MRI Blood Flow Simulation Helps Plan Pediatric Heart Surgery
|
By MedImaging International staff writers Posted on 04 Sep 2009 |
Researchers collaborating with pediatric cardiologists and surgeons from two U.S. medical institutions have developed a tool for virtual surgery that allows heart surgeons to view the predicted effects of different surgical approaches.
By manipulating three-dimensional (3D) cardiac magnetic resonance images (MRI) of a patient's specific anatomy, physicians can compare how alternative approaches affect blood flow and expected outcomes, and can select the best approach for each patient before entering the operating room. "This tool helps us to get the best result for each patient,” said coauthor Mark A. Fogel, M.D., an associate professor of cardiology and radiology, and director of cardiac MRI at the Children's Hospital of Philadelphia (PA, USA). "The team can assess the different surgical options to achieve the best blood flow and the optimum mixture of blood, so we can maximize the heart's energy efficiency.”
In the August 2009 issue of the Journal of the American College of Cardiology: Cardiovascular Imaging, the researchers described the surgical planning strategy, detailing how the application helped them to plan the surgery of a four-year-old girl who was born with just one functional ventricle, or pumping chamber, instead of two.
Two in every 1,000 babies in the United States alone are born with this type of single ventricle heart defect. These children typically suffer from low levels of oxygen in their tissues because their oxygen-rich and oxygen-poor blood mix in their one functional ventricle before being redistributed to their lungs and body.
To correct this, the children undergo a series of three open-heart surgeries called the staged Fontan reconstruction to reshape the circulation in a way that allows oxygen-poor blood to flow from the limbs directly to the lungs without going through the heart. While these vascular modifications can eliminate blood mixing and restore normal oxygenation levels, surgeons and cardiologists must ensure that the lungs will receive proper amounts of blood and nutrients after the surgery so that normal development occurs.
"Preoperatively determining the Fontan configuration that will achieve balanced blood flow to the lungs is very difficult and the wide variety and complexity of patients' anatomies requires an approach that is very specific and personalized,” said Ajit Yoganathan, Ph.D., a professor in the department of biomedical engineering at Georgia Institute of Technology (Georgia Tech; Atlanta, USA). "With our surgical planning framework, the physicians gain a better understanding of each child's unique heart defect, thus improving the surgery outcome and recovery time.”
The patient described in the study, a girl, age four, from Staten Island (NY, USA) had previously undergone all three stages of the Fontan procedure at the Children's Hospital of Philadelphia, but developed severe complications. Her oxygen saturation was very low only 72%, compared to normal levels of at least 95%, which indicated the possibility of abnormal connections between the veins and arteries in one of her lungs. Typically, the liver releases hormonal factors that prevent these abnormal connections, so the presence of the malformations indicated a low supply of hepatic blood to the lung.
To improve the distribution of these hormonal factors to both lungs, the surgeons needed to operate again and reconfigure the patient's cardiovascular anatomy. Georgia Tech's surgical planning framework helped Thomas L. Spray, M.D., chief of the division of cardiothoracic surgery at Children's Hospital, to determine the optimal surgical option. "MRI acquires images of the child's heart without using radiation,” said Dr. Spray. "Then we use the computerized technology to model different connections to simulate optimum blood flow characteristics, before we perform the surgery.”
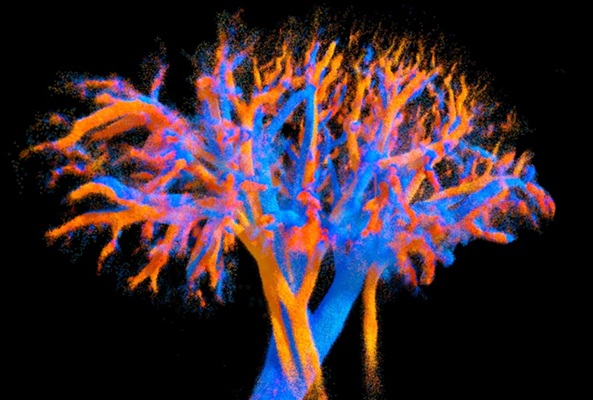
The image-based surgical planning consisted of five major steps: acquiring MR images of the child's heart at different times in the cardiac cycle, modeling the preoperative heart anatomy and blood flow, performing virtual surgeries, using computational fluid dynamics to model the proposed postoperative flow, and measuring the distribution of liver-derived hormonal factors and other clinically relevant parameters as feedback to the surgeon.
