Avoiding Overdiagnosis in Geriatric Imaging
By MedImaging International staff writers
Posted on 05 Apr 2011
Imaging geriatric patients will become more common as the global population ages. Radiologists are now learning about not only the most common pathologies among the elderly but also how to avoid potential pitfalls that could lead to overtreatment. Posted on 05 Apr 2011
Ultimately, the ability to differentiate between the elderly presenting with the normal signs of aging and those who need more care will help to avoid an even greater drain on healthcare systems, radiology experts argued at the annual meeting of the European Congress of Radiology (ECR), held in March 2011 in Vienna, Austria.
In geriatric patients the coexistence of several diseases, and the prevalence of involutional and degenerative characteristics combined with physical and cognitive problems represent "the norm,” thus the importance of differentiating the healthy elderly from those in need of treatment, Prof. Giuseppe Guglielmi, from Foggia (Italy) explained. "The question is how to be aware of the potential and limits of diagnostic imaging and its applications in geriatric patients,” he said.
Bone and joint disorders are common in the elderly population and the loss of mobility and physical independence resulting from fractures, osteoarthritis, and osteoporosis can be devastating, both physically and psychologically.
The most common complaints and conditions pertaining to the geriatric population must be known to radiologists, who will see more and more geriatric patients in the future, pointed out Prof. Anne Cotton, from Lille (France). "Radiologists must also be aware of some misleading radiological presentations typically occurring in this population, such as unrecognized fractures, missed infection or malignant conditions, and myeloma revealed by osteoporotic vertebral collapses,” she said.
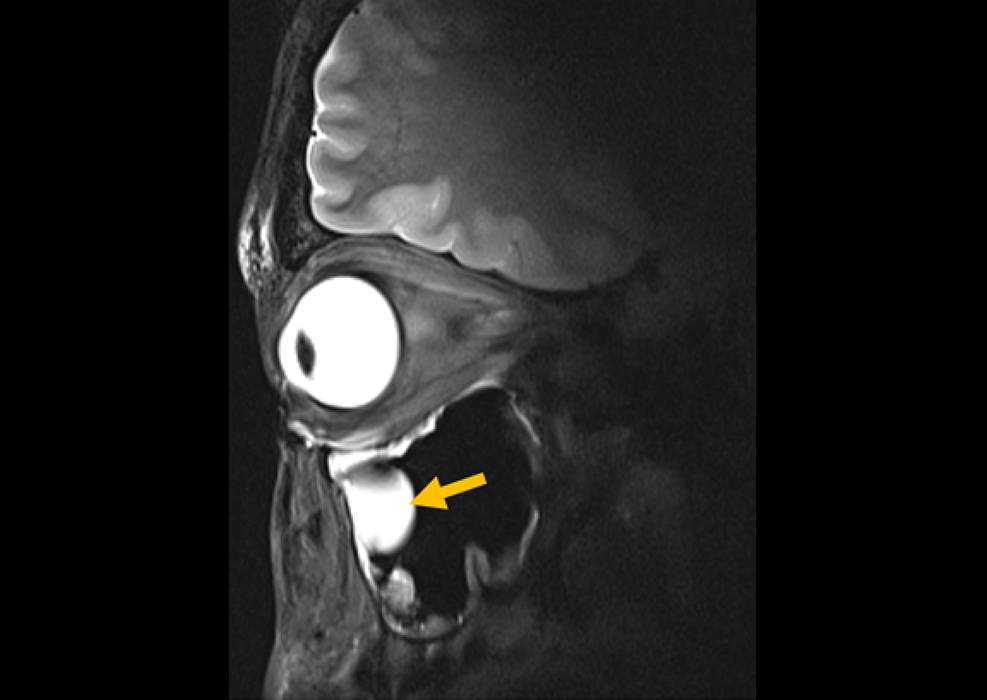
In the brain, severe incidental white matter lesions (WMLs) and incidental cerebral microbleeds (MBs) are tied to known cardiovascular risk factors, and while the concurrent impact may be subtle in terms of cognition, they carry a poor prognosis in the long run. The same is true for silent cerebral infarcts, which increase the risk of dementia. Neurodegenerative changes also occur well before the onset of clinical signs of dementia.
The role of functional magnetic resonance imaging (MRI) and positron emission tomography with fluorodexyglucose (FDG-PET) in predicting cognitive decline in genetically predisposed individuals has been shown. In particular, PET studies employing amyloid tracers have recently demonstrated abnormal binding in a significant proportion of cognitively elderly patients, suggesting that these subjects are at risk of developing Alzheimer's disease--the pace of which is currently undetermined.
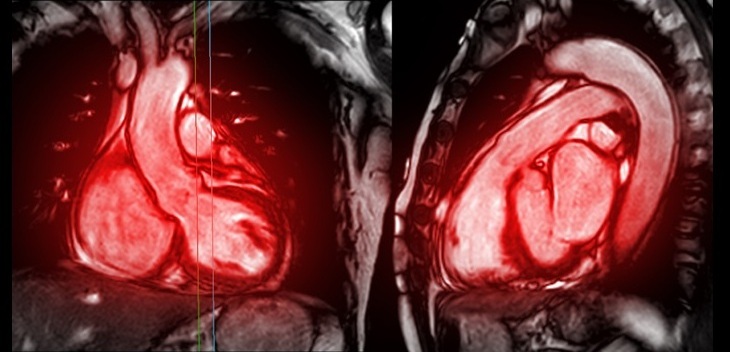
Finally, most complications of cardiovascular disease, including myocardial infarction, stroke, congestive heart failure, atrial fibrillation, and cardiovascular death, mostly occur in individuals who are 65 or older. A number of imaging modalities, such as ultrasound, PET/CT, and high-resolution black-blood MRI have emerged that can be used to evaluate the composition and morphology of atherosclerotic plaques. The ECR session included debates on the reversibility of atherosclerosis, by providing an update on the latest imaging studies examining the effects of antiatherosclerotic drugs on plaque regression and progression.
The European Congress of Radiology is the annual meeting of the European Society of Radiology (ESR).
Related Links:
European Society of Radiology