Revising MR Enterography Protocol May Reduce Costs, Complexity While Maintaining Effective Crohn’s Disease Diagnosis
By MedImaging International staff writers
Posted on 18 Jul 2011
A new study has found that magnetic resonance enterography (MRE) without the use of an antiperistaltic agent was as effective as computed tomography enterography (CTE) in determining the presence of Crohn’s disease. Moreover, MRE reduces the patient’s exposure to ionizing radiation. Posted on 18 Jul 2011
The study was published online in June 2011 advance of print in the European Journal of Radiology. Lead author David J. Grand, MD, director of the body MRI program at Rhode Island Hospital (Providence, USA) found that MR enterography without anti-peristaltic agents results in high diagnostic confidence for the presence or absence of Crohn’s disease when compared to CT enterography. To limit exposure to ionizing radiation in young patients, MR enterography may be considered a first-line study for the assessment of known or suspected Crohn’s disease.
“This is an important discovery in the diagnostic process for Crohn’s disease,” said Dr. Grand. “This information will help us to develop safer approaches toward testing, helping to lower patients’ exposure to radiation, while still maintaining the integrity of diagnosis.”
The study included 26 patients to be tested for known or suspected Crohn’s disease. The patients underwent CTE immediately followed by MRE without the use of an antiperistaltic agent. Two fellowship-trained abdominal imagers evaluated each study on a 10-point scale for exam quality, level of diagnostic confidence and presence of Crohn’s disease. The CTE and MRE images were reviewed in random order with at least two weeks separating interpretation of the test results of a single patient.
Whereas the quality of the MRE scans was ranked slightly lower than the quality of the CTEs, both tests were judged with similarly high rankings for level of confidence in interpretation.
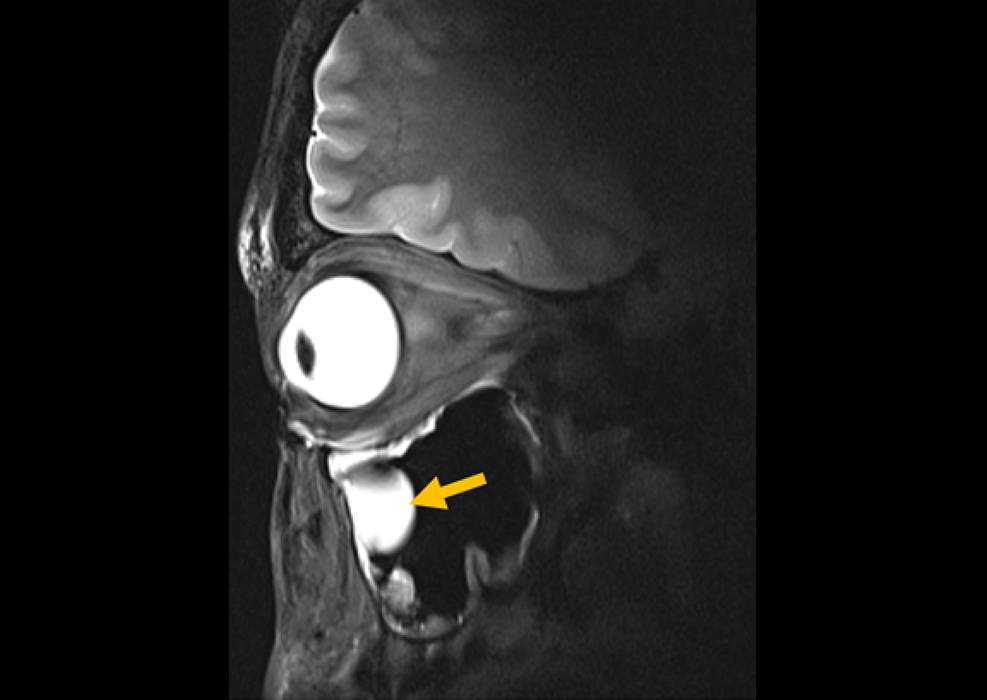
Crohn’s disease, a form of inflammatory bowel disease (IBD), is a chronic, relapsing, autoimmune disorder that may affect any portion of the gastrointestinal tract, most typically the terminal ileum. The incidence of IBD has increased 31 percent in the US since 1991. Cross-sectional imaging is currently a mainstay of evaluation of patients with Crohn’s disease due to its ability to assess the entire bowel and extra-luminal complications including fistula and abscess. However, MRE has shown excellent effectiveness both in detection of Crohn’s disease as well as in differentiation of active from chronic small bowel changes.
While CTE has proven to be an effective tool in diagnosing Crohn’s disease, the radiation dose the patient receives is up to five times higher than that of small-bowel follow through, the modality it has largely replaced. In one population-based study, diagnostic imaging exams exposed the majority of Crohn’s patients to an additional annual radiation does equal to the annual background radiation in the United States, while a subset of patients received up to 11 times this additional dosage.
MRE can eliminate ionizing radiation exposure in the population of patients who frequently present while young and undergo multiple imaging exams throughout their lives.
Moreover, all published literature to date has used a pharmacologic antiperistaltic agent to minimize motion artifacts. While the agents may improve subjective image quality, their use has not been shown to be diagnostically necessary and administration complicates exam protocol and increases expense. This study demonstrates, according to the researcher, that the antiperistaltic agents may not be necessary, and suggests a simplified protocol of MRE that maintains diagnostic yield while decreasing complexity and expense.
Related Links:
Rhode Island Hospital