Focused Ultrasound Can Lessen Cancer Pain
|
By MedImaging International staff writers Posted on 19 May 2014 |
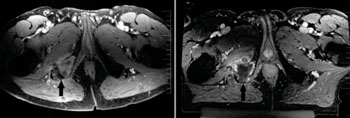
Image: Day of treatment pre- and post-procedure MR imaging. Axial T1-weighted contrast-enhanced MR images demonstrating a right ischial metastasis (black arrow) before treatment (left) and immediately after magnetic resonance-guided focused ultrasound surgery (MRgFUS) treatment (right). The post-treatment image shows nonenhancement of the lesion, which was targeted from a posterior approach. Each hash mark on the scale bars represents 1 cm (Photo courtesy of Journal of the US National Cancer Institute (JNCI)).
When cancer advances and metastasizes to the bone, patients often suffer debilitating pain. Now, a new phase III clinical trial shows that noninvasive magnetic resonance-guided focused ultrasound treatment that heats the cancer within the bone relieves pain and improves function for most patients when other treatment alternatives are limited.
The study’s findings were first published online April 23, 2014, in the Journal of the National Cancer Institute (JNCI).Magnetic resonance-guided focused ultrasound surgery (MRgFUS) is a technique that is been safely used to treat thousands of women with uterine fibroids. However, “this is the first phase III study to use this technology in the treatment of cancer,” noted the study’s principal investigator and lead author Mark Hurwitz, MD, vice chairman of quality, safety, and performance and director of thermal oncology in the department of radiation oncology at Thomas Jefferson University (Philadelphia, PA, USA).
Although radiotherapy is typically used to treat bone-related pain and effective for most patients, not all patients experience pain relief and over time those who do may have recurrence of pain. In addition, it's possible for a patient to receive the maximum radiation dose that can be safely delivered without fully controlling the pain. In situations where radiation therapy is not an option, alternative treatments are required.
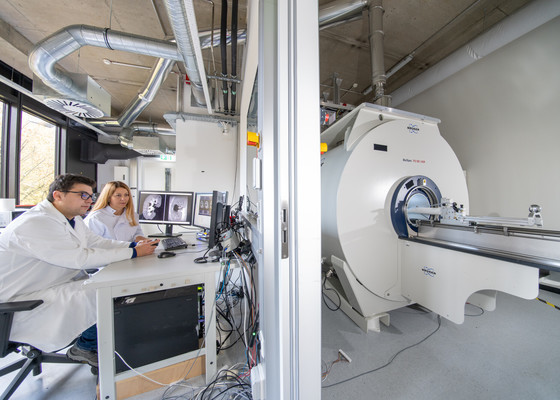
A total of 147 patients from 17 centers in the US, Canada, Israel, Italy, and Russia were enrolled in the study and randomized to undergo MRgFUS or a sham treatment. Patients in the treatment group received focused ultrasound precisely targeted to their bone tumors to heat the tumor tissue to between 65 °C and 85 °C, resulting in its obliteration. During each treatment, the patients were tracked real-time via magnetic resonance imaging (MRI) to make sure the appropriate tissue was targeted and the right temperatures were reached while ensuring heat in surrounding normal tissues and organs remained at safe levels. The control group underwent the same procedure but without the ultrasound device turned on. Finally, patients who did not respond to the placebo treatment within two weeks were allowed to be unblinded and offered MRgFUS.
Patients responded well to treatment, with 64% experiencing either no pain or a significant reduction in their pain at three months as gauged by a 2 point or greater decrease in the numeric rating score (NRS) for pain, a clinically validated measurement tool. Many patients were able to reduce or stop use of opiod medications. Significantly, most patients experienced pain relief and improved functioning within several days of treatment. “It’s clear that for many of these patients, pain has a major impact on their everyday lives," says Dr. Hurwitz. “This approach offers a new way to help alleviate that pain via an out-patient noninvasive procedure.”
The next phase in this research, according to Dr. Hurwitz, is to modify the treatment technique to get an even greater response rate, and to apply radiation and thermal therapy together in treatment of bone metastases noting the established clinical benefits for other malignant conditions with this combination. To achieve this, Dr. Jefferson has established a new program for thermal oncology within its department of radiation oncology to provide patients with access to thermal therapies that have been shown to augment radiation treatment.
