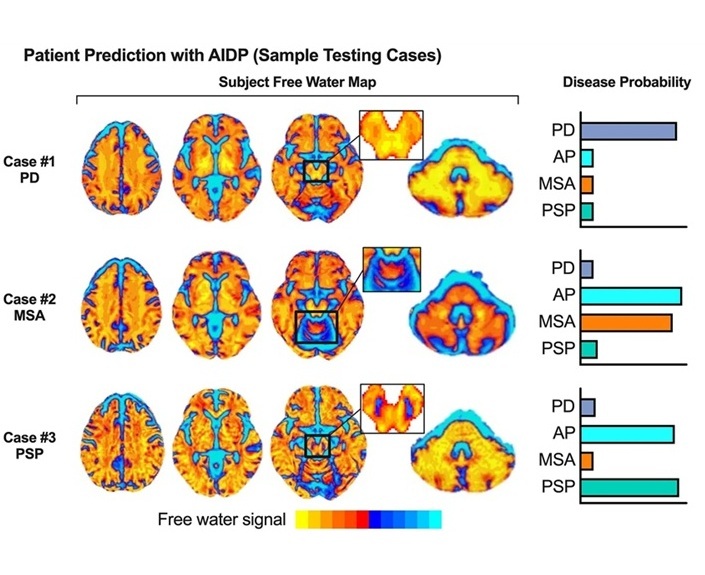
AI-Powered MRI Technology Improves Parkinson’s Diagnoses
Current research shows that the accuracy of diagnosing Parkinson’s disease typically ranges from 55% to 78% within the first five years of assessment. This is partly due to the similarities shared by Parkinson’s... Read more
Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
Artificial intelligence (AI) technologies are transforming the way medical images are analyzed, offering unprecedented capabilities in quantitatively extracting features that go beyond traditional visual... Read moreUltrasound
view channel.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read more
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read moreNuclear Medicine
view channel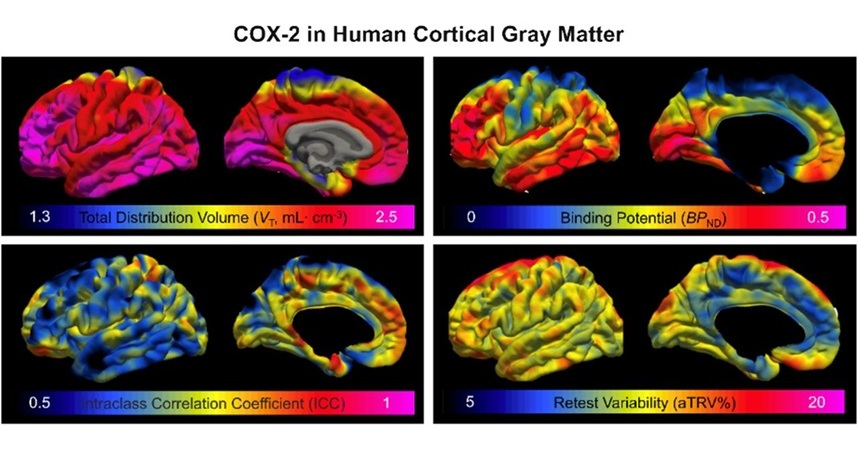
Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
