MRI-Ultrasound Fusion-Guided Biopsy Detects Prostate Cancer
|
By MedImaging International staff writers Posted on 24 Dec 2012 |
Cutting-edge research conducted by a group of engineers and clinicians demonstrates that prostate cancer—long detected only through hit-or-miss and painful biopsies—can be diagnosed far more easily and effectively using a new image-guided, targeted biopsy procedure.
Customarily, prostate tumors have been identified through so-called blind biopsies, in which tissue samples are gathered systematically from the entire prostate in the prospect of finding a part of a tumor--a strategy that was developed in the 1980s. But the tumor now can be detectable by direct sampling of tumor spots detected using magnetic resonance imaging (MRI), in combination with real-time ultrasound, according to the University of California, Los Angeles (UCLA; USA) researchers.
The study’s findings are published December 10, 2012, in the early online edition of the Journal of Urology and are scheduled for print publication in the journal's January 2013 issue. The UCLA study indicates that the MRI–ultrasound fusion biopsy, which is much more accurate than a conventional blind biopsy, may lead to a decrease in the number of prostate biopsies performed and could allow for the early detection of serious prostate tumors.
The study involved 171 men who were either undergoing active surveillance to monitor slow-growing prostate cancers or who, despite prior negative biopsies, had persistently elevated levels of prostate-specific antigen (PSA), a protein produced by the prostate that can indicate the presence of cancer. The UCLA biopsies using the new technique were done in about 20 minutes in an outpatient clinic environment under local anesthesia.
Yearly, almost all of the one million prostate biopsies performed in the United States are prompted by elevations in prostate-specific antigen (PSA) levels, and approximately 240,000 new instances of prostate cancer are found each year. Therefore, approximately 75% of biopsies are negative for cancer. However, many men with negative biopsies but elevated PSA levels may still harbor malignant tumors—tumors missed by traditional biopsies, according to the study’s senior author, Dr. Leonard S. Marks, a professor of urology and director of UCLA’s active surveillance program.
“Early prostate cancer is difficult to image because of the limited contrast between normal and malignant tissues within the prostate,” Dr. Marks said. “Conventional biopsies are basically performed blindly because we can’t see what we’re aiming for. Now, with this new method, which fuses MRI and ultrasound, we have the potential to see the prostate cancer and aim for it in a much more refined and rational manner.”
The new targeting process is the outcome of four years of work funded by the US National Cancer Institute and based at the Clark Urology Center at UCLA.
Since the mid-1980s, prostate cancer has been diagnosed using transrectal ultrasound to sample the prostate. Unlike most other cancers, prostate cancer is the only major malignancy diagnosed without actually visualizing the tumor as a biopsy is performed, according to Dr. Marks.
With the development of sophisticated MRI technology, the ability to image the prostate improved and provided an image of tumors within the organ. However, trying to biopsy the prostate with the patient inside an MRI scanner turned out to be costly, awkward, and time-consuming. However, with the development of the new MRI-ultrasound fusion process, the biopsy can now be performed in a clinic setting.
In the study, the volunteers first underwent MRI to visualize the prostate and any lesions. That data were then fed into a device called the Artemis, which electronically fuses the MR images with real-time, three-dimensional (3D) ultrasound, allowing the urologist to see the lesion during the biopsy. “With the Artemis, we have a virtual map of the suspicious areas placed directly onto the ultrasound image during the biopsy,” Dr. Marks said. “When you can see a lesion, you’ve got a major advantage of knowing what’s really going on in the prostate. The results have been very dramatic, and the rate of cancer detection in these targeted biopsies is very high. We’re finding a lot of tumors that hadn’t been found before using conventional biopsies.”
Prostate cancer was detected in 53% of 171 study participants. Of those tumors found using the fusion biopsy technique, 38% had a Gleason score of greater than seven, indicating an aggressive tumor and one more likely to metastasize than a tumor with lower scores. Once prostate cancer spreads, it is much more complicated to treat, and survival drops.
