Portable Ultrasound Tool Uses AI to Detect Arm Fractures More Quickly
Posted on 20 May 2024
Suspected injuries to the upper limbs are a major reason for visits to hospital emergency departments. Currently, wait times for an X-ray and subsequent doctor consultation can vary widely, typically ranging from two to six hours depending on the emergency department's location and workload on any given day. Now, a new portable ultrasound system is set to potentially reduce these wait times and decrease costs in hospital emergency departments.
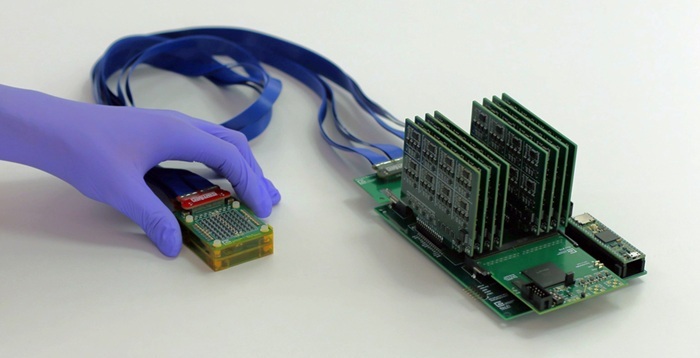
Developed by researchers at the University of Alberta (Edmonton, AB, Canada), the Ultrasound Arm Injury Detection tool leverages artificial intelligence (AI) to enable nurses or primary care physicians to quickly and accurately scan for fractures in the wrist or elbow, or tears in the rotator cuff. This tool allows for the immediate ruling out of fractures, thus decreasing both diagnostic wait times and costs. The innovative system enhances a portable ultrasound device with AI, helping the operator verify the accuracy of the scans and promptly identify the presence of fractures. If a fracture is detected, the patient is then referred for a follow-up X-ray or MRI scan to confirm the diagnosis and outline a treatment plan, which could vary from a simple splint to surgical intervention for more complex injuries.

This tool is designed to be operated by a nurse or physician with minimal training, as opposed to the extensive training required by sonographers or radiologists who typically handle conventional diagnostic imaging devices. The researchers are set to conduct clinical validations of this system with patients in the pediatric emergency departments of two hospitals. Ultrasound technology is fast, safe, and highly sensitive to fractures, particularly suitable for wrist assessments in emergency settings. The researchers also anticipate that the system will be easy to use and well-received by medical staff.
“What happens right now is people have to wait and — depending on which emergency department you go to and how busy they are that day — it could take from two to six hours to have an X-ray and then see the doctor,” said Dr. Abhilash Hareendranathan, assistant professor in the Department of Radiology and Diagnostic Imaging, who developed the system. “With our tool, if you are able to rule out a fracture, that cuts down on the wait time and saves money on the diagnosis.”
Related Links:
University of Alberta