New Cardiac MRI Strategy Guides Ablation Procedures for Complex Tachycardias
Posted on 09 Oct 2024
Ablation procedures use energy—typically heat or cold—to target and eliminate small areas of heart tissue that trigger abnormal cardiac arrhythmias, restoring normal heart rhythm. This approach is often applied to treat ventricular tachycardias that result from scarred regions following a myocardial infarction. A new strategy has now been proposed to guide ablation procedures for patients with complex tachycardias. It involves preoperative planning based on a cardiac magnetic resonance (CMR) imaging technique that avoids the biases associated with conventional image analysis.
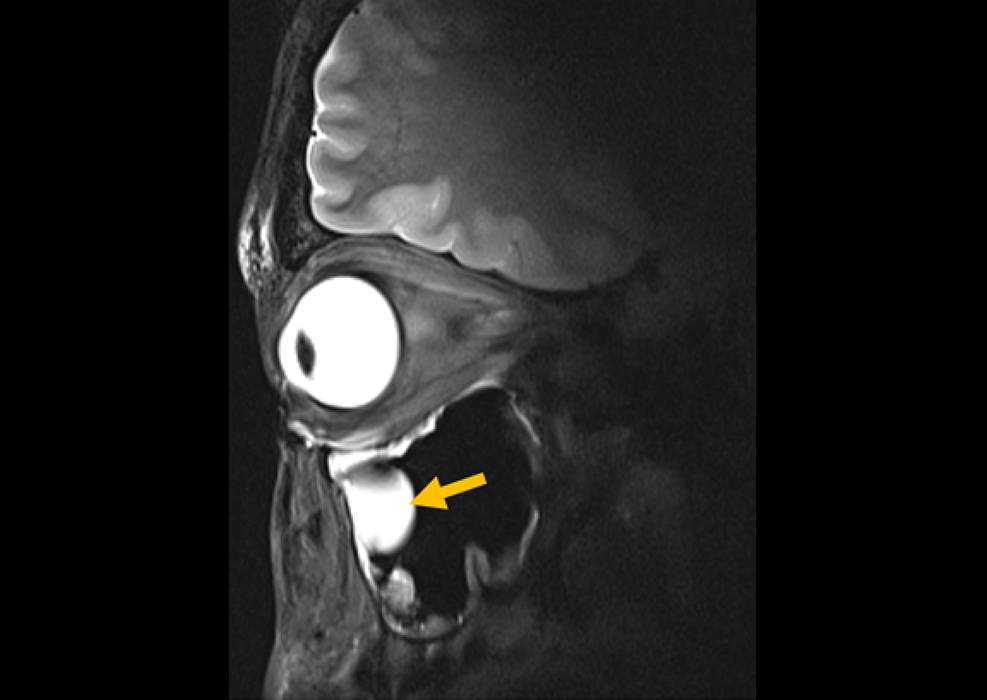
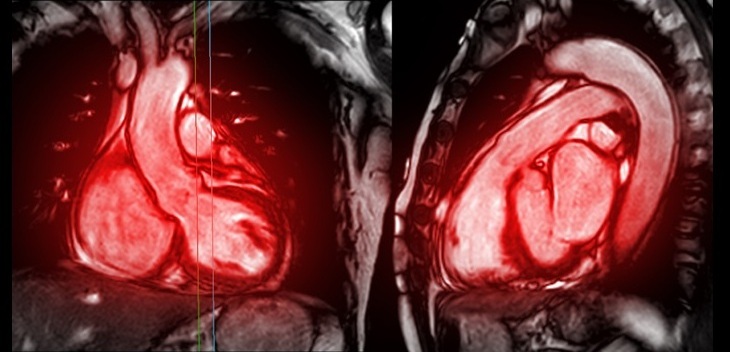
A multicenter study, led by the National Centre for Cardiovascular Research (Madrid, Spain), has described and validated this novel approach that utilizes advanced CMR image processing methods to identify the regions that sustain ventricular tachycardia in areas affected by postinfarction scarring. The method systematically processes the images, bypassing the biases that can occur when CMR imaging parameters are selected manually. This approach enhances sensitivity in detecting the regions responsible for these arrhythmias. Moreover, it supports preoperative planning by enabling operators to accurately locate these areas before the ablation procedure begins. Published in the journal Europace, the study employed a swine model of myocardial infarction to explore how variability in image processing parameters can obstruct accurate detection of cardiac tissue circuits that drive complex ventricular tachycardias.
Using this animal model, the researchers devised a strategy to overcome this issue. The method was later validated in patients through a multicenter study conducted from 2013 to 2022, involving leading national and international experts. The new image-processing technique simplifies the visualization of cardiac tissue at varying depths, allowing for an objective evaluation of the cardiac wall. It eliminates operator bias in the selection of imaging parameters, enabling accurate detection of the myocardial regions responsible for postinfarction ventricular tachycardia. The streamlined planning of ablation procedures with this method is especially beneficial for patients in whom conventional invasive catheter mapping is contraindicated, as it carries the risk of inducing more severe tachycardias and circulatory collapse. Instead of these risky procedures, the new approach uses pre-ablation cardiac imaging to identify target areas, reducing risk while maintaining the procedure's efficacy.
“The study helps to fill gaps in the integration of imaging data during the planning of ablation procedures for ventricular tachycardia,” said study coordinator David Filgueiras. “By allowing personalized and unbiassed pre-procedure planning, the new method can reduce procedure times and complications, which is especially useful in patients with severe and poorly tolerated episodes. The strategy achieves a high success rate without the need for invasive catheter mapping procedures, which in any case are frequently contraindicated by the patient’s clinical condition.”
“The conventional strategies used to characterize regions causing postinfarction ventricular tachycardia require invasive catheter mapping, a risky process that increases the time needed for the ablation procedure,” added study coauthor, Julián Pérez Villacastín. “The new approach identifies the culprit areas during preoperative planning and offers a standardized and unbiased method, allowing medical professionals in different centers to carry out ablations in a more controlled manner in highly complex patients.”
Related Links:
National Centre for Cardiovascular Research








 Guided Devices.jpg)