Dr. Fogel collected three different types of MR images, and Dr. Yoganathan, along with graduate students Kartik Sundareswaran and Diane de Zélicourt, generated a three dimensional model of the child's cardiovascular anatomy. From the model, they reconstructed the three-dimensional preoperative flow fields to understand the underlying causes of the malformations.
For this particular patient, the team saw a highly uneven flow distribution the left lung was receiving about 70% of the blood pumped out by the heart, but only 5% of the hepatic blood. Both observations suggested left lung malformations, but closer examination of the flow structures in that particular patient revealed that the competition between different vessels at the center of the original Fontan connection effectively forced all hepatic factors into the right lung even though a vast majority of total cardiac output went to the left lung.
To facilitate the design of the surgical options that would correct this problem, Jarek Rossignac, Ph.D., a professor in Georgia Tech's School of Interactive Computing, developed Surgem, an interactive geometric modeling environment that allowed the surgeon to use both hands and natural gestures in three-dimensions to grab, pull, twist, and bend a 3D computer representation of the patient's anatomy. After analyzing the 3D reconstruction of the failing cardiovascular geometry, the team considered three surgical options.
The research team then performed computational fluid dynamics simulations on all three options to investigate for each how well blood would flow to the lungs and the amount of energy required to drive blood through each connection design. These measures of clinical performance allowed the cardiologists and surgeons to conduct a risk/benefit analysis, which also included factors such as difficulty of completion and potential complications.
Of the three choices, Dr. Spray favored the option that showed a slightly higher energy cost but exhibited the best performance concerning hepatic factor distribution to the left and right lungs. Five months after the surgery, Dr. Mayer showed a dramatic improvement in her overall clinical condition and oxygen saturation levels, which increased from 72-94%. The child is breathing easier and is now able to play actively like other children, according to her cardiologist.
"The ability to perform this work is a team effort,” Dr. Fogel added. "State-of-the-art three-dimensional cardiac MRI married to modern biomedical engineering and applied anatomy and physiology enabled this approach. With the advanced pediatric cardiothoracic surgery we have here at The Children's Hospital of Philadelphia, patients can benefit from this new method.”
Related Links:
Children's Hospital of Philadelphia
Georgia Institute of Technology
By manipulating three-dimensional (3D) cardiac magnetic resonance images (MRI) of a patient's specific anatomy, physicians can compare how alternative approaches affect blood flow and expected outcomes, and can select the best approach for each patient before entering the operating room. "This tool helps us to get the best result for each patient,” said coauthor Mark A. Fogel, M.D., an associate professor of cardiology and radiology, and director of cardiac MRI at the Children's Hospital of Philadelphia (PA, USA). "The team can assess the different surgical options to achieve the best blood flow and the optimum mixture of blood, so we can maximize the heart's energy efficiency.”
In the August 2009 issue of the Journal of the American College of Cardiology: Cardiovascular Imaging, the researchers described the surgical planning strategy, detailing how the application helped them to plan the surgery of a four-year-old girl who was born with just one functional ventricle, or pumping chamber, instead of two.
Two in every 1,000 babies in the United States alone are born with this type of single ventricle heart defect. These children typically suffer from low levels of oxygen in their tissues because their oxygen-rich and oxygen-poor blood mix in their one functional ventricle before being redistributed to their lungs and body.
To correct this, the children undergo a series of three open-heart surgeries called the staged Fontan reconstruction to reshape the circulation in a way that allows oxygen-poor blood to flow from the limbs directly to the lungs without going through the heart. While these vascular modifications can eliminate blood mixing and restore normal oxygenation levels, surgeons and cardiologists must ensure that the lungs will receive proper amounts of blood and nutrients after the surgery so that normal development occurs.
