Imaging Biopsy Needle Makes Brain Surgery Safer
By MedImaging International staff writers
Posted on 09 Jan 2019
A novel biopsy needle that contains a miniaturized optical coherence tomography (OCT) probe can help surgeons identify and avoid blood vessels during brain surgery.Posted on 09 Jan 2019
Developed by researchers at the University of Adelaide (UA; Australia), Sir Charles Gairdner Hospital (Nedlands, Australia), and other institutions, the miniaturized fiber-optic OCT probe is integrated into a standard commercial neurosurgical stereotactic biopsy needle. Brain tissue is illuminated using near-infrared (NIR) light, and the backscattered optical signal from different depths is extracted using low-coherence interferometry and reconstructed into a structural image of the tissue, typically at a spatial resolution of 5-20 μm.
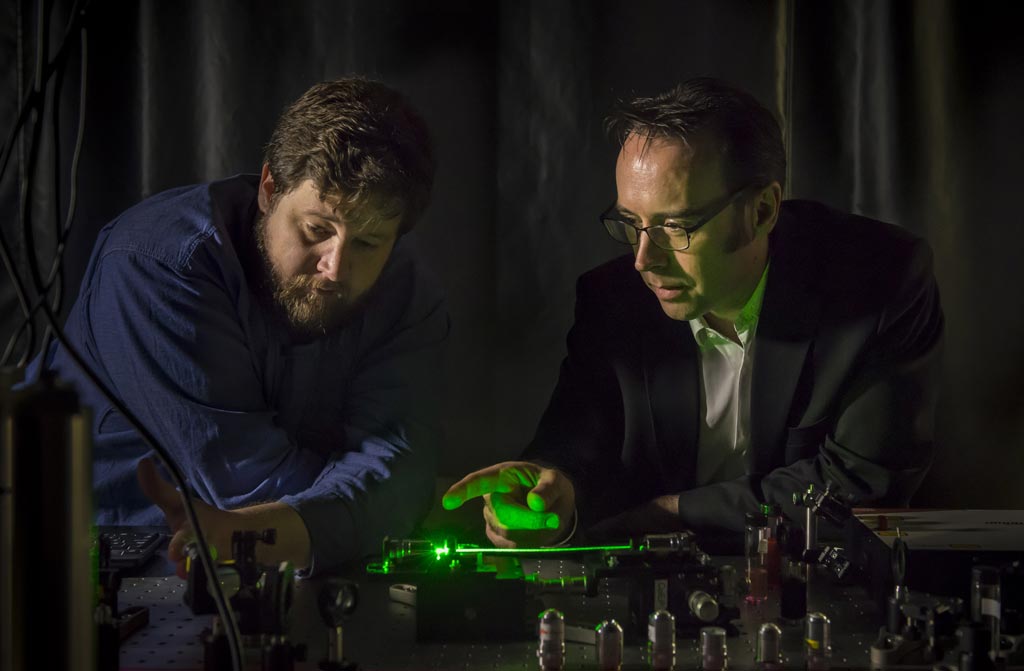
Image: Professor Robert McLaughlin (R) with the smart needle (Photo courtesy University of Adelaide).
The researchers then tested the probe intraoperatively in eleven patients undergoing craniotomy, using it to detect blood vessels at risk of causing intracranial hemorrhage. The probe successfully detected surface blood vessels with a sensitivity of 91.2% and a specificity of 97.7%, and was also able to detect deep cerebral blood vessels. And as OCT is label free, the researchers did not need a contrast agent, relying on endogenous optical scatterers in the tissue. The study was published on December 19, 2018, in Science Advances.
“The fiber-optic camera, the size of a human hair, shines infrared light onto the brain tissue. And the computer system behind the needle identifies the blood vessel and alerts the surgeon,” said senior author Professor Robert McLaughlin, PhD, chair of Biophotonics at the University of Adelaide. “The imaging needle lets surgeons ‘see’ at-risk blood vessels as they insert the needle, allowing them to avoid causing bleeds. This is the first reported use of such a probe in the human brain during live surgery, and is the first step in the long process required to bring new tools like this into clinical practice.”
OCT is based on low-coherence interferometry, typically using NIR light, a relatively long wavelength that allows it to penetrate into the scattering medium. Depending on the properties of the light source, OCT can achieve sub-micrometer resolution. Despite being an echo imaging method (like ultrasound), it is limited to imaging 1-2 mm below the surface in biological tissue, as at greater depths the proportion of light that escapes without scattering is too small to be detected.
Related Links:
University of Adelaide
Sir Charles Gairdner Hospital













.jpg)