Consulting Cardiologists Face an Imaging Paradigm Shift
By MedImaging International staff writers
Posted on 22 Mar 2017
In response to the rapid and unsustainable growth in the use of cardiac imaging procedures, the U.S. Centers for Medicare & Medicaid Service 2017 Medicare Physician Fee Schedule (MPFS) has confirmed the January 1, 2018, deadline for physicians to begin reporting on appropriate use criteria (AUC) interactions in order to receive payment for Medicare advanced imaging, as mandated by the Protecting Access to Medicare Act (PAMA) of 2014.Posted on 22 Mar 2017
The AUC will serve as a guide for physicians to incorporate symptoms, risk factors, and clinical history in selecting the patients for whom testing is most appropriate, based on the best available evidence or expert consensus. AUC will also be part of a patient’s comprehensive disease management plan in order to maximize the value of care by minimizing unnecessary imaging and resultant downstream invasive procedures. It will thus help to avoid excess costs, enhances the value of imaging in risk stratification and decision-making, and reduce radiation risk, particularly in women.
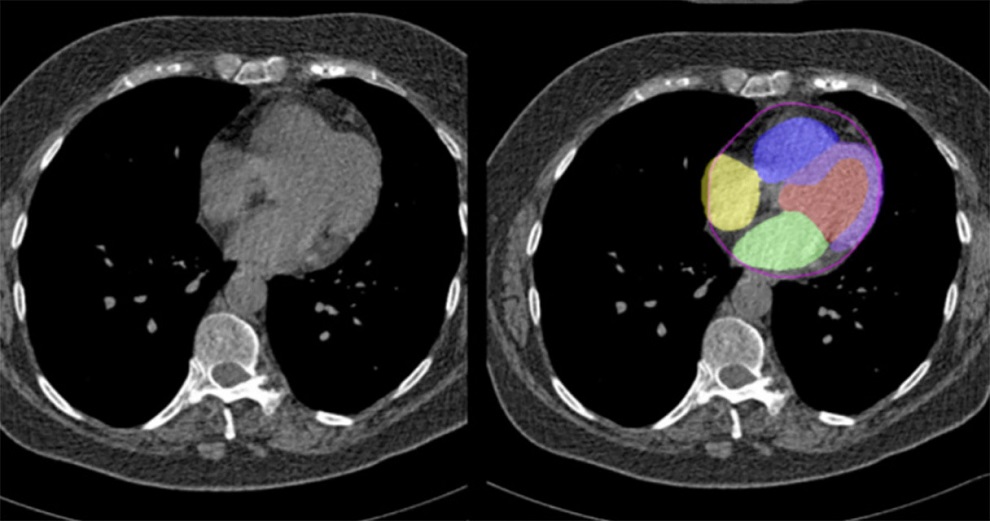
The AUC will help physicians steer patients to alternative tests, or no testing at all, by classifying testing across a range of clinical scenarios in three categories: “appropriate” (established value); “may be appropriate” (uncertain value); and “rarely appropriate” (no clear value). From 2018, physicians will be required to use a clinical decision-support mechanisms (CDSM) for AUC consultation when ordering advanced imaging procedures, such as radionuclide imaging, magnetic resonance imaging (MRI), and computed tomography (CT); but other procedures, such as echocardiography, will be exempt.
“With the PAMA change, a massive shift will occur, wherein the burden of reducing inappropriate use moves largely from payers to providers. Most physicians are unprepared for this paradigm shift,” said Rami Doukky, MD, of John H. Stroger Jr. Hospital (Chicago, IL, USA), and colleagues, in an opinion piece published on February 28, 2017, in Annals of Internal Medicine. “Currently available CDSMs are often disjointed from the care process, and need to be integrated more seamlessly into EHR systems to provide real-time guidance with the least provider burden.”
Professional organizations such as the American College of Cardiology and the American College of Radiology have established multidisciplinary autonomous teams for rigorous, systematic review of published literature and consensus guidelines in order to construct detailed AUCs, with transparency of the methodology supporting appropriate use determination, and full disclosure of potential conflicts of interest. Radiology benefits management programs and insurance companies are specifically excluded from this process.