Integrated 3D Imaging Facilitates Human Face Transplantation
|
By MedImaging International staff writers Posted on 13 Dec 2011 |
Image: Darren Smith, MD, resident, UPMC Division of Plastic and Reconstructive Surgery, talks about a new fused 3-D model that can be manipulated by surgeons to prepare for complex face transplant surgeries. The technology is currently being developed by UPMC's Reconstructive Transplantation Program (Photo courtesy of the University of Pittsburgh Medical Center).
By incorporating traditional medical imaging with some of the same three-dimensional (3D) modeling techniques used in movies, researchers are providing new hope to victims of devastating facial injuries.
Findings of a new study on human face transplantation, led by Darren M. Smith, MD, plastic surgery resident from the University of Pittsburgh Medical Center (UPMC; PA, USA), were presented November 28, 2011, at the annual meeting of the Radiological Society of North America (RSNA) held in Chicago (IL, USA).
Serious injuries or defects of the face are incredibly challenging, if not impossible, to satisfactorily reconstruct by traditional surgical techniques. In face transplantation, facial tissue from a donor is transferred to reconstruct the defect, restore fundamental life-sustaining functions--such as breathing, chewing, and speaking--and most importantly, reestablish a normal human appearance.
“This surgery is for patients with devastating injuries to the face, who have lost their ability to smell, eat and engage socially and have no other conventional treatment options,” said Vijay S. Gorantla, MD, PhD, administrative medical director of the Reconstructive Transplantation Program at UPMC.
Distinctly defining and understanding the complex tissue deficits and defects that go along with devastating facial injuries like electric burns, blast wounds, and accidental trauma are critical for both technical effectiveness and objective analysis of the return of function after face transplantation.
Medical imaging plays a major role in the entire spectrum of face transplantation, ranging from patient selection, donor and recipient surgical planning, and postoperative assessment of returning motor and sensory function. Face transplantation is a long, complex procedure that involves reconstruction of multiple tissues--such as skin, muscle, blood vessels, nerves, and bone--by a team of surgeons.
Currently, to prepare for facial transplantation, plaster or plastic models are first created based on 3D computed tomography (CT) or angiographic images or reconstruction. Following this, mock cadaveric dissections are performed to allow surgeons to prepare for the donor and recipient surgeries. Magnetic resonance imaging (MRI) and other imaging exams may also be used to provide supplemental information.
By combining data from multiple imaging exams and creating a sophisticated 3-D computer model, the researchers for this study were better able to assess the facial structure and contours, the underlying bone, muscles, nerves, and vessels, as well as the extent of damage.
Using advanced computer modeling software, Drs. Smith and Gorantla, along with Joseph Losee, MD, integrated information from 3D CT, CT angiography, MRI and high-definition tractography to create a 3D model of the patient’s head and neck anatomy. The same kind of modeling technology is frequently used in movies to animate computer-generated characters with detailed 3D human features and realistic expressions.
“We have integrated data from multiple imaging sources into a single 3D representation that allows for real-time user interaction and modification,” Dr. Smith said. “In assessing eligibility for this procedure, it is critical to understand whether the patient has enough blood vessels and bone structure to support new facial tissue. This 3D modeling helps us customize the procedure to the patient’s individual anatomy so that the donor tissue will fit like a puzzle piece onto the patient’s face.”
Utilizing computer modeling, the team also overlaid the patient model with a polygon mesh of a generic human face and then personalized it to the recipient facial anatomy. Dr. Smith noted that the ability to manipulate this 3D facial wrapper over the residual face model allows the entire surgical team to participate in planning exactly where bone, blood vessel, and nerves will be cut and connected, as well as to assess the outcomes of reconstructive transplantation, including nerve regeneration within the transplanted facial tissue.
“The goal of face transplantation is not just structural,” Dr. Gorantla said. “It is about restoring function, so that patients are once again able to chew their food, smile and regain the most important aspect of a normal face--to look human."
Related Links:
University of Pittsburgh Medical Center
Video: Creating 3-D Models to Prepare for Face Transplants
Findings of a new study on human face transplantation, led by Darren M. Smith, MD, plastic surgery resident from the University of Pittsburgh Medical Center (UPMC; PA, USA), were presented November 28, 2011, at the annual meeting of the Radiological Society of North America (RSNA) held in Chicago (IL, USA).
Serious injuries or defects of the face are incredibly challenging, if not impossible, to satisfactorily reconstruct by traditional surgical techniques. In face transplantation, facial tissue from a donor is transferred to reconstruct the defect, restore fundamental life-sustaining functions--such as breathing, chewing, and speaking--and most importantly, reestablish a normal human appearance.