"Preoperatively determining the Fontan configuration that will achieve balanced blood flow to the lungs is very difficult and the wide variety and complexity of patients' anatomies requires an approach that is very specific and personalized,” said Ajit Yoganathan, Ph.D., a professor in the department of biomedical engineering at Georgia Institute of Technology (Georgia Tech; Atlanta, USA). "With our surgical planning framework, the physicians gain a better understanding of each child's unique heart defect, thus improving the surgery outcome and recovery time.”
The patient described in the study, a girl, age four, from Staten Island (NY, USA) had previously undergone all three stages of the Fontan procedure at the Children's Hospital of Philadelphia, but developed severe complications. Her oxygen saturation was very low only 72%, compared to normal levels of at least 95%, which indicated the possibility of abnormal connections between the veins and arteries in one of her lungs. Typically, the liver releases hormonal factors that prevent these abnormal connections, so the presence of the malformations indicated a low supply of hepatic blood to the lung.
To improve the distribution of these hormonal factors to both lungs, the surgeons needed to operate again and reconfigure the patient's cardiovascular anatomy. Georgia Tech's surgical planning framework helped Thomas L. Spray, M.D., chief of the division of cardiothoracic surgery at Children's Hospital, to determine the optimal surgical option. "MRI acquires images of the child's heart without using radiation,” said Dr. Spray. "Then we use the computerized technology to model different connections to simulate optimum blood flow characteristics, before we perform the surgery.”
The image-based surgical planning consisted of five major steps: acquiring MR images of the child's heart at different times in the cardiac cycle, modeling the preoperative heart anatomy and blood flow, performing virtual surgeries, using computational fluid dynamics to model the proposed postoperative flow, and measuring the distribution of liver-derived hormonal factors and other clinically relevant parameters as feedback to the surgeon.
Dr. Fogel collected three different types of MR images, and Dr. Yoganathan, along with graduate students Kartik Sundareswaran and Diane de Zélicourt, generated a three dimensional model of the child's cardiovascular anatomy. From the model, they reconstructed the three-dimensional preoperative flow fields to understand the underlying causes of the malformations.
For this particular patient, the team saw a highly uneven flow distribution the left lung was receiving about 70% of the blood pumped out by the heart, but only 5% of the hepatic blood. Both observations suggested left lung malformations, but closer examination of the flow structures in that particular patient revealed that the competition between different vessels at the center of the original Fontan connection effectively forced all hepatic factors into the right lung even though a vast majority of total cardiac output went to the left lung.
To facilitate the design of the surgical options that would correct this problem, Jarek Rossignac, Ph.D., a professor in Georgia Tech's School of Interactive Computing, developed Surgem, an interactive geometric modeling environment that allowed the surgeon to use both hands and natural gestures in three-dimensions to grab, pull, twist, and bend a 3D computer representation of the patient's anatomy. After analyzing the 3D reconstruction of the failing cardiovascular geometry, the team considered three surgical options.
The research team then performed computational fluid dynamics simulations on all three options to investigate for each how well blood would flow to the lungs and the amount of energy required to drive blood through each connection design. These measures of clinical performance allowed the cardiologists and surgeons to conduct a risk/benefit analysis, which also included factors such as difficulty of completion and potential complications.
Of the three choices, Dr. Spray favored the option that showed a slightly higher energy cost but exhibited the best performance concerning hepatic factor distribution to the left and right lungs. Five months after the surgery, Dr. Mayer showed a dramatic improvement in her overall clinical condition and oxygen saturation levels, which increased from 72-94%. The child is breathing easier and is now able to play actively like other children, according to her cardiologist.
"The ability to perform this work is a team effort,” Dr. Fogel added. "State-of-the-art three-dimensional cardiac MRI married to modern biomedical engineering and applied anatomy and physiology enabled this approach. With the advanced pediatric cardiothoracic surgery we have here at The Children's Hospital of Philadelphia, patients can benefit from this new method.”
