Brain Radiotherapy May Not Be Necessary for Patients with Lung Cancer Metastases
By MedImaging International staff writers
Posted on 13 Sep 2016
The results of a phase 3 randomized trial have revealed that there was no beneficial effect in terms of survival rate or quality of life, for patients who underwent whole brain radiotherapy, compared to those who received only steroid treatment and supportive care.Posted on 13 Sep 2016
The results indicate that patients suffering from a common form of lung cancer, with brain metastases may not need to undergo whole brain radiotherapy that can result in substantial harmful side effects such as nausea, fatigue and neurotoxicity.
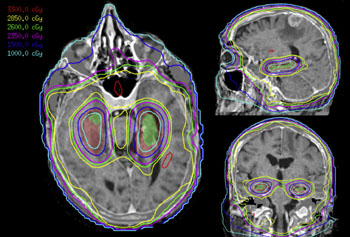
Image: The image displays an example of Hippocampal-sparing whole brain radiotherapy (Photo courtesy of ResearchGate).
The research was published in the August 2016 online edition of the journal The Lancet. The researchers found that whole brain radiotherapy could be beneficial in patients below the age of 60, but should not be used for standard treatment of most patients suffering from Non-Small Cell Lung Cancer (NSCLC) with brain metastases.
According to the researchers 11% of the participants randomized to whole-brain radiotherapy were too ill or died before they could receive the treatment. The assessment of quality-of-life was also limited, in order not to overburden the seriously ill patients.
Study author, Dr Paula Mulvenna, consultant clinical oncologist at the Newcastle Hospitals NHS Foundation Trust (Newcastle upon Tyne, UK), said, "Whole brain radiotherapy was widely adopted into clinical practice based on the assumption it improves tumor control in patients with brain metastases. But in our lung cancer clinics, we were not seeing the improvements we had hoped for in our patients. Survival times are poor and have hardly changed since the 1980s. What's more, the technique's toxicity can be substantial and it can damage cognitive function."
Related Links:
Newcastle Hospitals NHS Foundation Trust














