Intraoperative Ultrasound Good for Open, Laparoscopic, and Robotic Surgery
By MedImaging International staff writers
Posted on 23 Mar 2017
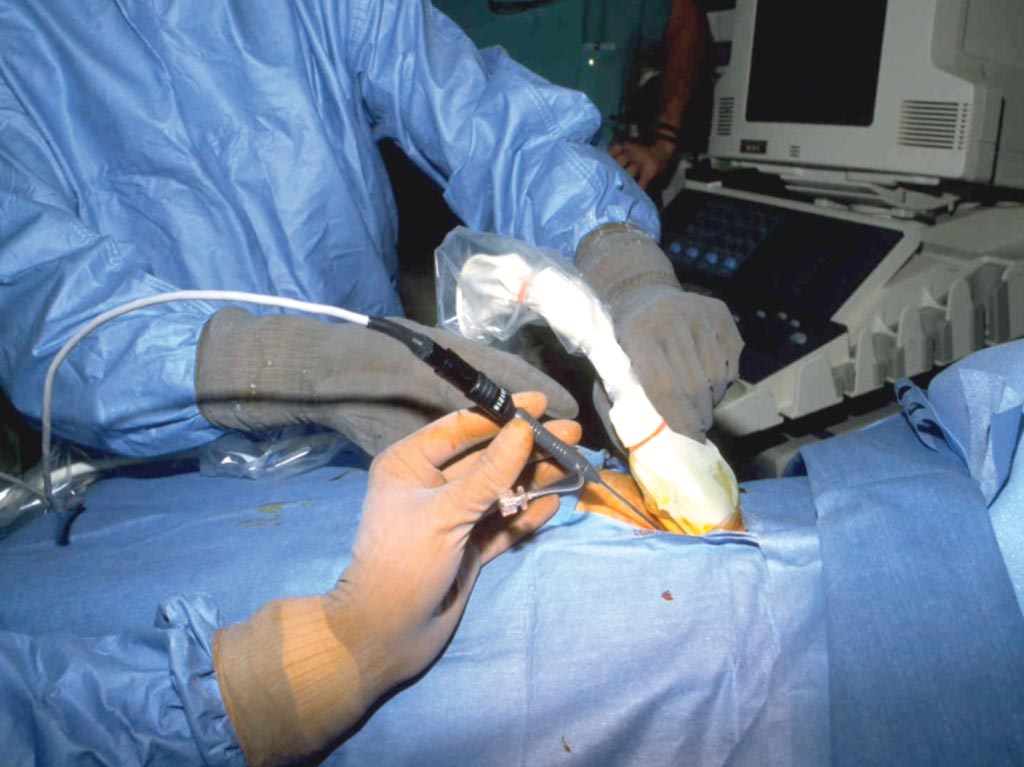
As the only established cross-section imaging tool in the operation room for diagnosis and image-guided treatment, intraoperative ultrasound (IOUS) is honed to the demands of open, laparoscopic, and robotic surgery where continuous monitoring is needed to guide operations and update diagnostic information for the surgical team.Posted on 23 Mar 2017
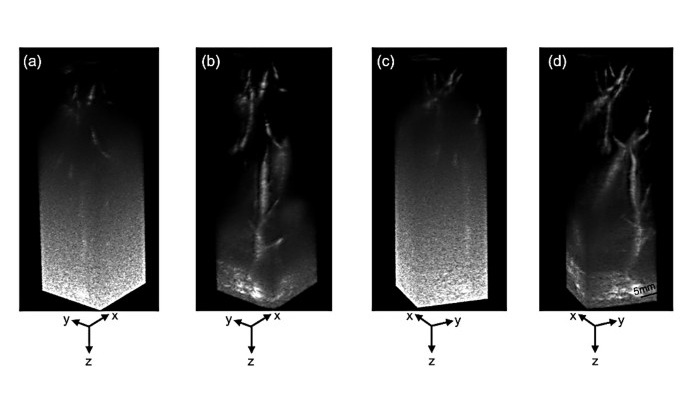
Images provided through IOUS scanning have a limited field of view of the anatomy, but through real-time, high-resolution, and magnification, a diagnosis can be made or confirmed for a pre-surgical impression using a percutaneous scanning approach.