Related Links:
Children's Hospital of Philadelphia
Georgia Institute of Technology
Latest MRI News
- Novel Imaging Approach to Improve Treatment for Spinal Cord Injuries
- AI-Assisted Model Enhances MRI Heart Scans
- AI Model Outperforms Doctors at Identifying Patients Most At-Risk of Cardiac Arrest
- New MRI Technique Reveals Hidden Heart Issues
- Shorter MRI Exam Effectively Detects Cancer in Dense Breasts
- MRI to Replace Painful Spinal Tap for Faster MS Diagnosis
- MRI Scans Can Identify Cardiovascular Disease Ten Years in Advance
- Simple Brain Scan Diagnoses Parkinson's Disease Years Before It Becomes Untreatable
- Cutting-Edge MRI Technology to Revolutionize Diagnosis of Common Heart Problem
- New MRI Technique Reveals True Heart Age to Prevent Attacks and Strokes
- AI Tool Predicts Relapse of Pediatric Brain Cancer from Brain MRI Scans
- AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
- Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
- AI-Powered MRI Technology Improves Parkinson’s Diagnoses
- Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
- First-Of-Its-Kind AI-Driven Brain Imaging Platform to Better Guide Stroke Treatment Options
Channels
Radiography
view channel
X-Ray Breakthrough Captures Three Image-Contrast Types in Single Shot
Detecting early-stage cancer or subtle changes deep inside tissues has long challenged conventional X-ray systems, which rely only on how structures absorb radiation. This limitation keeps many microstructural... Read more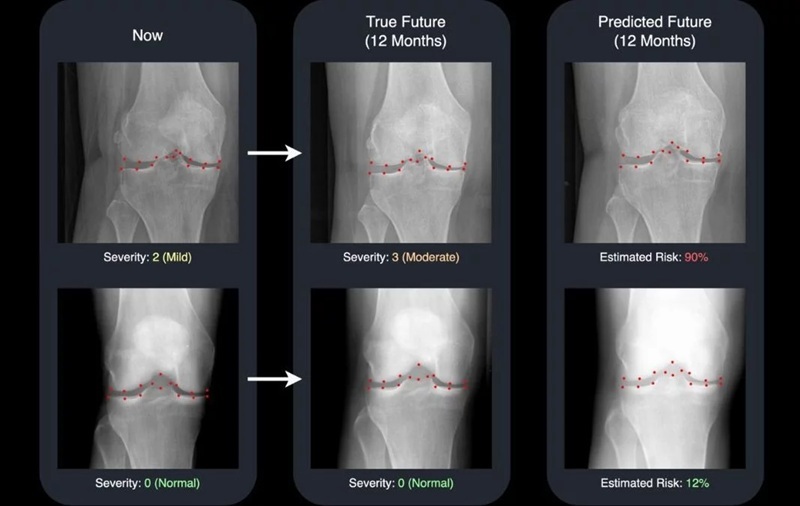
AI Generates Future Knee X-Rays to Predict Osteoarthritis Progression Risk