The UCLA study group of investigators included physicians and scientists from urology, radiology, pathology, the Center for Advanced Surgical and Interventional Technology (CASIT) and biomedical engineering. “Prostate lesions identified on MRI can be accurately targeted with MR-Ultrasound fusion biopsy in a clinic setting using local anesthesia,” the study authors stated. “Biopsy findings correlate with the level of suspicion on MRI. Targeted prostate biopsy has the potential to improve the diagnosis of prostate cancer and may aid in the selection of patients for active surveillance and focal therapy.”
The Artemis technology was developed by Eigen Corp. (Grass Valley, CA, USA).
Related Links:
University of California, Los Angeles
Eigen
Customarily, prostate tumors have been identified through so-called blind biopsies, in which tissue samples are gathered systematically from the entire prostate in the prospect of finding a part of a tumor--a strategy that was developed in the 1980s. But the tumor now can be detectable by direct sampling of tumor spots detected using magnetic resonance imaging (MRI), in combination with real-time ultrasound, according to the University of California, Los Angeles (UCLA; USA) researchers.
The study’s findings are published December 10, 2012, in the early online edition of the Journal of Urology and are scheduled for print publication in the journal's January 2013 issue. The UCLA study indicates that the MRI–ultrasound fusion biopsy, which is much more accurate than a conventional blind biopsy, may lead to a decrease in the number of prostate biopsies performed and could allow for the early detection of serious prostate tumors.
The study involved 171 men who were either undergoing active surveillance to monitor slow-growing prostate cancers or who, despite prior negative biopsies, had persistently elevated levels of prostate-specific antigen (PSA), a protein produced by the prostate that can indicate the presence of cancer. The UCLA biopsies using the new technique were done in about 20 minutes in an outpatient clinic environment under local anesthesia.
Yearly, almost all of the one million prostate biopsies performed in the United States are prompted by elevations in prostate-specific antigen (PSA) levels, and approximately 240,000 new instances of prostate cancer are found each year. Therefore, approximately 75% of biopsies are negative for cancer. However, many men with negative biopsies but elevated PSA levels may still harbor malignant tumors—tumors missed by traditional biopsies, according to the study’s senior author, Dr. Leonard S. Marks, a professor of urology and director of UCLA’s active surveillance program.
“Early prostate cancer is difficult to image because of the limited contrast between normal and malignant tissues within the prostate,” Dr. Marks said. “Conventional biopsies are basically performed blindly because we can’t see what we’re aiming for. Now, with this new method, which fuses MRI and ultrasound, we have the potential to see the prostate cancer and aim for it in a much more refined and rational manner.”
The new targeting process is the outcome of four years of work funded by the US National Cancer Institute and based at the Clark Urology Center at UCLA.
Since the mid-1980s, prostate cancer has been diagnosed using transrectal ultrasound to sample the prostate. Unlike most other cancers, prostate cancer is the only major malignancy diagnosed without actually visualizing the tumor as a biopsy is performed, according to Dr. Marks.
With the development of sophisticated MRI technology, the ability to image the prostate improved and provided an image of tumors within the organ. However, trying to biopsy the prostate with the patient inside an MRI scanner turned out to be costly, awkward, and time-consuming. However, with the development of the new MRI-ultrasound fusion process, the biopsy can now be performed in a clinic setting.
In the study, the volunteers first underwent MRI to visualize the prostate and any lesions. That data were then fed into a device called the Artemis, which electronically fuses the MR images with real-time, three-dimensional (3D) ultrasound, allowing the urologist to see the lesion during the biopsy. “With the Artemis, we have a virtual map of the suspicious areas placed directly onto the ultrasound image during the biopsy,” Dr. Marks said. “When you can see a lesion, you’ve got a major advantage of knowing what’s really going on in the prostate. The results have been very dramatic, and the rate of cancer detection in these targeted biopsies is very high. We’re finding a lot of tumors that hadn’t been found before using conventional biopsies.”
Prostate cancer was detected in 53% of 171 study participants. Of those tumors found using the fusion biopsy technique, 38% had a Gleason score of greater than seven, indicating an aggressive tumor and one more likely to metastasize than a tumor with lower scores. Once prostate cancer spreads, it is much more complicated to treat, and survival drops.