“This surgery is for patients with devastating injuries to the face, who have lost their ability to smell, eat and engage socially and have no other conventional treatment options,” said Vijay S. Gorantla, MD, PhD, administrative medical director of the Reconstructive Transplantation Program at UPMC.
Distinctly defining and understanding the complex tissue deficits and defects that go along with devastating facial injuries like electric burns, blast wounds, and accidental trauma are critical for both technical effectiveness and objective analysis of the return of function after face transplantation.
Medical imaging plays a major role in the entire spectrum of face transplantation, ranging from patient selection, donor and recipient surgical planning, and postoperative assessment of returning motor and sensory function. Face transplantation is a long, complex procedure that involves reconstruction of multiple tissues--such as skin, muscle, blood vessels, nerves, and bone--by a team of surgeons.
Currently, to prepare for facial transplantation, plaster or plastic models are first created based on 3D computed tomography (CT) or angiographic images or reconstruction. Following this, mock cadaveric dissections are performed to allow surgeons to prepare for the donor and recipient surgeries. Magnetic resonance imaging (MRI) and other imaging exams may also be used to provide supplemental information.
By combining data from multiple imaging exams and creating a sophisticated 3-D computer model, the researchers for this study were better able to assess the facial structure and contours, the underlying bone, muscles, nerves, and vessels, as well as the extent of damage.
Using advanced computer modeling software, Drs. Smith and Gorantla, along with Joseph Losee, MD, integrated information from 3D CT, CT angiography, MRI and high-definition tractography to create a 3D model of the patient’s head and neck anatomy. The same kind of modeling technology is frequently used in movies to animate computer-generated characters with detailed 3D human features and realistic expressions.
“We have integrated data from multiple imaging sources into a single 3D representation that allows for real-time user interaction and modification,” Dr. Smith said. “In assessing eligibility for this procedure, it is critical to understand whether the patient has enough blood vessels and bone structure to support new facial tissue. This 3D modeling helps us customize the procedure to the patient’s individual anatomy so that the donor tissue will fit like a puzzle piece onto the patient’s face.”
Utilizing computer modeling, the team also overlaid the patient model with a polygon mesh of a generic human face and then personalized it to the recipient facial anatomy. Dr. Smith noted that the ability to manipulate this 3D facial wrapper over the residual face model allows the entire surgical team to participate in planning exactly where bone, blood vessel, and nerves will be cut and connected, as well as to assess the outcomes of reconstructive transplantation, including nerve regeneration within the transplanted facial tissue.
“The goal of face transplantation is not just structural,” Dr. Gorantla said. “It is about restoring function, so that patients are once again able to chew their food, smile and regain the most important aspect of a normal face--to look human."
