AI Algorithm Identifies Lung Cancer on CT Scans within Seconds
|
By MedImaging International staff writers Posted on 26 Aug 2022 |

Lung cancer, the most common cancer worldwide, is targeted with radiation therapy (RT) in nearly one-half of cases. RT planning is a manual, resource-intensive process that can take days to weeks to complete, and even highly trained physicians vary in their determinations of how much tissue to target with radiation. Furthermore, a shortage of radiation-oncology practitioners and clinics worldwide is expected to grow as cancer rates increase. Now, a newly developed and validated deep learning algorithm can identify and outline (segment) a non-small cell lung cancer (NSCLC) tumor on a computed tomography (CT) scan within seconds. Additionally, radiation oncologists using the algorithm in simulated clinics performed as well as physicians not using the algorithm, while working 65% more quickly.
Researchers at the Brigham and Women's Hospital (Boston, MA, USA) developed the deep learning algorithm by using CT images from 787 patients to train their model to distinguish tumors from other tissues. They tested the algorithm’s performance using scans from over 1,300 patients from increasingly external datasets. Developing and validating the algorithm involved close collaboration between data scientists and radiation oncologists. For example, when the researchers observed that the algorithm was incorrectly segmenting CT scans involving the lymph nodes, they retrained the model with more of these scans to improve its performance.
Finally, the researchers asked eight radiation oncologists to perform segmentation tasks as well as rate and edit segmentations produced by either another expert physician or the algorithm (they were not told which). There was no significant difference in performance between human-AI collaborations and human-produced (de novo) segmentations. Intriguingly, physicians worked 65% faster and with 32% less variation when editing an AI-produced segmentation compared to a manually produced one, even though they were unaware of which one they were editing. They also rated the quality of AI-drawn segmentations more highly than the human expert-drawn segmentations in this blinded study.
Going forward, the researchers plan to combine this work with AI models they designed previously that can identify “organs at risk” of receiving undesired radiation during cancer treatment (such as the heart) and thereby exclude them from radiotherapy. They are continuing to study how physicians interact with AI to ensure that AI-partnerships help, rather than harm, clinical practice, and are developing a second, independent segmentation algorithm that can verify both human and AI-drawn segmentations.
“The biggest translation gap in AI applications to medicine is the failure to study how to use AI to improve human clinicians, and vice versa,” said corresponding author Raymond Mak, MD, of the Brigham’s Department of Radiation Oncology. “We’re studying how to make human-AI partnerships and collaborations that result in better outcomes for patients. The benefits of this approach for patients include greater consistency in segmenting tumors and accelerated times to treatment. The clinician benefits include a reduction in mundane but difficult computer work, which can reduce burnout and increase the time they can spend with patients.”
“This study presents a novel evaluation strategy for AI models that emphasizes the importance of human-AI collaboration,” added co-author Hugo Aerts, PhD, of the Department of Radiation Oncology. “This is especially necessary because in silico (computer-modeled) evaluations can give different results than clinical evaluations. Our approach can help pave the way towards clinical deployment."