The UCLA study group of investigators included physicians and scientists from urology, radiology, pathology, the Center for Advanced Surgical and Interventional Technology (CASIT) and biomedical engineering. “Prostate lesions identified on MRI can be accurately targeted with MR-Ultrasound fusion biopsy in a clinic setting using local anesthesia,” the study authors stated. “Biopsy findings correlate with the level of suspicion on MRI. Targeted prostate biopsy has the potential to improve the diagnosis of prostate cancer and may aid in the selection of patients for active surveillance and focal therapy.”
The Artemis technology was developed by Eigen Corp. (Grass Valley, CA, USA).
Related Links:
University of California, Los Angeles
Eigen
Latest MRI News
- AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
- Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
- AI-Powered MRI Technology Improves Parkinson’s Diagnoses
- Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
- First-Of-Its-Kind AI-Driven Brain Imaging Platform to Better Guide Stroke Treatment Options
- New Model Improves Comparison of MRIs Taken at Different Institutions
- Groundbreaking New Scanner Sees 'Previously Undetectable' Cancer Spread
- First-Of-Its-Kind Tool Analyzes MRI Scans to Measure Brain Aging
- AI-Enhanced MRI Images Make Cancerous Breast Tissue Glow
- AI Model Automatically Segments MRI Images
- New Research Supports Routine Brain MRI Screening in Asymptomatic Late-Stage Breast Cancer Patients
- Revolutionary Portable Device Performs Rapid MRI-Based Stroke Imaging at Patient's Bedside
- AI Predicts After-Effects of Brain Tumor Surgery from MRI Scans
- MRI-First Strategy for Prostate Cancer Detection Proven Safe
- First-Of-Its-Kind 10' x 48' Mobile MRI Scanner Transforms User and Patient Experience
- New Model Makes MRI More Accurate and Reliable
Channels
Radiography
view channel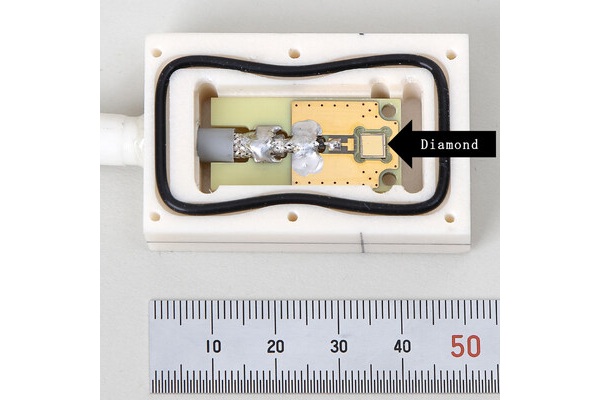
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read more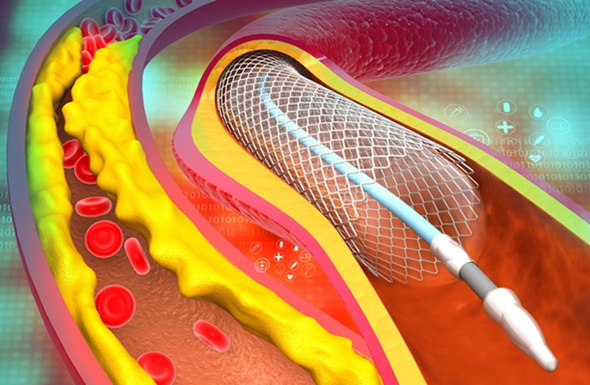
AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure where small metal tubes called stents are inserted into partially blocked coronary arteries... Read moreUltrasound
view channel
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read more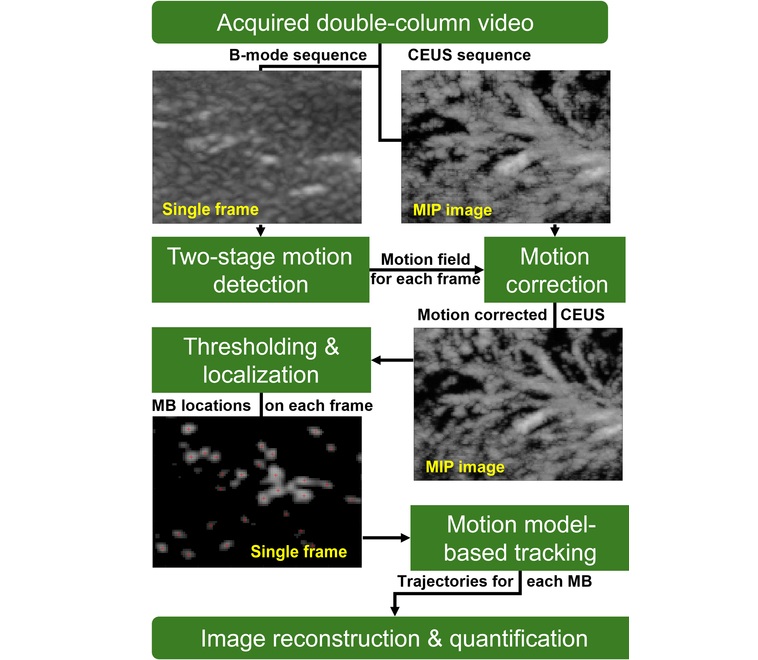
Novel Imaging Method Enables Early Diagnosis and Treatment Monitoring of Type 2 Diabetes