Related Links:
University of Pittsburgh Medical Center
Video: Creating 3-D Models to Prepare for Face Transplants
Latest MRI News
- AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
- Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
- AI-Powered MRI Technology Improves Parkinson’s Diagnoses
- Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
- First-Of-Its-Kind AI-Driven Brain Imaging Platform to Better Guide Stroke Treatment Options
- New Model Improves Comparison of MRIs Taken at Different Institutions
- Groundbreaking New Scanner Sees 'Previously Undetectable' Cancer Spread
- First-Of-Its-Kind Tool Analyzes MRI Scans to Measure Brain Aging
- AI-Enhanced MRI Images Make Cancerous Breast Tissue Glow
- AI Model Automatically Segments MRI Images
- New Research Supports Routine Brain MRI Screening in Asymptomatic Late-Stage Breast Cancer Patients
- Revolutionary Portable Device Performs Rapid MRI-Based Stroke Imaging at Patient's Bedside
- AI Predicts After-Effects of Brain Tumor Surgery from MRI Scans
- MRI-First Strategy for Prostate Cancer Detection Proven Safe
- First-Of-Its-Kind 10' x 48' Mobile MRI Scanner Transforms User and Patient Experience
- New Model Makes MRI More Accurate and Reliable
Channels
Radiography
view channel
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read more
AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure where small metal tubes called stents are inserted into partially blocked coronary arteries... Read moreUltrasound
view channel
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read more
Novel Imaging Method Enables Early Diagnosis and Treatment Monitoring of Type 2 Diabetes
Type 2 diabetes is recognized as an autoimmune inflammatory disease, where chronic inflammation leads to alterations in pancreatic islet microvasculature, a key factor in β-cell dysfunction.... Read moreNuclear Medicine
view channel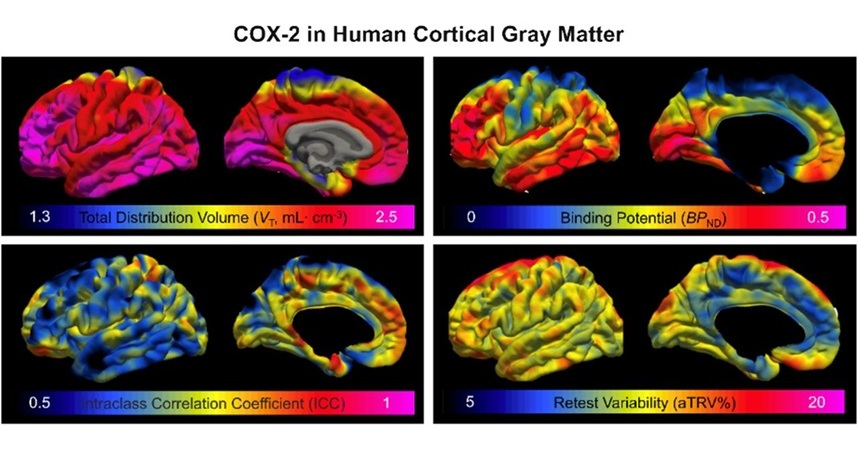
Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
COX-2, an enzyme that plays a key role in brain inflammation, can be significantly upregulated by inflammatory stimuli and neuroexcitation. Researchers suggest that COX-2 density in the brain could serve... Read more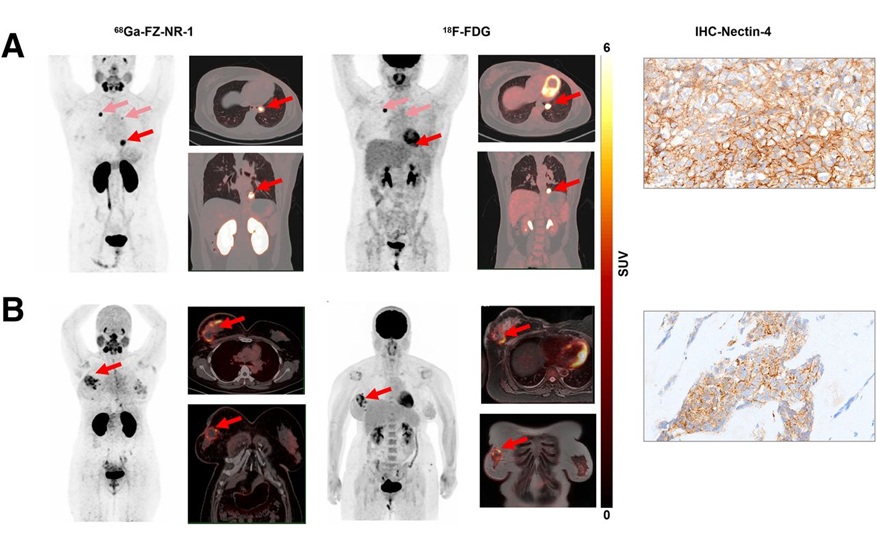
Novel Radiotracer Identifies Biomarker for Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC), which represents 15-20% of all breast cancer cases, is one of the most aggressive subtypes, with a five-year survival rate of about 40%. Due to its significant heterogeneity... Read moreGeneral/Advanced Imaging
view channel
AI-Powered Imaging System Improves Lung Cancer Diagnosis
Given the need to detect lung cancer at earlier stages, there is an increasing need for a definitive diagnostic pathway for patients with suspicious pulmonary nodules. However, obtaining tissue samples... Read more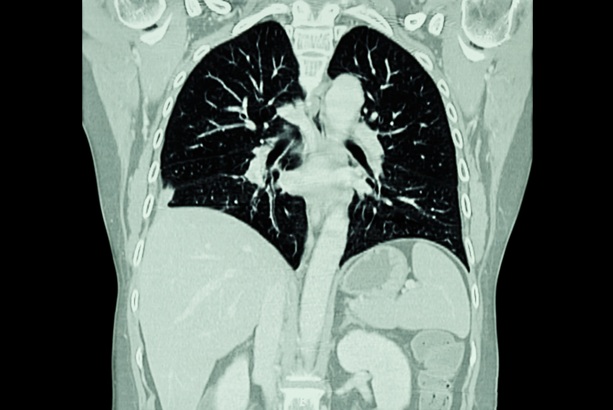
AI Model Significantly Enhances Low-Dose CT Capabilities
Lung cancer remains one of the most challenging diseases, making early diagnosis vital for effective treatment. Fortunately, advancements in artificial intelligence (AI) are revolutionizing lung cancer... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more