SBRT Can Safely Treat Multiple Metastatic Tumors
By MedImaging International staff writers
Posted on 03 May 2021
A new study suggests that stereotactic body radiotherapy (SBRT) can be used effectively for treating patients with multiple metastases. Posted on 03 May 2021
Researchers at Fox Chase Cancer Center (Philadelphia, PA, USA), the University of Chicago Comprehensive Cancer Center (IL, USA), the University of Michigan (U-M; Ann Arbor, USA), and other institutions conducted a study involving 39 patients (mean age, 63.1; 20 57.1% male; 85.7% White) with breast, prostate, or non-small cell lung cancer (NSCLC), with at least three metastases or two metastases in close proximity. In all, 34.3% had breast cancer, 28.6% had NSCLC, and 37.1% had prostate cancer.
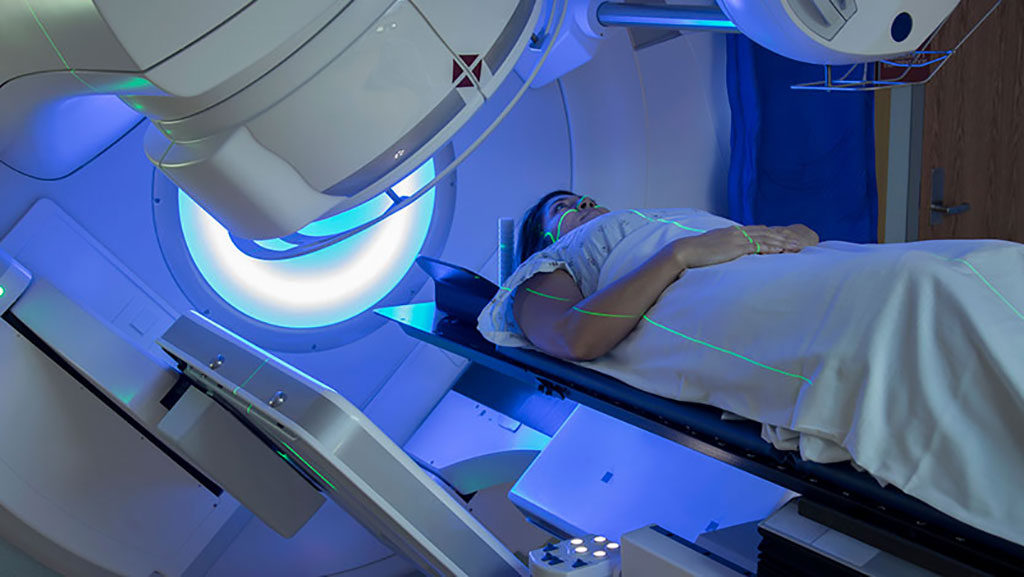
Image: SBRT can be used to treat multiple metastases (Photo courtesy of University of Chicago)
Dose levels were considered safe if dose-limiting toxicity (DLT) levels were observed in no more than one of six patients per location; otherwise, the dose at that location would be de-escalated. The primary end point was DLT related to SBRT within 180 days of treatment. Results of the phase one study showed that at the end of the trial period, primary six-month DLT endpoint was 0%, indicating that the approach was safe enough to begin phase 2/3 clinical trials in a larger group of patients. The study was published on April 22, 2021, in JAMA Oncology.
“People have been saying for years that if we used SBRT in patients with multiple, limited metastases, we could potentially cure more patients. But it's very technically complicated to do so,” said lead author Professor Steven Chmura, MD, PhD, of the University of Chicago. “The greatest challenge was having a whole team of people come together and figure out how we could define the doses and manage the real-time quality assurance to make sure every single patient had the best treatment possible.”
SBRT is emerging as an attractive option for treating cancers in the lung, head and neck, prostate, liver and other disease sites, with the objective of increasing local control of the target lesion while limiting dose to nearby critical structures and normal tissue. Requirements include precise localization of the target lesion in the treatment planning process; accounting for tumor motion due to respiration or other changes in the body; highly conformal dose distribution to the target volume, including a steep dose gradient to minimize radiation to surrounding healthy tissue; and image-guidance at the time of dose delivery for verification and adjustment of the target localization.
Related Links:
Fox Chase Cancer Center
University of Chicago Comprehensive Cancer Center
University of Michigan