Osteoarthritis, a degenerative joint disease affecting over 500 million people worldwide, is the leading cause of disability among older adults. Current diagnostic tools allow doctors to assess damage... Read moreUltrasound
view channel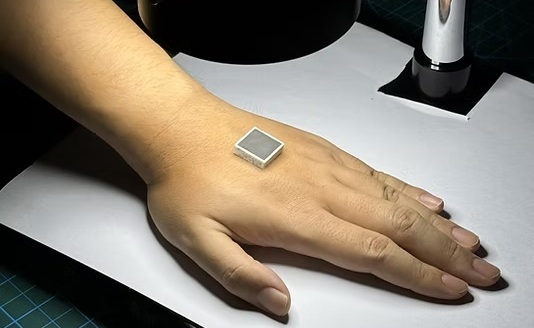
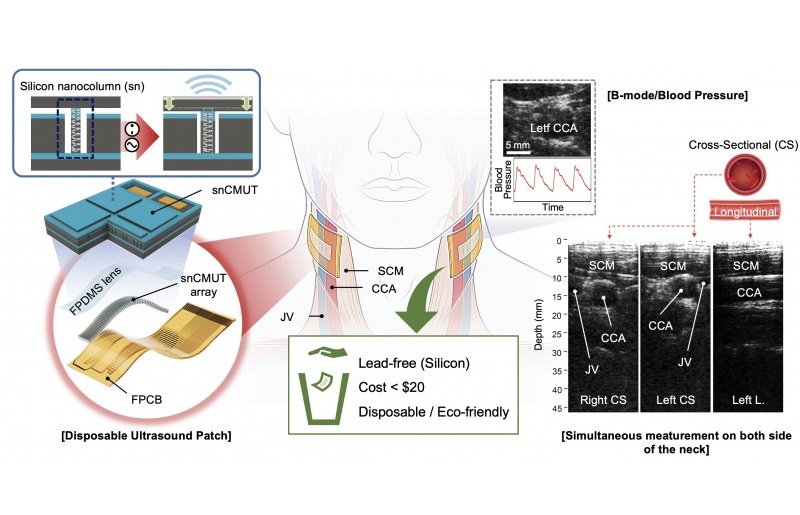
Wearable Ultrasound Imaging System to Enable Real-Time Disease Monitoring
Chronic conditions such as hypertension and heart failure require close monitoring, yet today’s ultrasound imaging is largely confined to hospitals and short, episodic scans. This reactive model limits... Read more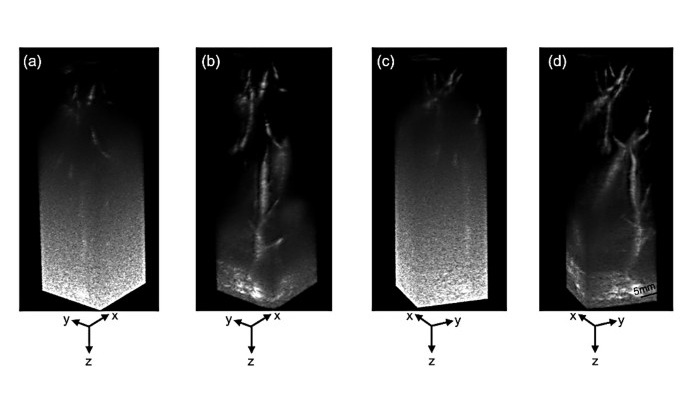
Ultrasound Technique Visualizes Deep Blood Vessels in 3D Without Contrast Agents
Producing clear 3D images of deep blood vessels has long been difficult without relying on contrast agents, CT scans, or MRI. Standard ultrasound typically provides only 2D cross-sections, limiting clinicians’... Read moreNuclear Medicine
view channel
PET Imaging of Inflammation Predicts Recovery and Guides Therapy After Heart Attack
Acute myocardial infarction can trigger lasting heart damage, yet clinicians still lack reliable tools to identify which patients will regain function and which may develop heart failure.... Read more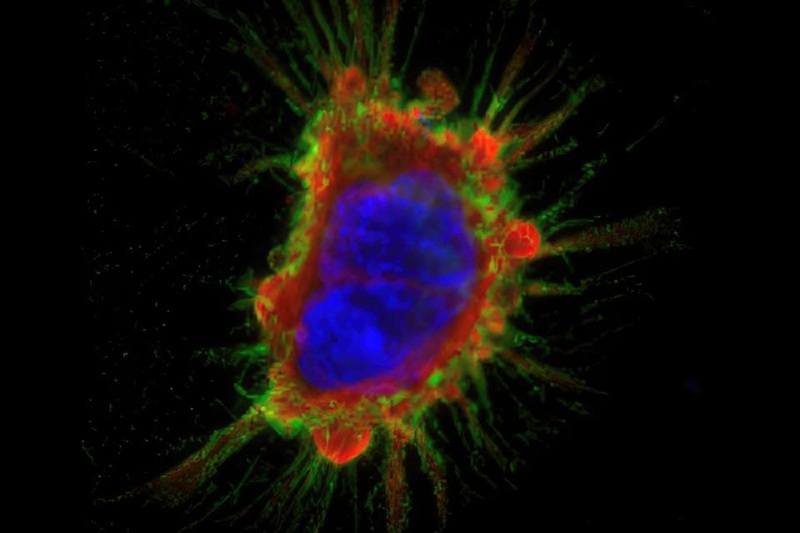
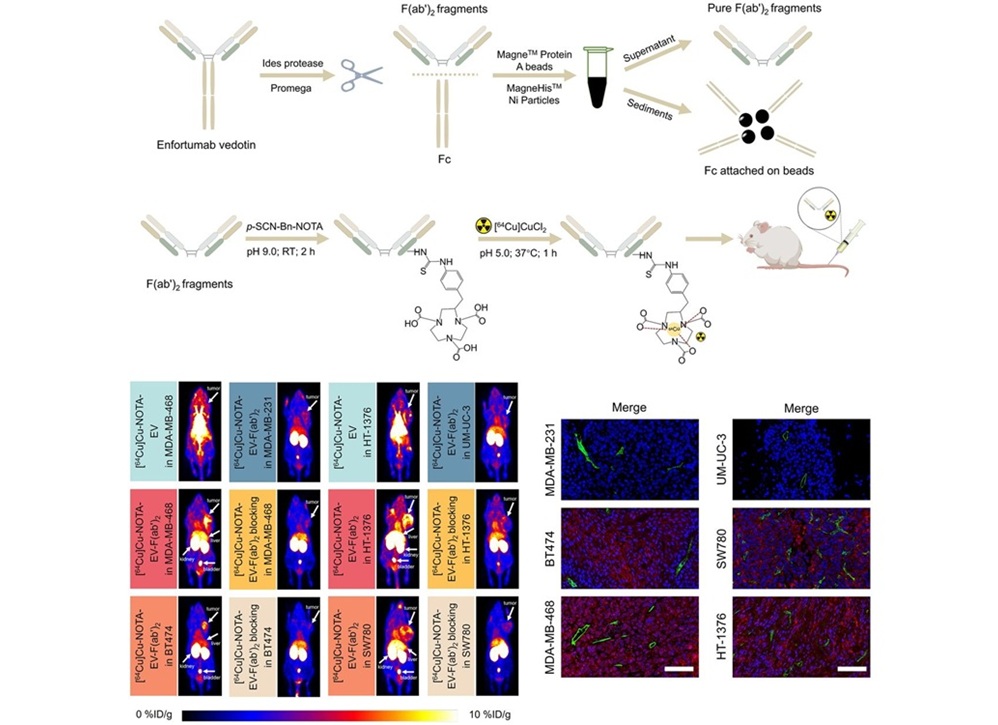
Radiotheranostic Approach Detects, Kills and Reprograms Aggressive Cancers
Aggressive cancers such as osteosarcoma and glioblastoma often resist standard therapies, thrive in hostile tumor environments, and recur despite surgery, radiation, or chemotherapy. These tumors also... Read more
