Wearable Ultrasound Navigation System Could Improve Lumbar Puncture Accuracy
Posted on 26 Sep 2024
A lumbar puncture, or spinal tap, is a common medical procedure in which a hollow needle is inserted into the spinal canal to access cerebrospinal fluid that surrounds the brain and spinal cord. It is used to diagnose serious neurological conditions like meningitis or encephalitis and to administer anesthetics or chemotherapy. Physicians often refer to lumbar punctures as “blind bedside procedures” because they rely on feeling for the gap between two lumbar bones and then attempting to insert the needle in the correct location. This process can be particularly challenging in overweight or elderly patients. In some cases, the bony landmarks that guide the needle may not be easily felt, and in elderly patients, spinal degeneration adds to the difficulty. Multiple failed attempts can cause pain and increase the risk of blood contamination in the cerebrospinal fluid, potentially impacting the accuracy of diagnostic tests for conditions like meningitis, encephalitis, or subarachnoid hemorrhage. Now, researchers have developed an innovative ultrasound navigation system designed to provide accurate, real-time guidance for needle insertion during lumbar punctures.
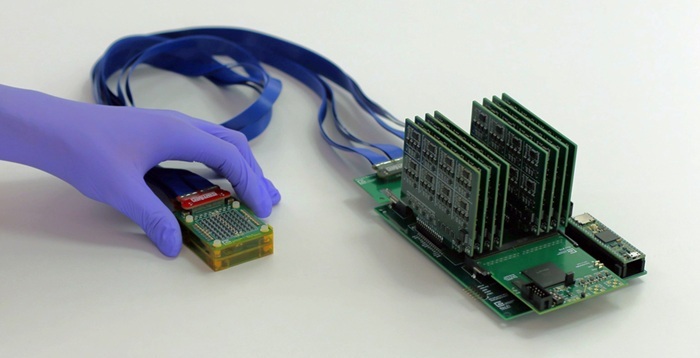
The system, created by a team from Johns Hopkins University (Baltimore, MD, USA) and Clear Guide Medical (Baltimore, MD, USA), incorporates three key components to enhance needle accuracy: a cell phone-sized ultrasound scanner that can be attached to the patient’s skin along the lower spine, imaging algorithms that estimate bone surfaces, and an augmented reality display that superimposes a digital guide for needle insertion onto the view of the patient’s spine. This research builds on earlier findings, which demonstrated that the ultrasound scanner significantly improved visibility of the lumbar gap.
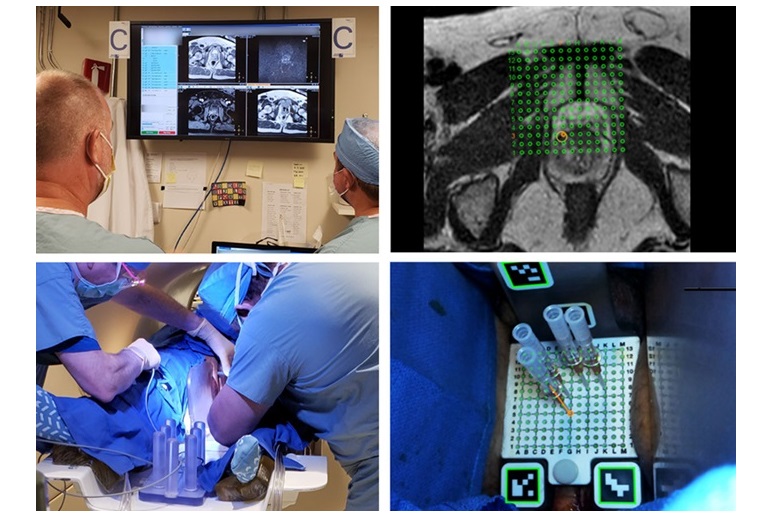
Published in IEEE Transactions on Medical Robotics and Bionics, the current study evaluated the overall accuracy of the navigation system, comparing two augmented reality methods: one using a tablet with camera-based tracking and the other using a head-mounted display similar to goggles, with optical-based tracking. Both approaches successfully guided needle placement, with an accuracy of 2.83 mm for the tablet and 2.76 mm for the head-mounted display, both within the 4 mm benchmark commonly used in spinal surgeries for needle placement precision.
The researchers also conducted a preliminary user study to gather feedback and compare the two augmented reality systems. Sixteen users completed eight sets of lumbar punctures using a realistic anatomical model (phantom) of the spine. The success rate for first-time needle insertions was 89%. On average, users required 1.14 attempts with the head-mounted display and 1.12 attempts with the tablet system to reach the target, defined as a rubber tube embedded in the phantom vertebrae canal. In comparison, other studies have shown that traditional methods using palpation often require multiple attempts. One study found that first-time needle insertion was successful in 71% of patients, while nearly 30% needed multiple attempts or failed entirely. Since completing this study, the researchers have replaced their needle tracking method using QR and other codes with artificial intelligence, simplifying the system for clinical use.
“This wearable ultrasound navigation system has several advantages over other imaging navigation methods,” said Peter Kazanzides, Ph.D., a research professor in computer science at Johns Hopkins University. “A pre-operative computed tomography scan would not be necessary, and clinicians would be able to use both hands to control the needle when using the navigation system. They currently use one hand to hold and guide the imaging probe and the other hand to insert the needle.”
“Our team at Hopkins is very excited about the direction we’re taking toward wearable ultrasound devices. Our device can capture the complex shape of lumbar bones without the shadows often seen in typical ultrasound scanners and it has the flexibility to adapt to motion,” added Emad Boctor, Ph.D., associate research professor at Johns Hopkins University and co-founder of Clear Guide Medical.
Related Links:
Johns Hopkins University
Clear Guide Medical