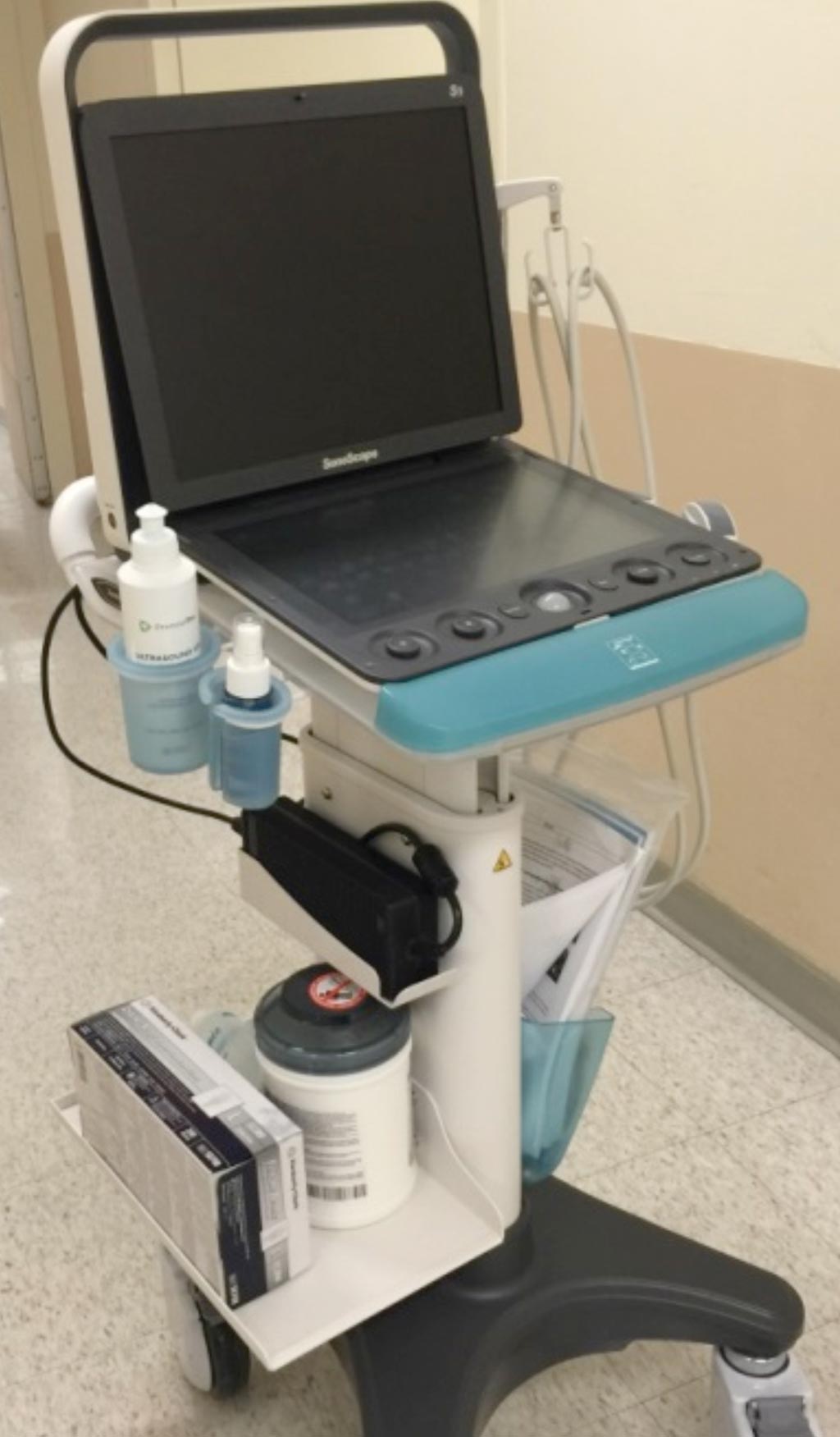
SonoScape produces the S9 portable US unit that can be used intraoperatively. This unit incorporates recent advances in IOUS including broadband transducers with high-resolution imaging and specially designed smaller footprint probes, which enable IOUS to acquire the best possible image within a limited space. In addition, software-driven techniques specifically for US provide better imaging and a greater range of applications than in previous generations.