“The work provides cancer patients with more options for treatment of cancer pain and the opportunity for patients to reduce opioid use, which has significant side effects,” said Adam Dicker, MD, PhD, chair of Jefferson’s department of radiation oncology, and not involved in the study.
Related Links:
Thomas Jefferson University
The study’s findings were first published online April 23, 2014, in the Journal of the National Cancer Institute (JNCI).Magnetic resonance-guided focused ultrasound surgery (MRgFUS) is a technique that is been safely used to treat thousands of women with uterine fibroids. However, “this is the first phase III study to use this technology in the treatment of cancer,” noted the study’s principal investigator and lead author Mark Hurwitz, MD, vice chairman of quality, safety, and performance and director of thermal oncology in the department of radiation oncology at Thomas Jefferson University (Philadelphia, PA, USA).
Although radiotherapy is typically used to treat bone-related pain and effective for most patients, not all patients experience pain relief and over time those who do may have recurrence of pain. In addition, it's possible for a patient to receive the maximum radiation dose that can be safely delivered without fully controlling the pain. In situations where radiation therapy is not an option, alternative treatments are required.
A total of 147 patients from 17 centers in the US, Canada, Israel, Italy, and Russia were enrolled in the study and randomized to undergo MRgFUS or a sham treatment. Patients in the treatment group received focused ultrasound precisely targeted to their bone tumors to heat the tumor tissue to between 65 °C and 85 °C, resulting in its obliteration. During each treatment, the patients were tracked real-time via magnetic resonance imaging (MRI) to make sure the appropriate tissue was targeted and the right temperatures were reached while ensuring heat in surrounding normal tissues and organs remained at safe levels. The control group underwent the same procedure but without the ultrasound device turned on. Finally, patients who did not respond to the placebo treatment within two weeks were allowed to be unblinded and offered MRgFUS.
Patients responded well to treatment, with 64% experiencing either no pain or a significant reduction in their pain at three months as gauged by a 2 point or greater decrease in the numeric rating score (NRS) for pain, a clinically validated measurement tool. Many patients were able to reduce or stop use of opiod medications. Significantly, most patients experienced pain relief and improved functioning within several days of treatment. “It’s clear that for many of these patients, pain has a major impact on their everyday lives," says Dr. Hurwitz. “This approach offers a new way to help alleviate that pain via an out-patient noninvasive procedure.”
The next phase in this research, according to Dr. Hurwitz, is to modify the treatment technique to get an even greater response rate, and to apply radiation and thermal therapy together in treatment of bone metastases noting the established clinical benefits for other malignant conditions with this combination. To achieve this, Dr. Jefferson has established a new program for thermal oncology within its department of radiation oncology to provide patients with access to thermal therapies that have been shown to augment radiation treatment.
“The work provides cancer patients with more options for treatment of cancer pain and the opportunity for patients to reduce opioid use, which has significant side effects,” said Adam Dicker, MD, PhD, chair of Jefferson’s department of radiation oncology, and not involved in the study.
