Many Stroke Patients Undergo Possible Redundant MRI and CT Neuromaging
By MedImaging International staff writers
Posted on 27 Mar 2012
Neuroimaging for stroke patients may be unnecessarily expensive and redundant, contributing to rising costs for stroke care, according to recent research. Posted on 27 Mar 2012
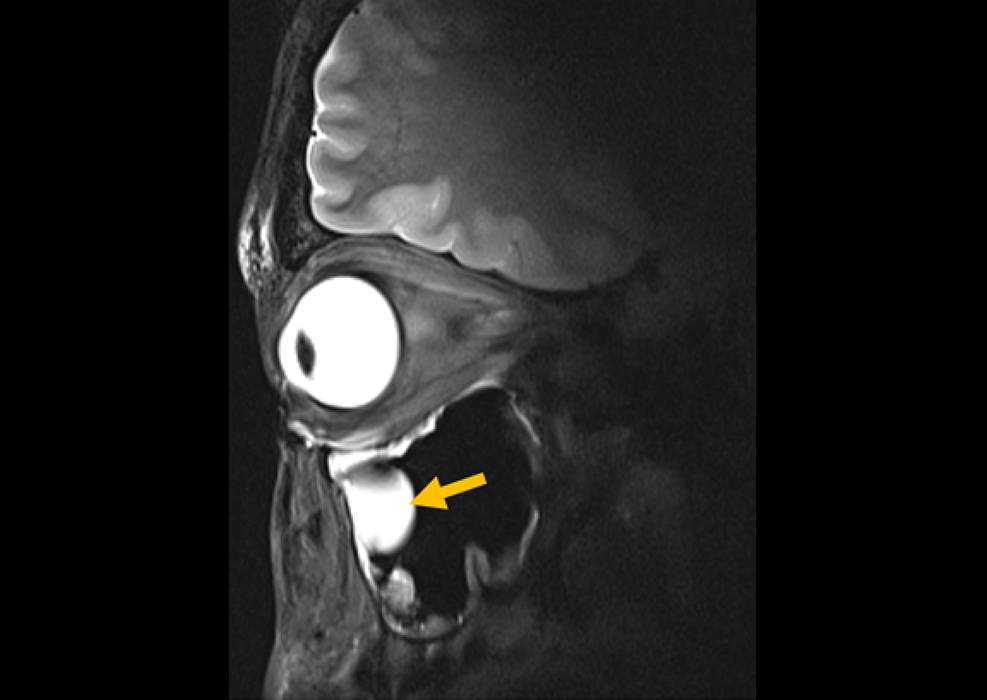
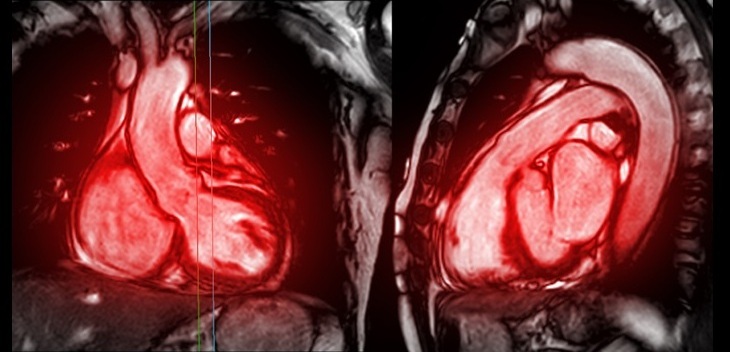
The research, published in the February 2012 issue of the journal Annals of Neurology, found that 95% of stroke patients who received magnetic resonance imaging (MRI) also had a computed tomography (CT) scan. “Compared to CT, MRI is a more accurate test for stroke,” said James F. Burke, MD, lead author of the study and a clinical lecturer in the University of Michigan Medical School’s (Ann Arbor, USA) department of neurology. “But our results showed that MRI is not replacing CT as the primary stroke neuroimaging study--instead, patients are getting both. Minimizing the use of multiple studies could be a viable strategy to reduce costs.”
The costs of inpatient stroke care have climbed by 42% between 1997 and 2007, an increase of USD 3,800 per case, Dr. Burke and his University of Michigan found. Neuroimaging--MRIs and CTs--were the largest driver of costs.
Diagnostic imaging has been the fastest growing component of total hospital costs, increasing 213% t from 1999 to 2007. “The data show that neuroimaging practices in stroke are neither standardized nor efficient,” Dr. Burke noted. “This represents an area where we have an opportunity to substantially reduce the cost of care without adversely affecting the quality of care.”
Dr. Burke’s research spurred an accompanying editorial in the same issue of the journal, written by the journal editors S. Clairborne Johnson, MD, PhD, and Stephen L. Hauser, MD. “The issue of duplicative imaging in stroke is just one example of wasteful care,” the editors wrote. “Quite simply, it is very easy to order more test and to treat with more expensive therapies . “We should track waste as another measure of quality care...The failure to find a political solution to rising healthcare costs only increases our responsibility to become leaders and not victims.”
Burke and his coauthors studied patients diagnosed with stroke from 1999 to 2008 in 11 states, studying 624,842 patients. They found wide geographic variation for the use of MRI, but overall the use of MRI jumped dramatically. “There currently is not evidence-based guidelines that preferentially recommend either MRIs or CT,” Dr. Burke remarked. “Understanding trends like these presented in this study are essential to determining efficient and consistent neuroimaging strategies.”
Related Links:
University of Michigan Medical School