Mathematical Model Devised for Curing More Cervical Cancer Patients
By MedImaging International staff writers
Posted on 24 Feb 2010
Cervical cancer is curable when detected early. But in one-third of cases, the tumor responds poorly to therapy or recurs later, when cure is much less likely. A more rapid identification of nonresponding tumors may be possible using a new mathematical model.Posted on 24 Feb 2010
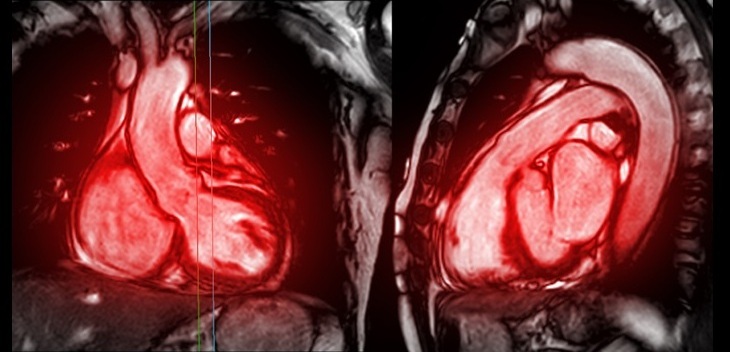
The model, devised by researchers at the Ohio State University Comprehensive Cancer Center-Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC-James; Columbus, USA), utilizes information from magnetic resonance imaging (MRI) scans taken before and during therapy to monitor changes in tumor size. That information is plugged into the model to predict whether a specific case is responding well to treatment. If not, the patient can be changed to a more aggressive or experimental therapy midway through treatment, something not possible now.
The study, published in the February 1, 2010, issue of the journal Cancer Research, uses MRI scans and outcome information from 80 cervical cancer patients receiving a standard course of radiation therapy designed to cure their cancer. "The model enables us to better interpret clinical data and predict treatment outcomes for individual patients,” said lead investigator Dr. Jian Z. Wang, assistant professor of radiation medicine and a radiation physicist at the OSUCCC-James. "The outcome predictions presented in this paper were solely based on changes in tumor volume as derived from MRI scans, which can be easily accessed even in community hospitals. The model is very robust and can provide a prediction accuracy of 90% for local tumor control and recurrence.”
An advantage of the new model, according to first author Zhibin Huang, is its use of MRI data to estimate three factors that play key roles in tumor shrinkage and that vary from patient to patient--the proportion of tumor cells that survive radiation exposure, the speed at which the body removes dead cells from the tumor, and the growth rate of surviving tumor cells.
The model is applicable to all cervical cancer patients, and the investigators are developing a model that can be applied to other cancer sites, according to Dr. Wang. Co-author Dr. Nina A. Mayr, professor of radiation medicine at Ohio State, noted that the size of cervical tumors is currently estimated by touch, or palpation, which is frequently imprecise. Furthermore, shrinkage of a tumor may not be apparent until months after therapy has ended.
Other clinical factors currently used to predict a tumor's response to therapy include the tumor's stage, whether it has invaded neighboring lymph nodes and its microscopic appearance. "Our kinetic model helps us understand the underlying biological mechanisms of the rather complicated living tissue that is a tumor,” Dr. Wang concluded. "It enables us to better interpret clinical data and predict treatment outcomes, which is critical for identifying the most effective therapy for personalized medicine.”
Related Links:
Ohio State University Comprehensive Cancer Center-Arthur G. James Cancer Hospital