Related Links:
Thomas Jefferson University
Latest Ultrasound News
- Diagnostic System Automatically Analyzes TTE Images to Identify Congenital Heart Disease
- Super-Resolution Imaging Technique Could Improve Evaluation of Cardiac Conditions

- First AI-Powered POC Ultrasound Diagnostic Solution Helps Prioritize Cases Based On Severity

- Largest Model Trained On Echocardiography Images Assesses Heart Structure and Function
- Groundbreaking Technology Enables Precise, Automatic Measurement of Peripheral Blood Vessels
- Deep Learning Advances Super-Resolution Ultrasound Imaging
- Novel Ultrasound-Launched Targeted Nanoparticle Eliminates Biofilm and Bacterial Infection
- AI-Guided Ultrasound System Enables Rapid Assessments of DVT
- Focused Ultrasound Technique Gets Quality Assurance Protocol
- AI-Guided Handheld Ultrasound System Helps Capture Diagnostic-Quality Cardiac Images
- Non-Invasive Ultrasound Imaging Device Diagnoses Risk of Chronic Kidney Disease
- Wearable Ultrasound Platform Paves Way for 24/7 Blood Pressure Monitoring On the Wrist
- Diagnostic Ultrasound Enhancing Agent to Improve Image Quality in Pediatric Heart Patients
- AI Detects COVID-19 in Lung Ultrasound Images
- New Ultrasound Technology to Revolutionize Respiratory Disease Diagnoses
- Dynamic Contrast-Enhanced Ultrasound Highly Useful For Interventions
Channels
Radiography
view channel
Novel Breast Imaging System Proves As Effective As Mammography
Breast cancer remains the most frequently diagnosed cancer among women. It is projected that one in eight women will be diagnosed with breast cancer during her lifetime, and one in 42 women who turn 50... Read more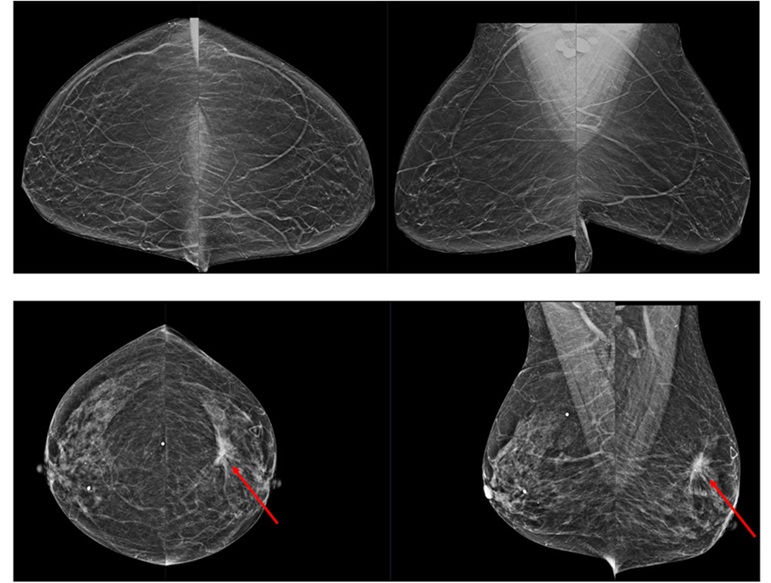
AI Assistance Improves Breast-Cancer Screening by Reducing False Positives
Radiologists typically detect one case of cancer for every 200 mammograms reviewed. However, these evaluations often result in false positives, leading to unnecessary patient recalls for additional testing,... Read moreMRI
view channel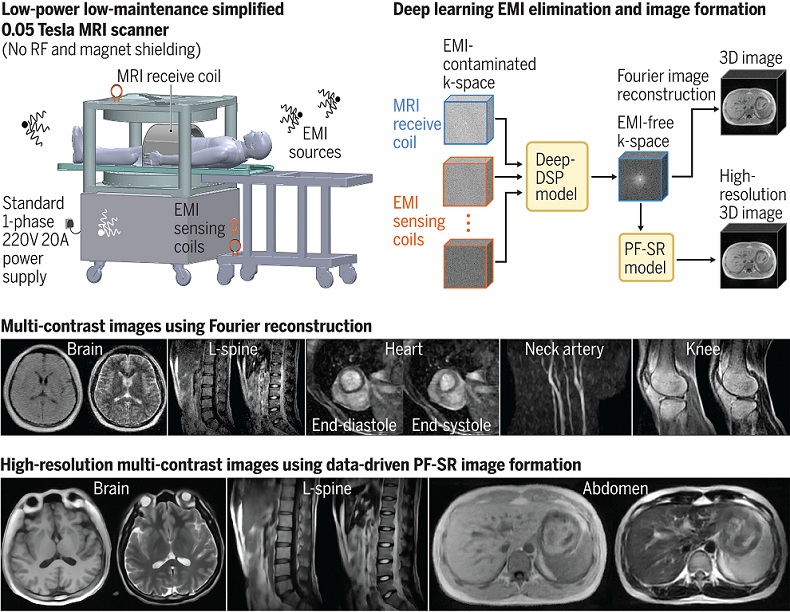
Low-Cost Whole-Body MRI Device Combined with AI Generates High-Quality Results
Magnetic Resonance Imaging (MRI) has significantly transformed healthcare, providing a noninvasive, radiation-free method for detailed imaging. It is especially promising for the future of medical diagnosis... Read more
World's First Whole-Body Ultra-High Field MRI Officially Comes To Market
The world's first whole-body ultra-high field (UHF) MRI has officially come to market, marking a remarkable advancement in diagnostic radiology. United Imaging (Shanghai, China) has secured clearance from the U.... Read moreNuclear Medicine
