Personalized Shields Reduce Radiotherapy Tissue Injury
By MedImaging International staff writers
Posted on 12 May 2021
3D-printed devices derived from CT images can shield healthy structures in the gastrointestinal (GI) tract during radiation therapy (RT) procedures, according to a new study.Posted on 12 May 2021
Developed at Brigham and Women's Hospital (BWH; Boston, AM, USA), the Massachusetts Institute of Technology (MIT; Cambridge, MA, USA), Massachusetts General Hospital (MGH; Boston, USA), and other institutions, the personalized shields were designed and contoured on diagnostic CT scans using the open-source 3D Slicer software app. The contours were then generated into 3D models, and the personalized radioprotective shields were 3D-printed with high atomic number materials to block gamma and x-rays and reduce radiation backscatter.
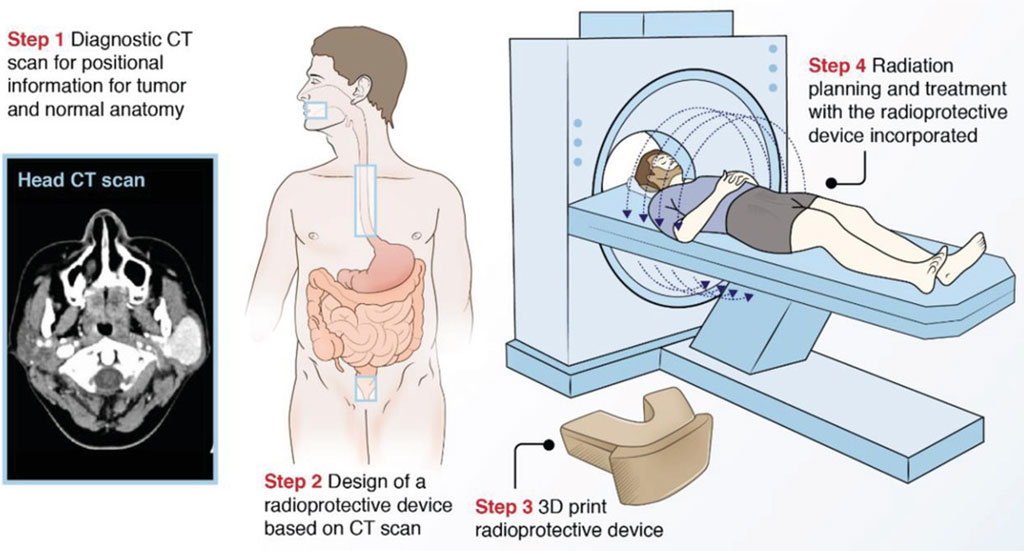
Image: Clinical workflow for integrating personalized radioprotectant devices in RT (Photo courtesy of BWH)
In initial testing on rats and pigs, the researchers found that the devices could protect healthy tissue in the mouth and rectum in rats and were feasible and reproducible in pigs. In human simulation studies, dosimetric modeling showed a 30% dose reduction to the normal buccal mucosa in maxillofacial cancer patients, and a 15.2% dose reduction in the rectum for prostate cancer patients. They also suggest that the new shields are more cost-effective than a hydrogel rectal spacer. The study was published on April 27, 2021, in Advanced Science.
“Personalized 3D‐printed radioprotectant devices may have great potential to reduce radiation toxicity in clinical settings where radiation is used, including neoadjuvant and adjuvant therapy, curative treatment, and palliative treatments,” concluded lead author James Byrne, PhD, of BWH, and colleagues. “This personalized approach could be applicable to a variety of cancers that respond to radiation therapy, including head and neck, lung, prostate, anal, skin, and gynecological cancers, sarcomas, and lymphomas.”
Most cancer patients undergoing RT will develop colateral tissue injury as a result of treatment. The toxicities are dependent upon the location of treatment, with the most common toxicities involving the oral cavity and gastrointestinal (GI) tract in the forms of oral mucositis, esophagitis, and proctitis. This injury may lead to severe morbidity and, ultimately, treatment breaks or discontinuation that adversely impact tumor cure rates.
Related Links:
Brigham and Women's Hospital
Massachusetts Institute of Technology
Massachusetts General Hospital