New Imaging Solution Improves Survival for Patients with Recurring Prostate Cancer
Detecting recurrent prostate cancer remains one of the most difficult challenges in oncology, as standard imaging methods such as bone scans and CT scans often fail to accurately locate small or early-stage tumors.... Read moreGeneral/Advanced Imaging
view channel
3D Scanning Approach Enables Ultra-Precise Brain Surgery
Precise navigation is critical in neurosurgery, yet even small alignment errors can affect outcomes when operating deep within the brain. A new 3D surface-scanning approach now provides a radiation-free... Read more
AI Tool Improves Medical Imaging Process by 90%
Accurately labeling different regions within medical scans, a process known as medical image segmentation, is critical for diagnosis, surgery planning, and research. Traditionally, this has been a manual... Read more
New Ultrasmall, Light-Sensitive Nanoparticles Could Serve as Contrast Agents
Medical imaging technologies face ongoing challenges in capturing accurate, detailed views of internal processes, especially in conditions like cancer, where tracking disease development and treatment... Read more
AI Algorithm Accurately Predicts Pancreatic Cancer Metastasis Using Routine CT Images
In pancreatic cancer, detecting whether the disease has spread to other organs is critical for determining whether surgery is appropriate. If metastasis is present, surgery is not recommended, yet current... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more