view channel
New PET Biomarker Predicts Success of Immune Checkpoint Blockade Therapy
Immunotherapies, such as immune checkpoint blockade (ICB), have shown promising clinical results in treating melanoma, non-small cell lung cancer, and other tumor types. However, the effectiveness of these... Read moreNew PET Agent Rapidly and Accurately Visualizes Lesions in Clear Cell Renal Cell Carcinoma Patients
Clear cell renal cell cancer (ccRCC) represents 70-80% of renal cell carcinoma cases. While localized disease can be effectively treated with surgery and ablative therapies, one-third of patients either... Read more
New Imaging Technique Monitors Inflammation Disorders without Radiation Exposure
Imaging inflammation using traditional radiological techniques presents significant challenges, including radiation exposure, poor image quality, high costs, and invasive procedures. Now, new contrast... Read more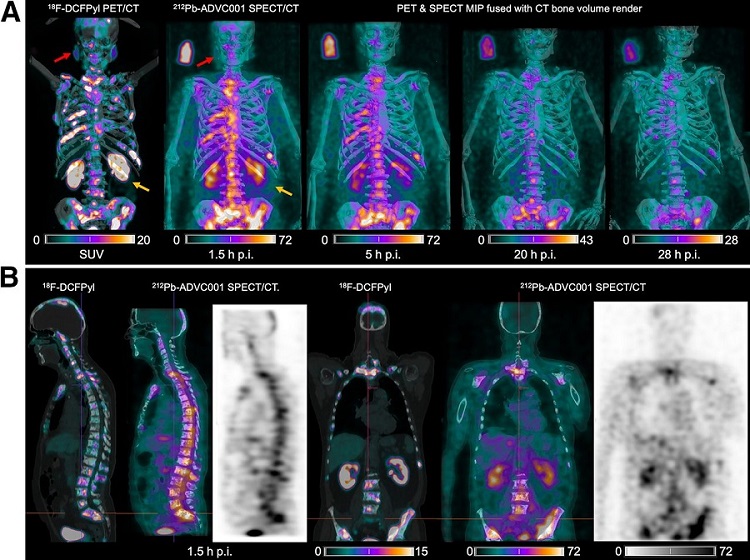
New SPECT/CT Technique Could Change Imaging Practices and Increase Patient Access
The development of lead-212 (212Pb)-PSMA–based targeted alpha therapy (TAT) is garnering significant interest in treating patients with metastatic castration-resistant prostate cancer. The imaging of 212Pb,... Read moreGeneral/Advanced Imaging
view channelBone Density Test Uses Existing CT Images to Predict Fractures
Osteoporotic fractures are not only devastating and deadly, especially hip fractures, but also impose significant costs. They rank among the top chronic diseases in terms of disability-adjusted life years... Read more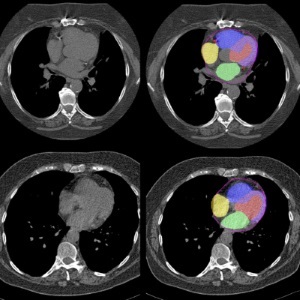
AI Predicts Cardiac Risk and Mortality from Routine Chest CT Scans
Heart disease remains the leading cause of death and is largely preventable, yet many individuals are unaware of their risk until it becomes severe. Early detection through screening can reveal heart issues,... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
Hologic Acquires UK-Based Breast Surgical Guidance Company Endomagnetics Ltd.
Hologic, Inc. (Marlborough, MA, USA) has entered into a definitive agreement to acquire Endomagnetics Ltd. (Cambridge, UK), a privately held developer of breast cancer surgery technologies, for approximately... Read more
Bayer and Google Partner on New AI Product for Radiologists
Medical imaging data comprises around 90% of all healthcare data, and it is a highly complex and rich clinical data modality and serves as a vital tool for diagnosing patients. Each year, billions of medical... Read more