Latest General/Advanced Imaging News
- PET Scans Reveal Hidden Inflammation in Multiple Sclerosis Patients
- Artificial Intelligence Evaluates Cardiovascular Risk from CT Scans
- New AI Method Captures Uncertainty in Medical Images
- CT Coronary Angiography Reduces Need for Invasive Tests to Diagnose Coronary Artery Disease
- Novel Blood Test Could Reduce Need for PET Imaging of Patients with Alzheimer’s
- CT-Based Deep Learning Algorithm Accurately Differentiates Benign From Malignant Vertebral Fractures
- Minimally Invasive Procedure Could Help Patients Avoid Thyroid Surgery
- Self-Driving Mobile C-Arm Reduces Imaging Time during Surgery
- AR Application Turns Medical Scans Into Holograms for Assistance in Surgical Planning
- Imaging Technology Provides Ground-Breaking New Approach for Diagnosing and Treating Bowel Cancer
- CT Coronary Calcium Scoring Predicts Heart Attacks and Strokes
- AI Model Detects 90% of Lymphatic Cancer Cases from PET and CT Images
- Breakthrough Technology Revolutionizes Breast Imaging
- State-Of-The-Art System Enhances Accuracy of Image-Guided Diagnostic and Interventional Procedures
- Catheter-Based Device with New Cardiovascular Imaging Approach Offers Unprecedented View of Dangerous Plaques
- AI Model Draws Maps to Accurately Identify Tumors and Diseases in Medical Images
Channels
Radiography
view channel
Novel Breast Imaging System Proves As Effective As Mammography
Breast cancer remains the most frequently diagnosed cancer among women. It is projected that one in eight women will be diagnosed with breast cancer during her lifetime, and one in 42 women who turn 50... Read more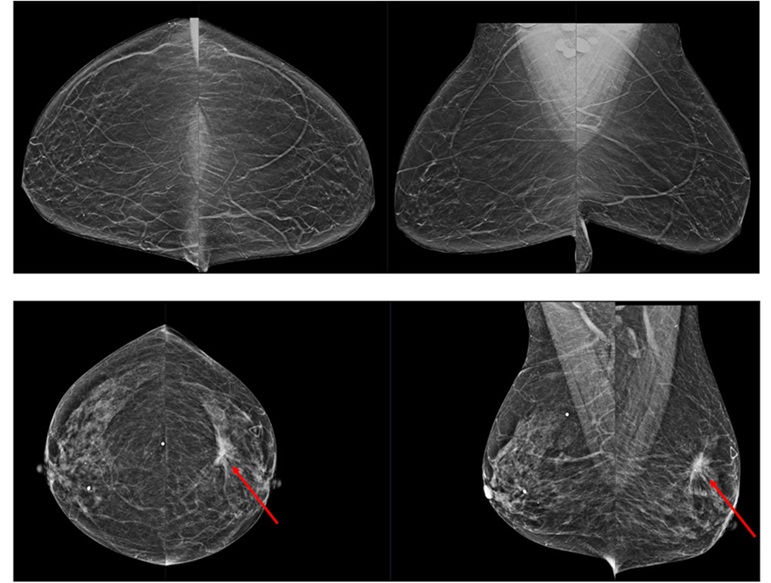
AI Assistance Improves Breast-Cancer Screening by Reducing False Positives
Radiologists typically detect one case of cancer for every 200 mammograms reviewed. However, these evaluations often result in false positives, leading to unnecessary patient recalls for additional testing,... Read moreMRI
view channel
Diamond Dust Could Offer New Contrast Agent Option for Future MRI Scans
Gadolinium, a heavy metal used for over three decades as a contrast agent in medical imaging, enhances the clarity of MRI scans by highlighting affected areas. Despite its utility, gadolinium not only... Read more.jpg)
Combining MRI with PSA Testing Improves Clinical Outcomes for Prostate Cancer Patients
Prostate cancer is a leading health concern globally, consistently being one of the most common types of cancer among men and a major cause of cancer-related deaths. In the United States, it is the most... Read more
PET/MRI Improves Diagnostic Accuracy for Prostate Cancer Patients
The Prostate Imaging Reporting and Data System (PI-RADS) is a five-point scale to assess potential prostate cancer in MR images. PI-RADS category 3 which offers an unclear suggestion of clinically significant... Read more