Dr. Ji-Bin Liu, MD, Professor of Radiology, and Director, Special Training Programs at Jefferson Ultrasound and Radiology Education Institute, Philadelphia, PA, is an expert in the use of IOUS. He points out that current US machines are smaller, more portable and technologically superior. He has recently used the S9 portable US unit from SonoScape for ultrasound-guided research project in the operating room at the Thomas Jefferson University Hospital.
“The use of dynamic scanning techniques with superior imaging quality can overcome any limitation that might be associated with IOUS requiring a small opening and area,” he said, adding that, “If a more complete image of a larger structure is sought, multiple images acquired using IOUS can be combined to create a larger and more complete picture.”
Fewer Artifacts and Spotting Sub-Milliliter Tumors
Unlike conventional pre-surgical imaging, the unique and superior imaging produced by IOUS as used on SonoScape equipment, is associated with fewer artifacts to hinder the image display because the transducer is placed directly on the surface of the organ. By doing so, IOUS visually displaces other organs and avoids bowel gases as well as bone structures.
One of the most common applications of IOUS is in imaging the liver, which is commonly done through open-surgery. Dr. Liu explains that, “When scanning the liver with the transabdominal method, chest ribs and bowel gases can increase the difficulty of seeing it clearly, but with an intraoperative probe it can be placed directly on the liver during open surgery and provide a complete and detailed image of the liver, biliary duct, and pancreas associated with surrounding structures.”
IOUS also facilitates the radiologist and surgeon for answering questions about the tumor during the management of hepatic neoplasms. Because IOUS helps detect exact tumor location, margin, invasion of major blood vessels or not, and feasibility of resection, sub-milliliter tumors and tumor thrombosis in the portal vein to be spotted that could otherwise be missed by transabdominal ultrasound, or other modalities.
Detecting tumors that are often missed has particular relevance to pancreatic tumors that can be late to show symptoms, grow rapidly and be too deep for transabdominal US transducers to image. These tumors also prove difficult to confirm for resection by pre-surgical scanning, however, IOUS provides a means of determining if the tumor resection is possible or whether it has invaded a major blood vessel, aiding decision-making.
Another application of IOUS that can be used on SonoScape’s equipment is in detecting tumor thrombosis in the portal vein, which could be missed by other modalities and transabdominal US. Detection of such tumors by IOUS would change the operation procedure and prognosis, Dr. Liu pointed out.
“For example, if a tumor thrombosis of the vessels is detected, it implies that the tumor has already spread through that blood vessel to another location, increasing the staging for that tumor,” he said.
Likewise, efficient detection can ensure resection is confined to tumor and not healthy tissue. Renal tumors may have multiple focal lesions that can be small and subcapsular, and due to tumor location, damage to the kidney during partial nephrectomy is a real concern. “IOUS, mitigates this fear significantly by accurately localizing tumor for resection,” he added.
As minimally invasive procedures become more commonplace, laparoscopic IOUS is made possible with specially designed transducers that are both rigid and flexible. Although the probe is harder to maneuver once inside the body cavities, this method provides the same imaging capabilities as open-surgery IOUS and is minimally invasive for the patient as an important benefit.
Finally, considerable advances are being made with IOUS being introduced into robotic surgery and sharing the same benefits as seen in laparoscopic and open surgery. Robotic surgery is now at the point where small, highly manipulative and specialized instruments can be inserted into the operational field including use of a robotic US probe. This technique using smaller, robotically controlled instruments offers a less invasive procedure for the patient with more accuracy and capabilities by these. The Thomas Jefferson University Hospital has successfully applied robotic ultrasound in robotic surgery during partial nephrectomy. “No doubt, we will see the continued evolution and development of IOUS in surgical applications for the ultimate goal of improving patient care,” Dr. Liu commented.