MRI Improves Diagnosis and Treatment of Prostate Cancer
Posted on 28 Mar 2024
Prostate cancer ranks as a leading cancer type among men. Suspected prostate cancer cases are usually identified through a prostate-specific antigen (PSA) test or a rectal examination. If cancer is suspected, a systematic biopsy is typically performed, involving the collection of 10 to 12 random tissue samples with the assistance of ultrasound for laboratory analysis. Despite the use of ultrasound, this method is invasive and carries the risk of missing cancerous areas, along with possible side effects like bleeding, difficulty urinating, and infection. semen or urine, difficulty urinating, and infection including potentially deadly sepsis in rare cases. Now, two multi-center studies using magnetic resonance imaging (MRI) are playing a major role in changing the diagnostic pathway for prostate cancer.
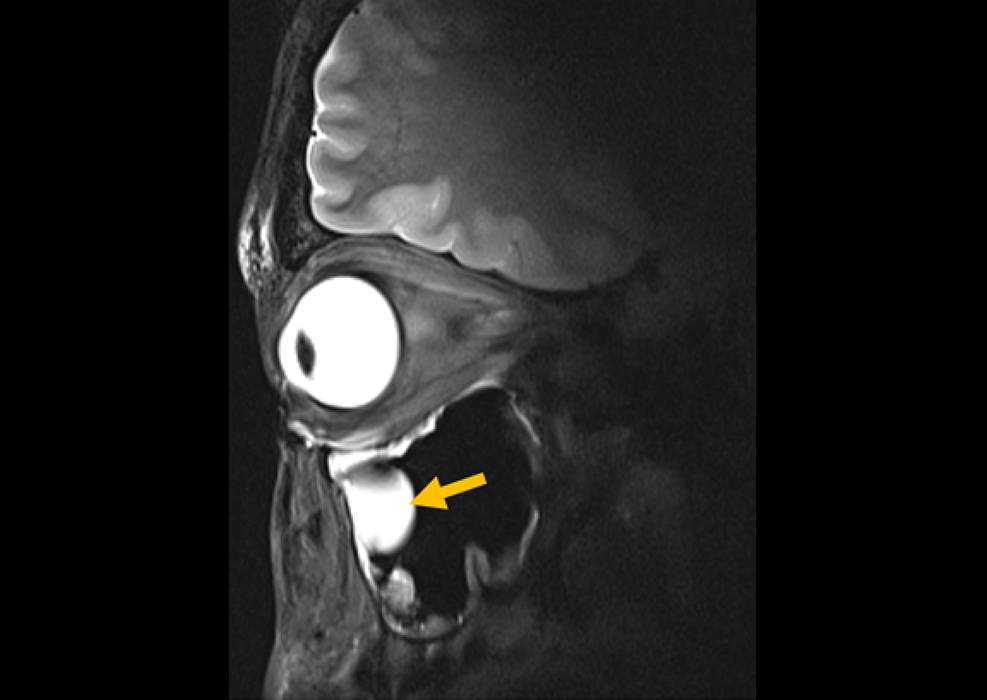
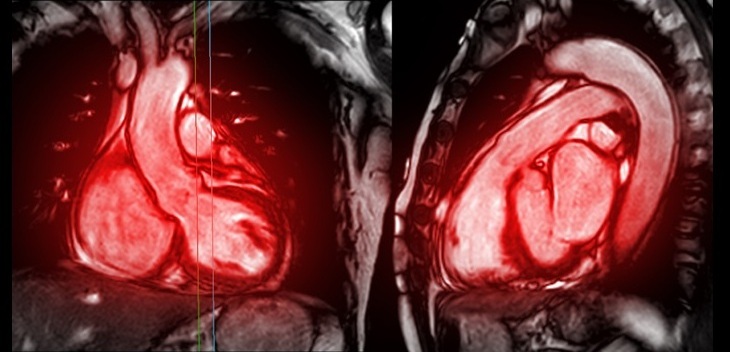
MRI employs strong magnetic fields and radiofrequency waves to produce detailed cross-sectional images that can reveal cancers other methods may overlook, identifying the cancer's size, location, and spread. Both multi-center studies led by Hamilton Health Sciences (HHS, Ontario, Canada) used MRI to improve the diagnosis and treatment for men going through a prostate cancer diagnosis. The ASIST study (2010-2015) examined whether MRI detected additional high-risk cancers when used along with the standard-of-care systematic biopsy. The positive results from the ASIST study led to the second PRECISE study (2015-2017) to examine whether MRI could determine the need for a biopsy.

The ASIST trial, involving 273 participants, investigated whether MRI, alongside standard systematic biopsies guided by ultrasound, could detect prostate cancer at a risk of becoming aggressive at a different rate than when using an ultrasound-guided biopsy process alone. The study revealed MRI’s potential for helping to distinguish between patients who could benefit from aggressive treatment and those who are more ideal for regular monitoring, as many prostate cancers are not aggressive. The PRECISE trial, with 453 male participants, evaluated the necessity of biopsies in all suspected prostate cancer cases. It demonstrated that MRI could target two to four specific tissue samples from areas appearing cancerous, as opposed to the traditional method of collecting 10 to 12 random samples. This targeted approach not only reduces invasiveness but also minimizes recovery time and side effects, enhancing the detection of high-risk diseases while helping some patients avoid unnecessary radical treatments. In the PRECISE study, 37% of patients (79 individuals) were spared a biopsy after an MRI assessment indicated it was unnecessary.
“By providing MRI first, only those men who need a biopsy receive it,” said HHS researcher Dr. Gregory Pond who is the lead statistician and co-investigator for the two clinical trials. “It’s basically a win-win because we’re picking up the same amount of cancers as the systematic biopsy using ultrasound, but by doing the MRI first it’s safer, less invasive and more cost effective for the health-care system. Both studies have absolutely changed practice, and will continue to change practice worldwide.”
Related Links:
Hamilton Health Sciences