Next Generation MR-Guided Focused Ultrasound Ushers In Future of Incisionless Neurosurgery
Essential tremor, often called familial, idiopathic, or benign tremor, leads to uncontrollable shaking that significantly affects a person’s life. When traditional medications do not alleviate symptoms,... Read moreUltrasound
view channel.jpg)
Groundbreaking Technology Enables Precise, Automatic Measurement of Peripheral Blood Vessels
The current standard of care of using angiographic information is often inadequate for accurately assessing vessel size in the estimated 20 million people in the U.S. who suffer from peripheral vascular disease.... Read more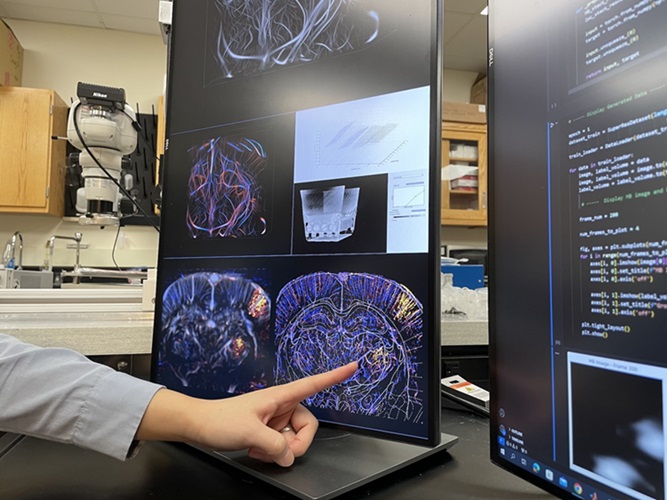
Deep Learning Advances Super-Resolution Ultrasound Imaging
Ultrasound localization microscopy (ULM) is an advanced imaging technique that offers high-resolution visualization of microvascular structures. It employs microbubbles, FDA-approved contrast agents, injected... Read more
Novel Ultrasound-Launched Targeted Nanoparticle Eliminates Biofilm and Bacterial Infection
Biofilms, formed by bacteria aggregating into dense communities for protection against harsh environmental conditions, are a significant contributor to various infectious diseases. Biofilms frequently... Read moreNuclear Medicine
view channel
New Imaging Technique Monitors Inflammation Disorders without Radiation Exposure
Imaging inflammation using traditional radiological techniques presents significant challenges, including radiation exposure, poor image quality, high costs, and invasive procedures. Now, new contrast... Read more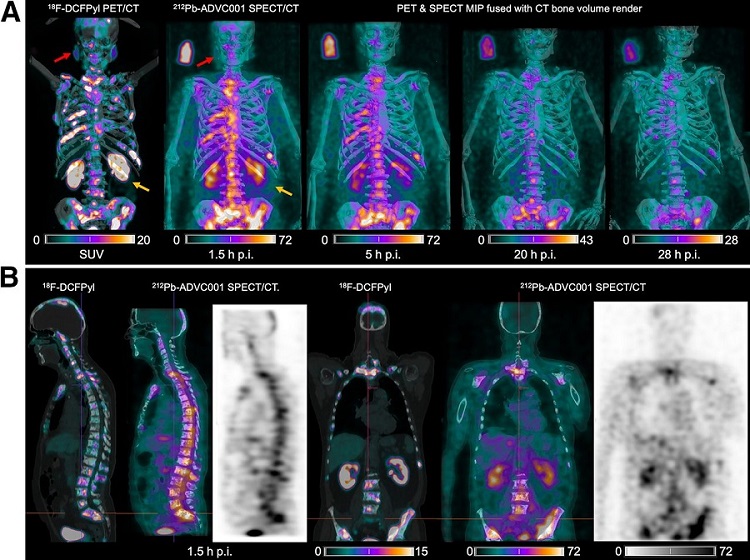
New SPECT/CT Technique Could Change Imaging Practices and Increase Patient Access
The development of lead-212 (212Pb)-PSMA–based targeted alpha therapy (TAT) is garnering significant interest in treating patients with metastatic castration-resistant prostate cancer. The imaging of 212Pb,... Read moreNew Radiotheranostic System Detects and Treats Ovarian Cancer Noninvasively
Ovarian cancer is the most lethal gynecological cancer, with less than a 30% five-year survival rate for those diagnosed in late stages. Despite surgery and platinum-based chemotherapy being the standard... Read more
AI System Automatically and Reliably Detects Cardiac Amyloidosis Using Scintigraphy Imaging
Cardiac amyloidosis, a condition characterized by the buildup of abnormal protein deposits (amyloids) in the heart muscle, severely affects heart function and can lead to heart failure or death without... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
Bayer and Google Partner on New AI Product for Radiologists
Medical imaging data comprises around 90% of all healthcare data, and it is a highly complex and rich clinical data modality and serves as a vital tool for diagnosing patients. Each year, billions of medical... Read more