COX-2, an enzyme that plays a key role in brain inflammation, can be significantly upregulated by inflammatory stimuli and neuroexcitation. Researchers suggest that COX-2 density in the brain could serve... Read more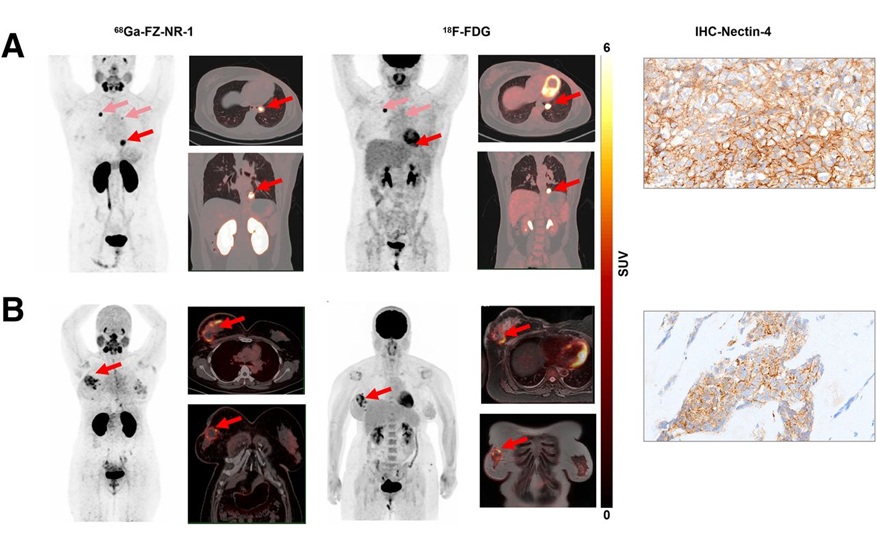
Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC), which represents 15-20% of all breast cancer cases, is one of the most aggressive subtypes, with a five-year survival rate of about 40%. Due to its significant heterogeneity... Read moreGeneral/Advanced Imaging
view channel
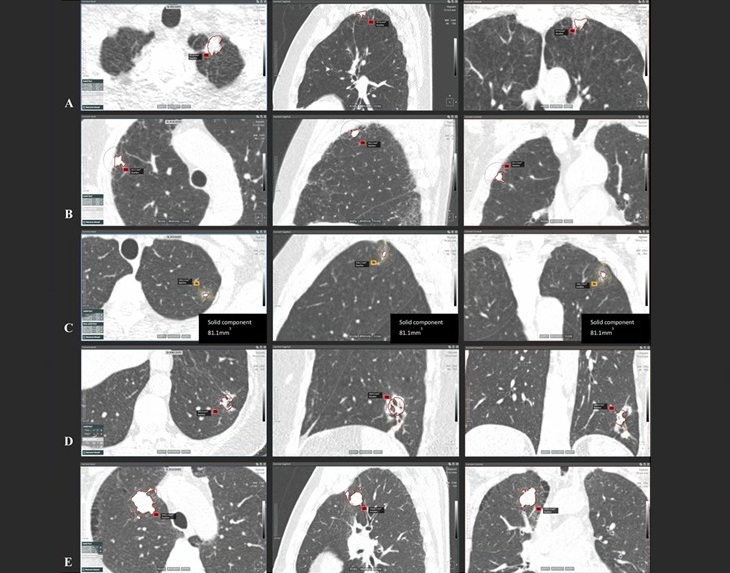
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read more
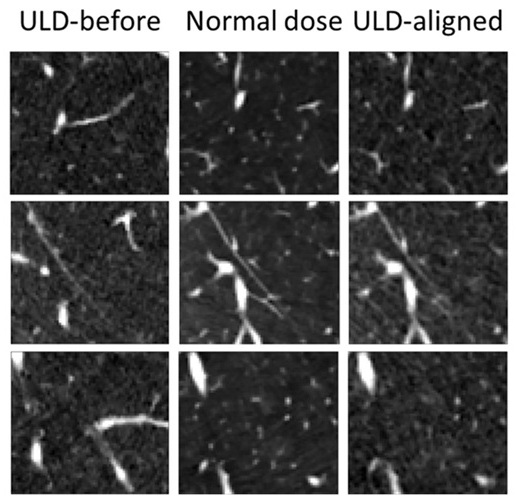
AI Model Significantly Enhances Low-Dose CT Capabilities
Lung cancer remains one of the most challenging diseases, making early diagnosis vital for effective treatment. Fortunately, advancements in artificial intelligence (AI) are revolutionizing lung cancer... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more