Radiation Detector Plate Improves Cancer Radiotherapy
By MedImaging International staff writers
Posted on 14 Mar 2016
A prototype detector plate placed in the radiation path (before the X-ray beam hits the patient) records a real-time map of the intensity of the radiotherapy (RT) beams.Posted on 14 Mar 2016
Developed by researchers at the University of Wollongong (UOW; Australia), the MagicPlate-512 (MP512) detector consists of a silicon monolithic diode array sandwiched between plastic sheets less than 1-mm thick, which measures the radiation dose during treatment with millisecond by millisecond precision. A proprietary algorithm determines the actual dose reaching the patient, based on the measured intensity of the X-ray distribution in the beam. This can then be compared to the planned dose; if a mismatch exists, the RT could be automatically and immediately stopped.
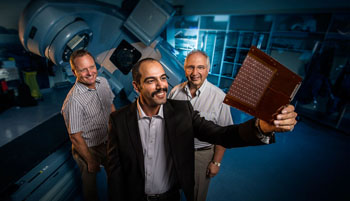
Image: Ziyad Alrowaili holds up the MP512 with Dr. Martin Carolan and Prof, Anatoly Rozenfeld (Photo courtesy of UOW).
The MP512 detector is wire bonded on a printed circuit board 0.5 mm thick and covered by a thin layer of resin to preserve it from moisture and chemical contamination, and to protect the bonding wires. The array contains 512 0.5×0.5 mm2 pixels with a pitch of 2 mm. It has been tested and validated in a simulated environment using different X-ray beam energies that are commonly used to treat cancer patients. The researchers found the plate did not interfere with the quality of RT and accurately recorded in real-time the transmission of the radiation beam.
“Current procedures typically involve a test on a plastic dummy before the patient is treated, to verify the equipment is delivering the dose according to the oncologist’s treatment plan calculations,” said Ziyad Alrowaili, MSc, who developed the plate as part of his PhD thesis. “This is an intensive task and an additional workload for the medical physicist. And despite the high levels of quality assurance, the clinician can’t routinely measure the dose accuracy directly during the patient treatment delivery and independently of the linear accelerator settings.”
“A single patient treatment plan may contain thousands of parameters defining the variables involved, and this complexity makes it imperative that processes are in place to check and verify the X-ray equipment delivers the dose accurately,” added Martin Carolan, MD, director of radiation oncology medical physics at Illawarra Shoalhaven Local Health District (ISLHD; Australia). “There are many layers of safeguards already in place to reduce the risk to the patient, but the concept of measuring the radiation dose distribution every day as it is delivered to the patient is elegant and appealing.”
Related Links:
University of Wollongong
Illawarra Shoalhaven Local Health District