Type 2 diabetes is recognized as an autoimmune inflammatory disease, where chronic inflammation leads to alterations in pancreatic islet microvasculature, a key factor in β-cell dysfunction.... Read moreNuclear Medicine
view channel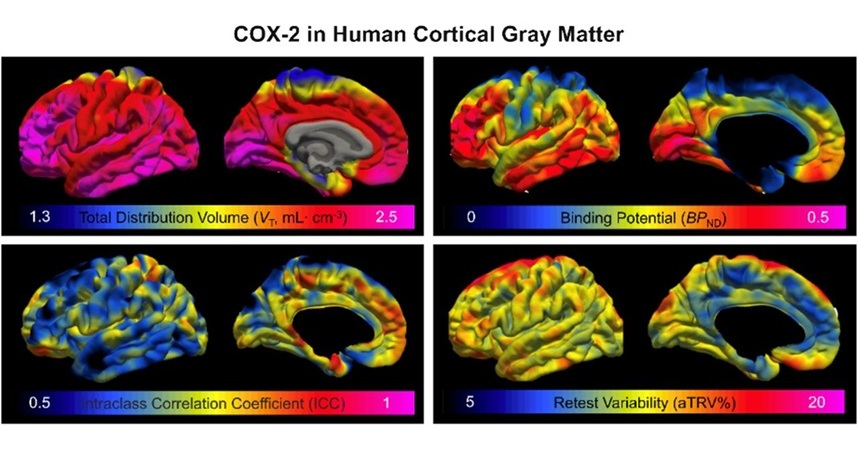
Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
COX-2, an enzyme that plays a key role in brain inflammation, can be significantly upregulated by inflammatory stimuli and neuroexcitation. Researchers suggest that COX-2 density in the brain could serve... Read more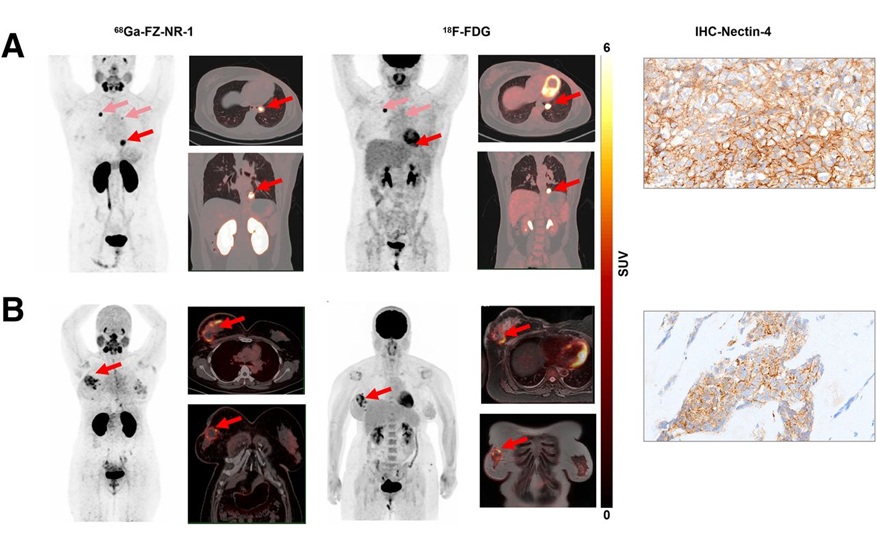
Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC), which represents 15-20% of all breast cancer cases, is one of the most aggressive subtypes, with a five-year survival rate of about 40%. Due to its significant heterogeneity... Read moreGeneral/Advanced Imaging
view channel
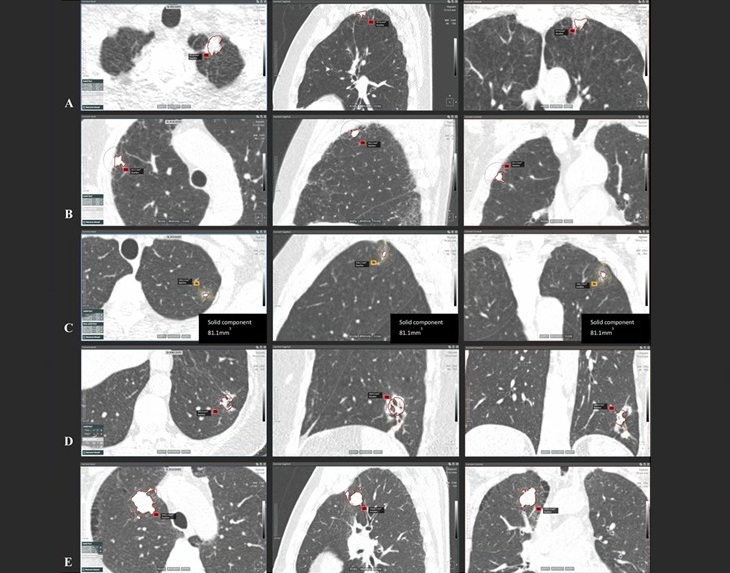
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read more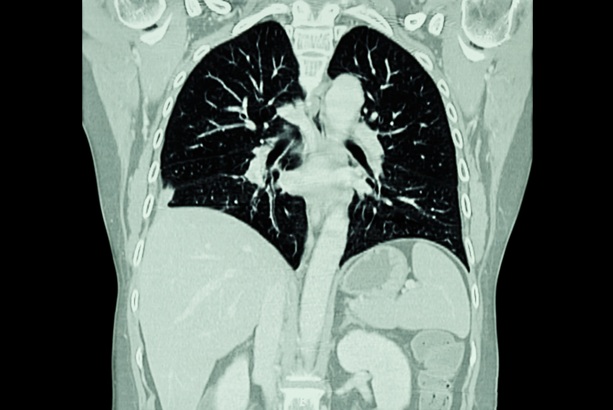
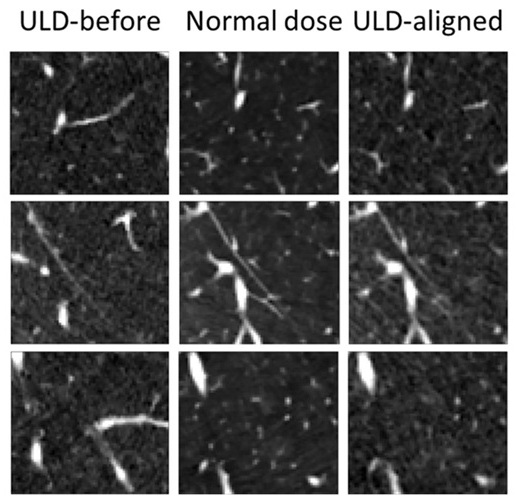
AI Model Significantly Enhances Low-Dose CT Capabilities
Lung cancer remains one of the most challenging diseases, making early diagnosis vital for effective treatment. Fortunately, advancements in artificial intelligence (AI) are revolutionizing lung cancer... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more